Neuropathy Neuropathy Leprosy is a nerve pathology presenting with sensory Sensory Neurons which conduct nerve impulses to the central nervous system. Nervous System: Histology, motor Motor Neurons which send impulses peripherally to activate muscles or secretory cells. Nervous System: Histology, or autonomic impairment secondary to dysfunction of the affected nerve. The peripheral nerves Peripheral Nerves The nerves outside of the brain and spinal cord, including the autonomic, cranial, and spinal nerves. Peripheral nerves contain non-neuronal cells and connective tissue as well as axons. The connective tissue layers include, from the outside to the inside, the epineurium, the perineurium, and the endoneurium. Nervous System: Histology (outside the brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification and spinal cord Spinal cord The spinal cord is the major conduction pathway connecting the brain to the body; it is part of the CNS. In cross section, the spinal cord is divided into an H-shaped area of gray matter (consisting of synapsing neuronal cell bodies) and a surrounding area of white matter (consisting of ascending and descending tracts of myelinated axons). Spinal Cord: Anatomy), are derived from several plexuses, with the brachial and lumbosacral plexuses supplying the major innervation to the extremities. Mononeuropathy (affecting a single nerve) and plexopathy (affecting the plexus) can occur from trauma, compression Compression Blunt Chest Trauma, and systemic diseases. The clinical presentation varies according to location, type of nerves affected, and cause of the damage. Diagnosis requires a thorough physical examination, and diagnostic tests Diagnostic tests Diagnostic tests are important aspects in making a diagnosis. Some of the most important epidemiological values of diagnostic tests include sensitivity and specificity, false positives and false negatives, positive and negative predictive values, likelihood ratios, and pre-test and post-test probabilities. Epidemiological Values of Diagnostic Tests include laboratory tests, imaging and a confirmatory nerve conduction study Nerve Conduction Study Motor Neuron Lesions, and electromyography Electromyography Recording of the changes in electric potential of muscle by means of surface or needle electrodes. Becker Muscular Dystrophy. Management depends on the etiology but centers around physical therapy Physical Therapy Becker Muscular Dystrophy, supportive care, and treatment of underlying issues.
Last updated: Jan 12, 2024
Neuropathy Neuropathy Leprosy is a term used to describe nerve pathology presenting with sensory Sensory Neurons which conduct nerve impulses to the central nervous system. Nervous System: Histology, motor Motor Neurons which send impulses peripherally to activate muscles or secretory cells. Nervous System: Histology, or autonomic impairment secondary to dysfunction of the affected nerve.
