Macrolides and ketolides are antibiotics that inhibit bacterial protein synthesis Synthesis Polymerase Chain Reaction (PCR) by binding to the 50S ribosomal subunit and blocking transpeptidation Transpeptidation Lincosamides. These antibiotics have a broad spectrum of antimicrobial activity but are best known for their coverage of atypical microorganisms. Common macrolides are erythromycin, clarithromycin, azithromycin, and fidaxomicin. Side effects include GI upset, QT prolongation, and hepatotoxicity Hepatotoxicity Acetaminophen. Resistance Resistance Physiologically, the opposition to flow of air caused by the forces of friction. As a part of pulmonary function testing, it is the ratio of driving pressure to the rate of air flow. Ventilation: Mechanics of Breathing mechanisms include ribosomal methylation Methylation Addition of methyl groups. In histo-chemistry methylation is used to esterify carboxyl groups and remove sulfate groups by treating tissue sections with hot methanol in the presence of hydrochloric acid. . Glucocorticoids or mutation Mutation Genetic mutations are errors in DNA that can cause protein misfolding and dysfunction. There are various types of mutations, including chromosomal, point, frameshift, and expansion mutations. Types of Mutations, inactivation of the drug through enzyme production, or removal of the drug through efflux pumps Efflux Pumps Lincosamides.
Last updated: Dec 15, 2025