There are numerous etiologies for mononeuropathy, which can be acute or chronic.
Neuropathies Neuropathies Chédiak-Higashi Syndrome in the upper extremities can affect the brachial plexus Brachial Plexus The large network of nerve fibers which distributes the innervation of the upper extremity. The brachial plexus extends from the neck into the axilla. In humans, the nerves of the plexus usually originate from the lower cervical and the first thoracic spinal cord segments (c5-c8 and T1), but variations are not uncommon. Peripheral Nerve Injuries in the Cervicothoracic Region (causing brachial plexopathy) or the individual nerves that branch off to supply different areas.
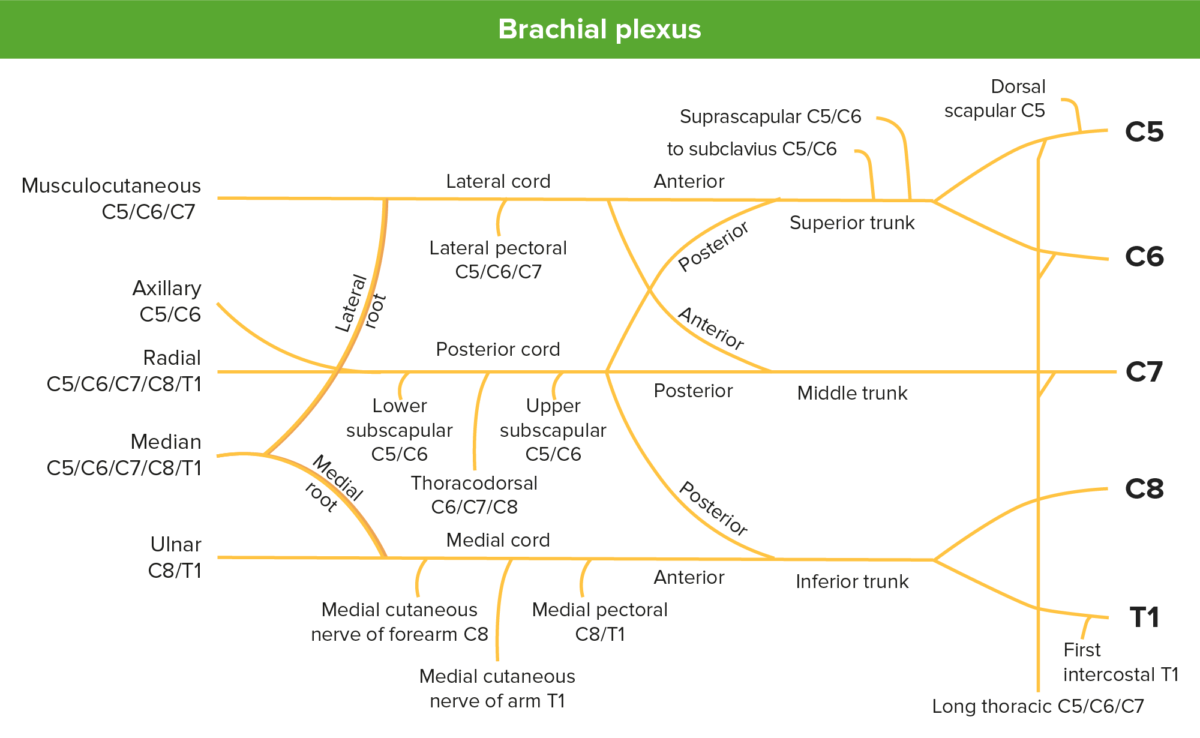
Image depicting the brachial plexus and its branches
Image by Lecturio.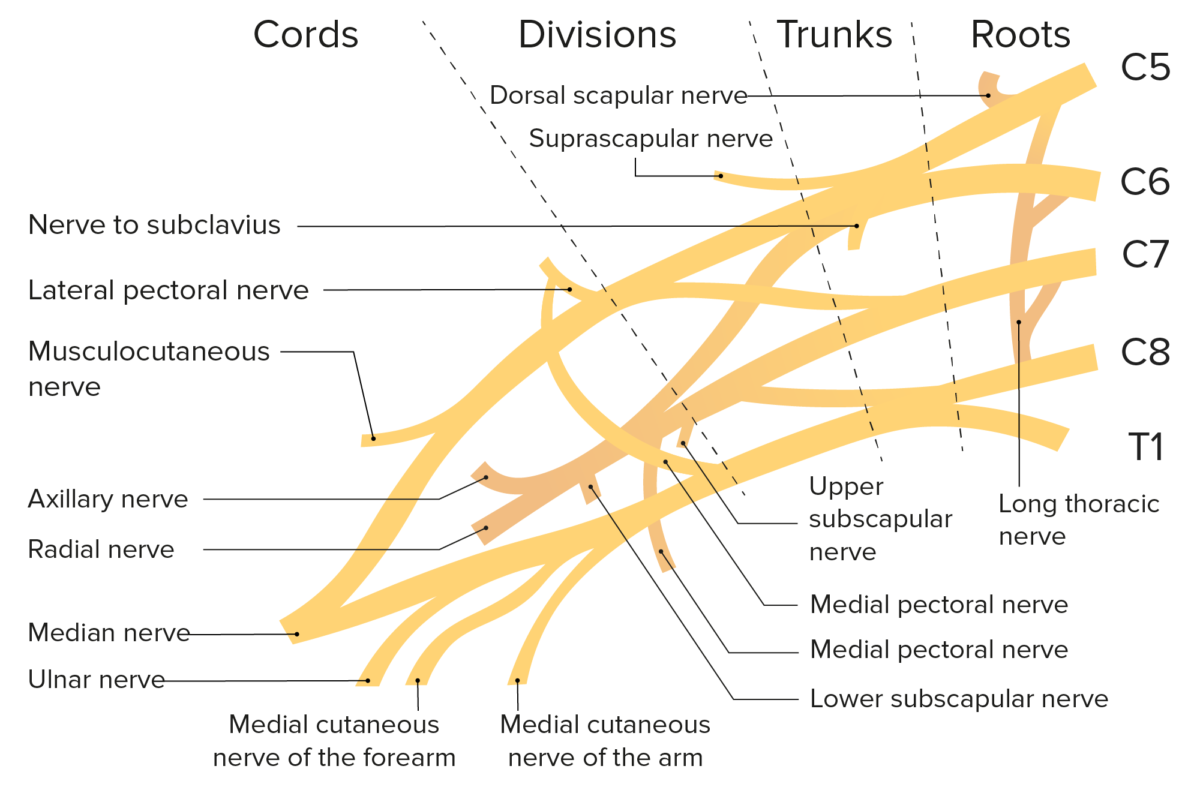
Schematic of the brachial plexus and the branches of the brachial plexus
Image by Lecturio.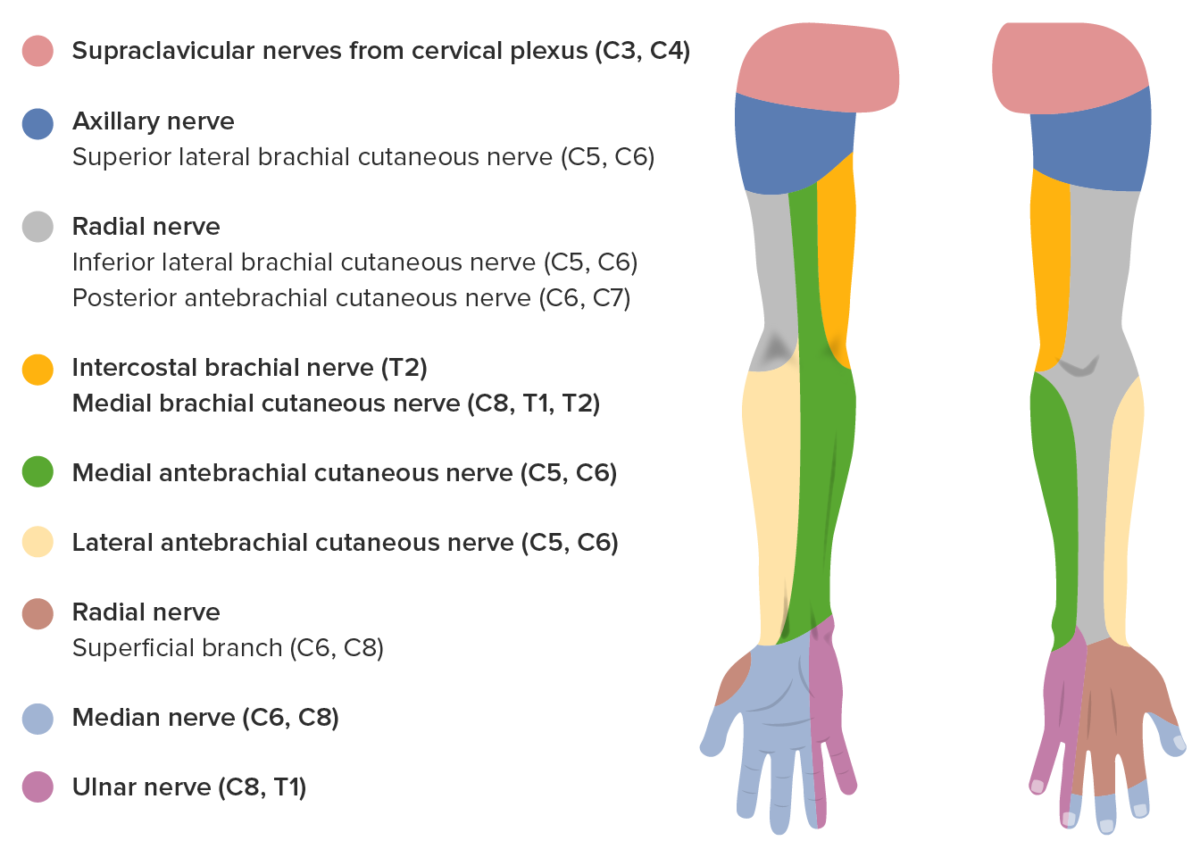
Sensory innervation of the upper extremity
Image by Lecturio.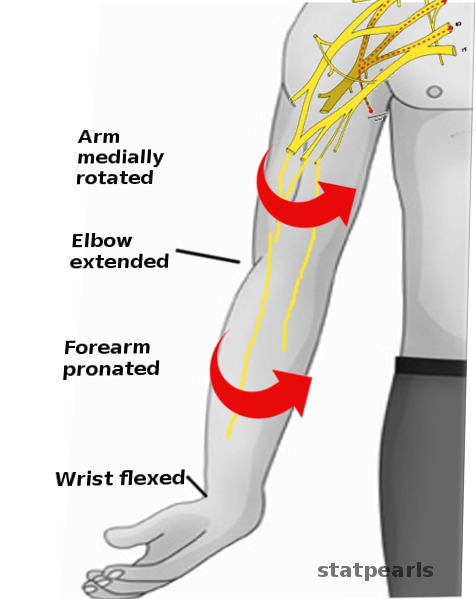
Waiter’s tip posture (Erb palsy)
Image: “Erb palsy-Physical exam” by S. Bhimji, MD. License: CC BY 4.0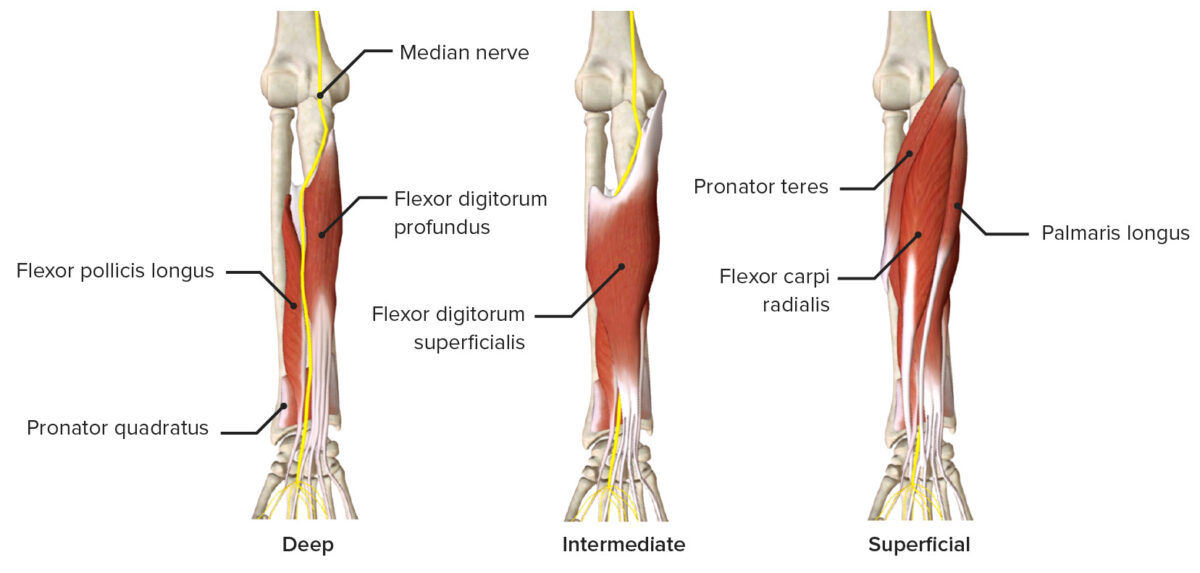
Median nerve as it passes through the various layers of the anterior forearm, featuring the muscles it innervates
Image by BioDigital, edited by Lecturio.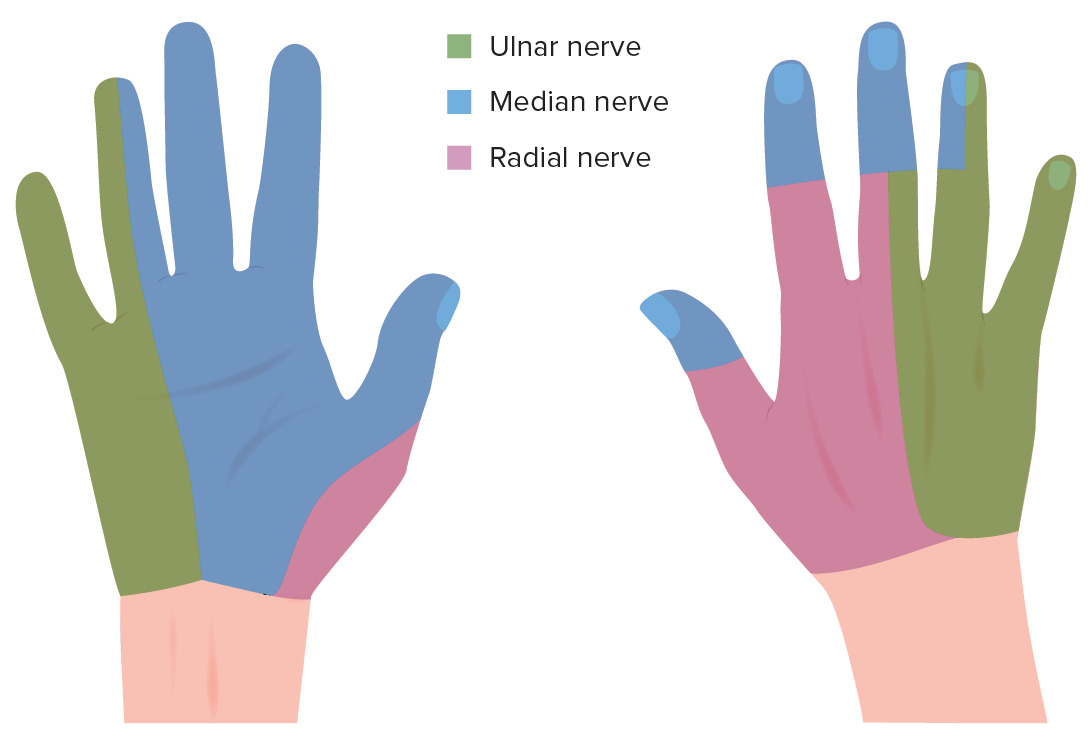
Sensory innervation of the hand:
Left image is volar aspect and right image is the dorsal aspect.
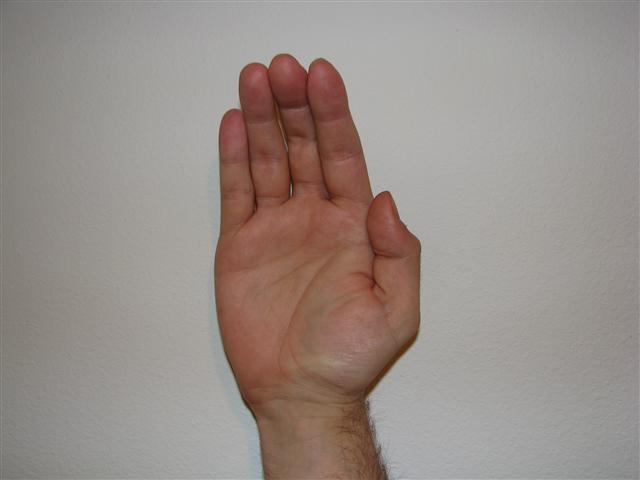
Ape-hand deformity
Image: “Ape Hand Deformity” by Emily Barrett. License: CC BY 3.0
Hand of benediction
Image: “Benediction Hand” by Katherine Humphries. License: CC BY 4.0| Ulnar claw | Hand Hand The hand constitutes the distal part of the upper limb and provides the fine, precise movements needed in activities of daily living. It consists of 5 metacarpal bones and 14 phalanges, as well as numerous muscles innervated by the median and ulnar nerves. Hand: Anatomy of benediction | |
|---|---|---|
| Nerve | Ulnar nerve Ulnar Nerve A major nerve of the upper extremity. In humans, the fibers of the ulnar nerve originate in the lower cervical and upper thoracic spinal cord (usually C7 to T1), travel via the medial cord of the brachial plexus, and supply sensory and motor innervation to parts of the hand and forearm. Axilla and Brachial Plexus: Anatomy (wrist area) | Median nerve Median Nerve A major nerve of the upper extremity. In humans, the fibers of the median nerve originate in the lower cervical and upper thoracic spinal cord (usually C6 to T1), travel via the brachial plexus, and supply sensory and motor innervation to parts of the forearm and hand. Cubital Fossa: Anatomy (wrist/elbow) |
| Presentation | Clawing when asked to extend the fingers | Hand Hand The hand constitutes the distal part of the upper limb and provides the fine, precise movements needed in activities of daily living. It consists of 5 metacarpal bones and 14 phalanges, as well as numerous muscles innervated by the median and ulnar nerves. Hand: Anatomy of benediction when asked to make a fist (but can extend fingers) |
| Affected fingers | 4th and 5th fingers extended at MCP joints and flexed at IP joints | 2nd and 3rd fingers |
| Mechanism |
|
Loss of motor Motor Neurons which send impulses peripherally to activate muscles or secretory cells. Nervous System: Histology function of the 2nd and 3rd fingers |
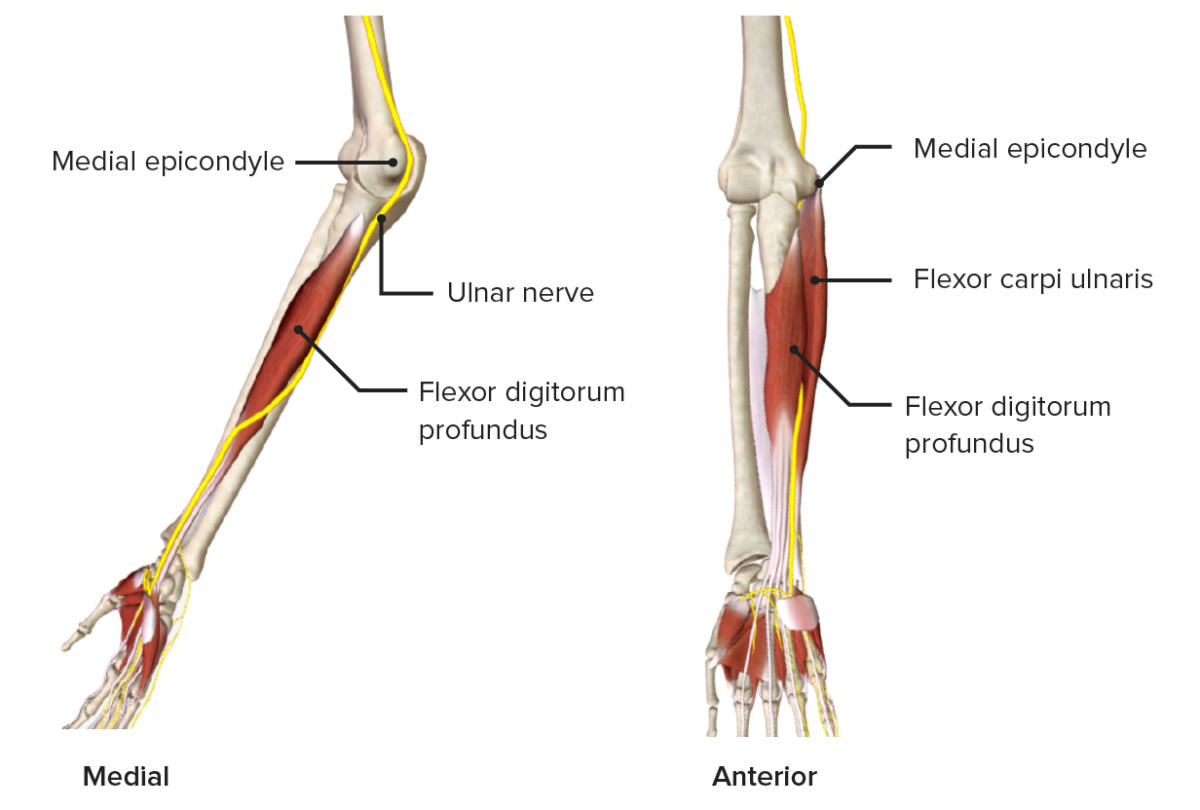
Ulnar nerve as it passes through the medial aspect of the forearm
Image by BioDigital, edited by Lecturio.
Ulnar claw:
The metacarpophalangeal joints of the 4th and 5th fingers are extended and the interphalangeal joints of the same fingers are flexed.
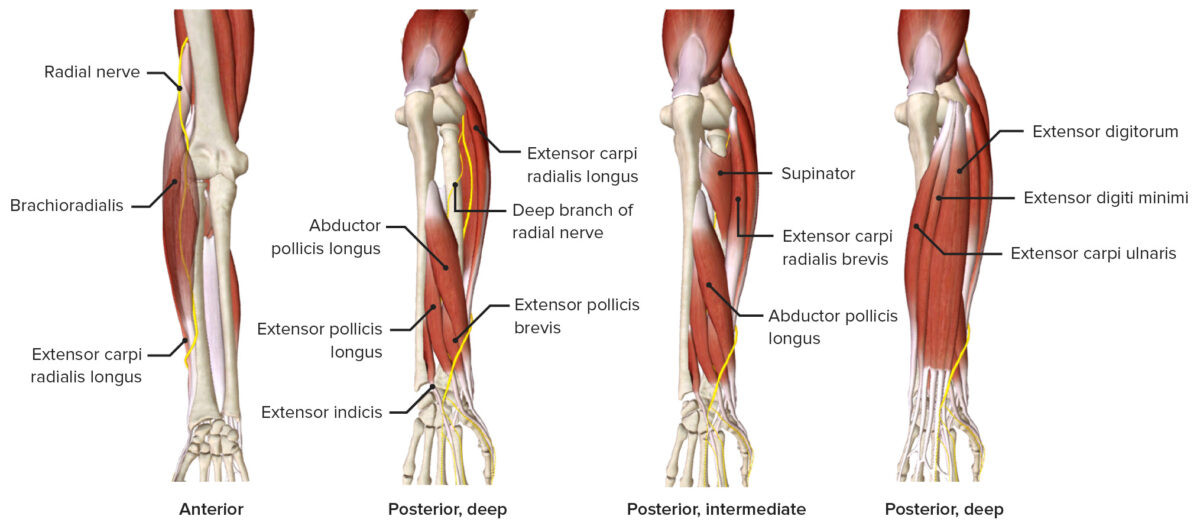
Radial nerve as it passes through the forearm, featuring the muscles it innervates (mainly posterior compartment)
Image by BioDigital, edited by Lecturio.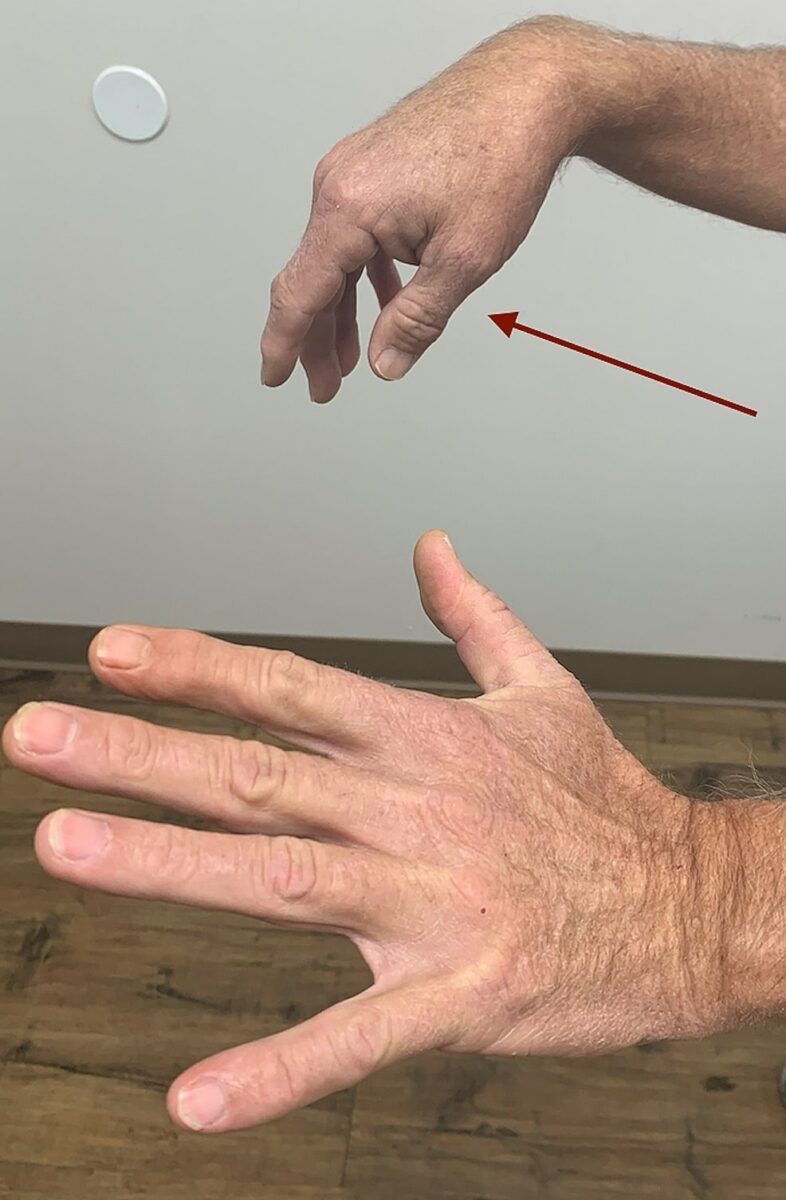
Wrist drop (radial nerve palsy)
Image: “Right wrist, finger, and thumb drop (red arrow)” by Hassan Kesserwani. License: CC BY 4.0
Spinal accessory nerve palsy:
Frontal view (left) demonstrating the right neck asymmetry and ipsilateral shoulder depression. Dorsal view (right) showing that the right scapula’s medial wall (red line) is translated laterally, as it is evident with its increased distance from the body’s midline (black line). Arrow points to the drooping shoulder.
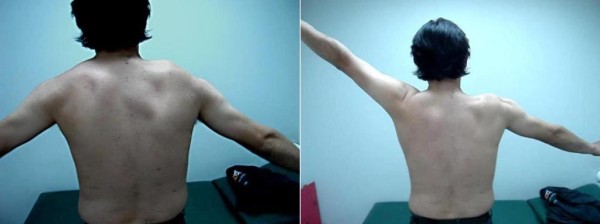
Spinal accessory nerve palsy:
Scapular winging at different angles of arm abduction
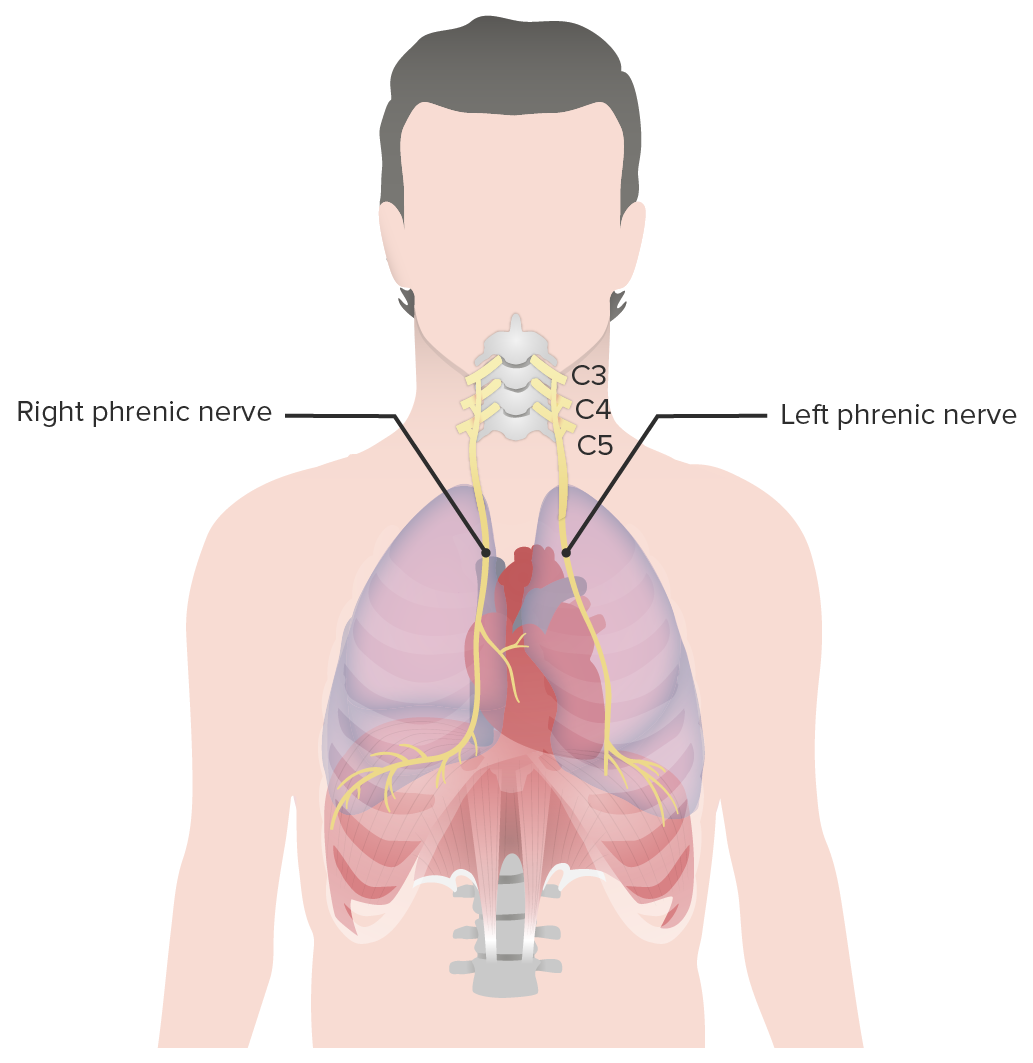
Phrenic nerves:
The left and right phrenic nerves provide innervation to the diaphragm.
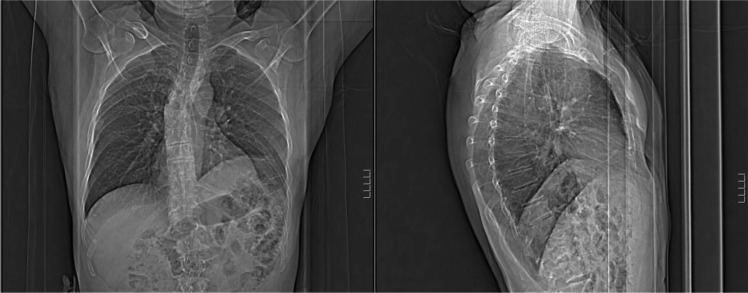
Phrenic nerve injury:
Elevated left hemidiaphragm is noted on chest X-ray.
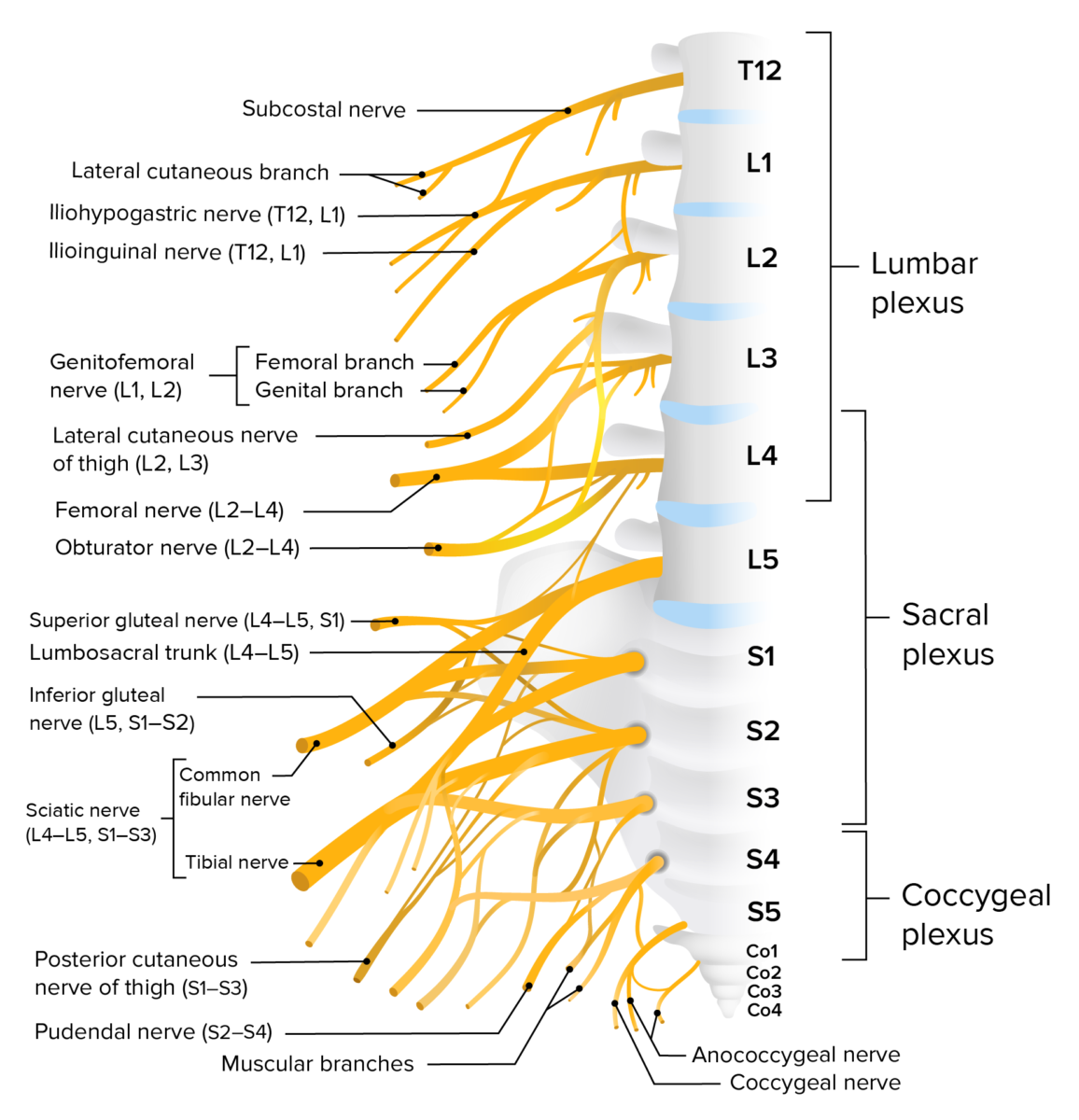
Lumbosacral plexus
Image by Lecturio.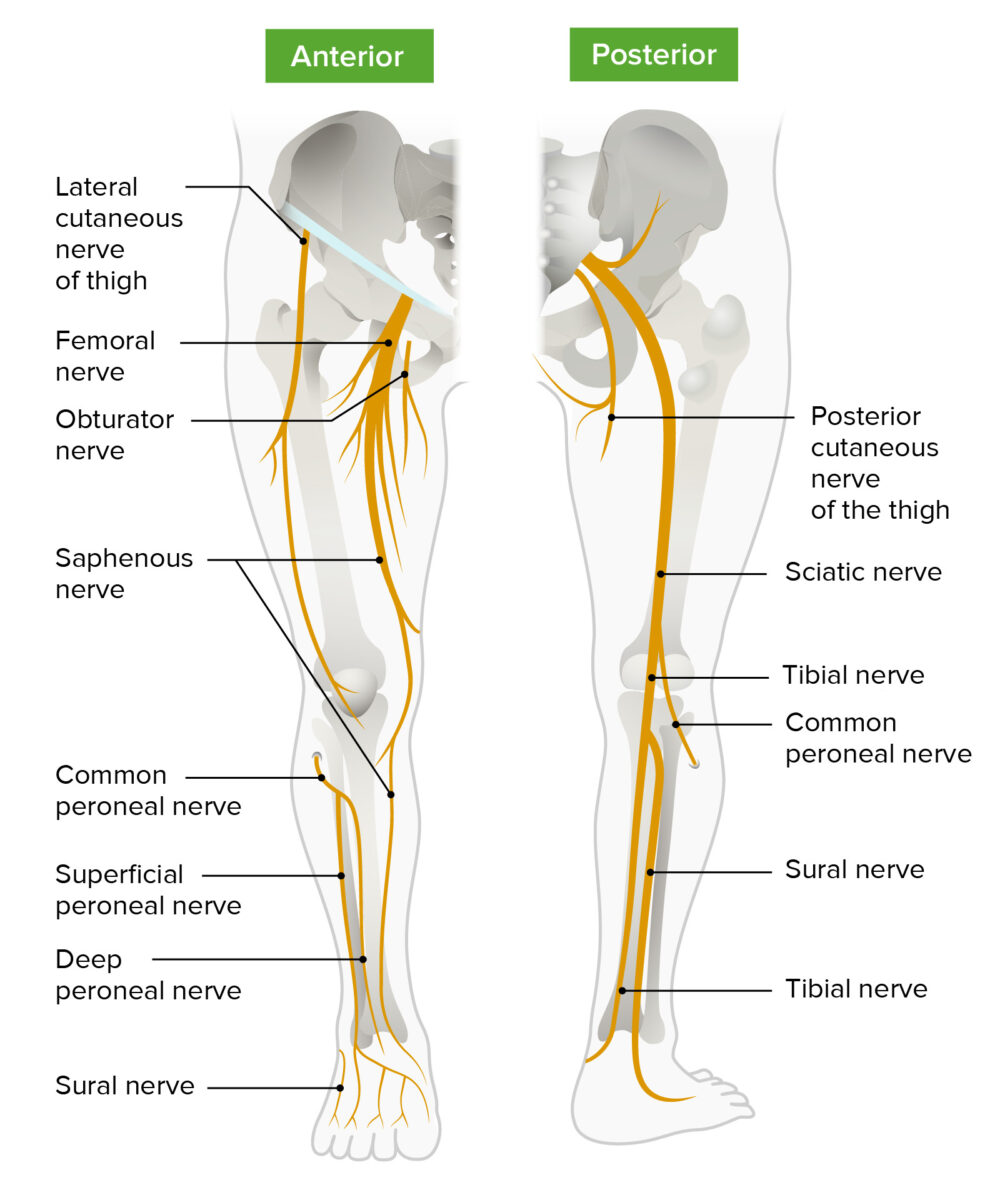
Schematic diagram of the course and main branches of the lumbosacral plexus that innervate the lower limbs
Image by Lecturio.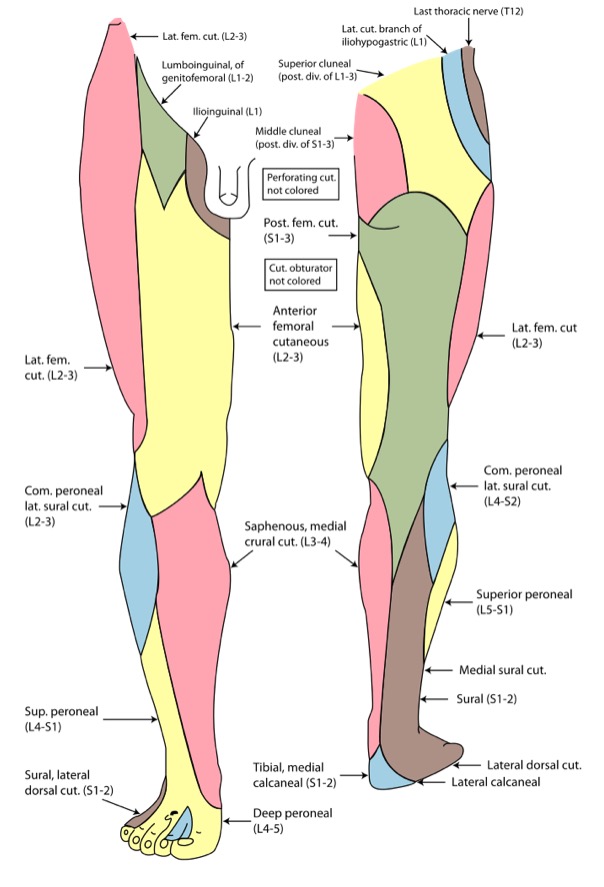
Cutaneous innervation of the lower limb
Image: “Gray826and831” by Henry Vandyke Carter. License: Public Domain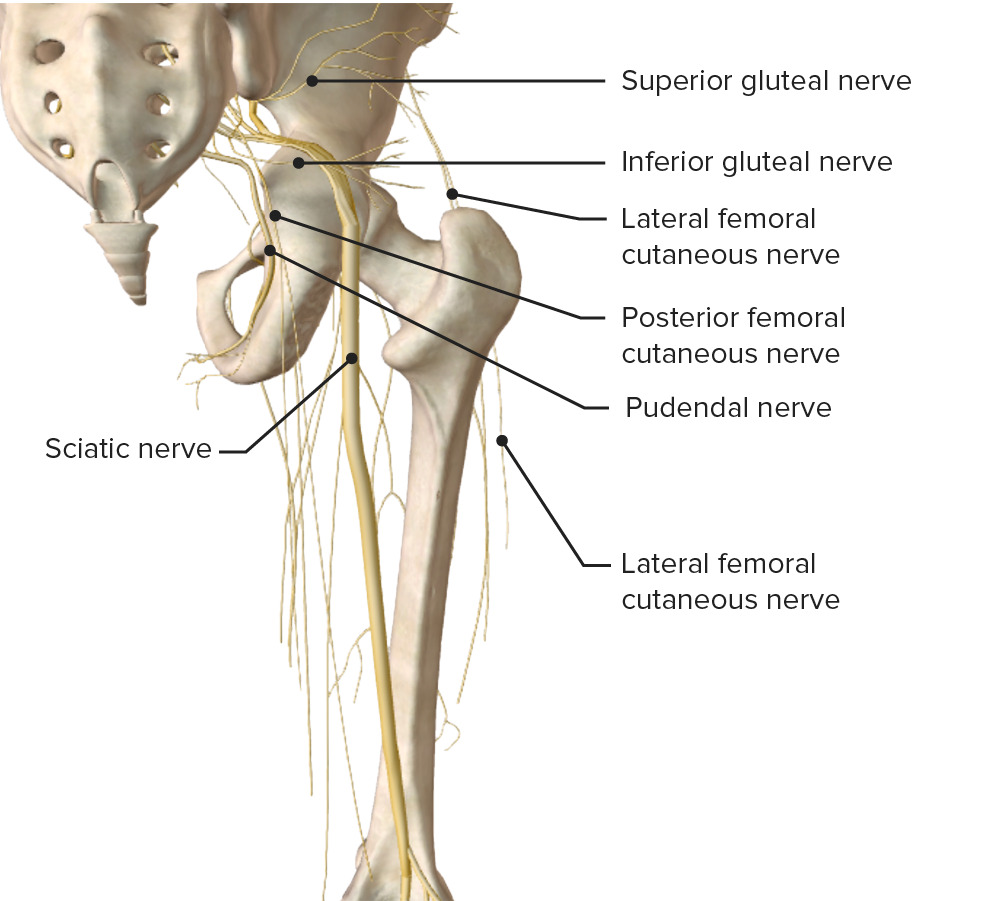
Schematic diagram of the course and main branches of the lumbosacral plexus
Image by BioDigital, edited by Lecturio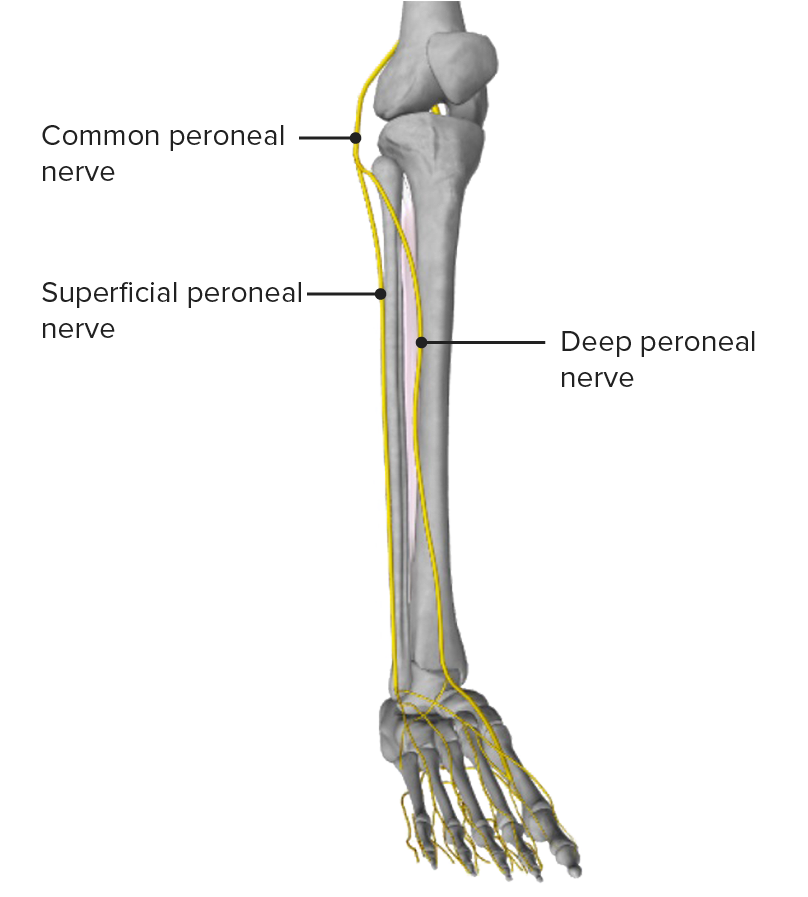
Anterior view of the leg, featuring the common peroneal nerve and its main branches
Image by BioDigital, edited by Lecturio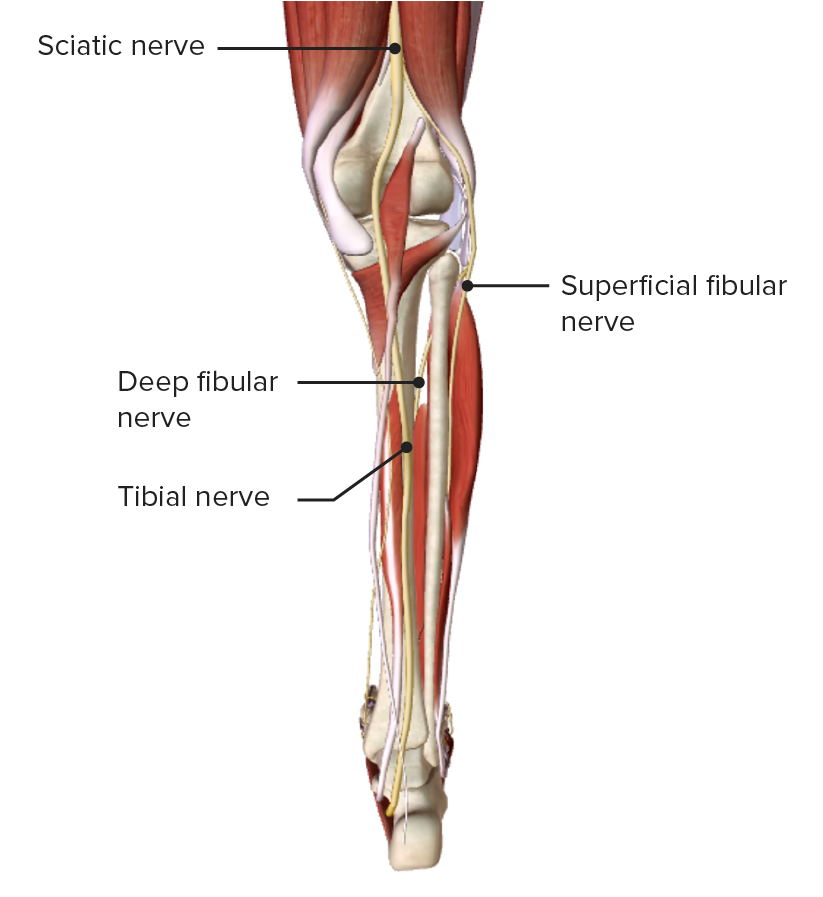
Posterior view of the leg, featuring the tibial nerve as it passes through the medial aspect of the popliteal fossa
Image by BioDigital, edited by Lecturio
Carpal tunnel splint:
A wrist splint is often used in individuals with carpal tunnel syndrome.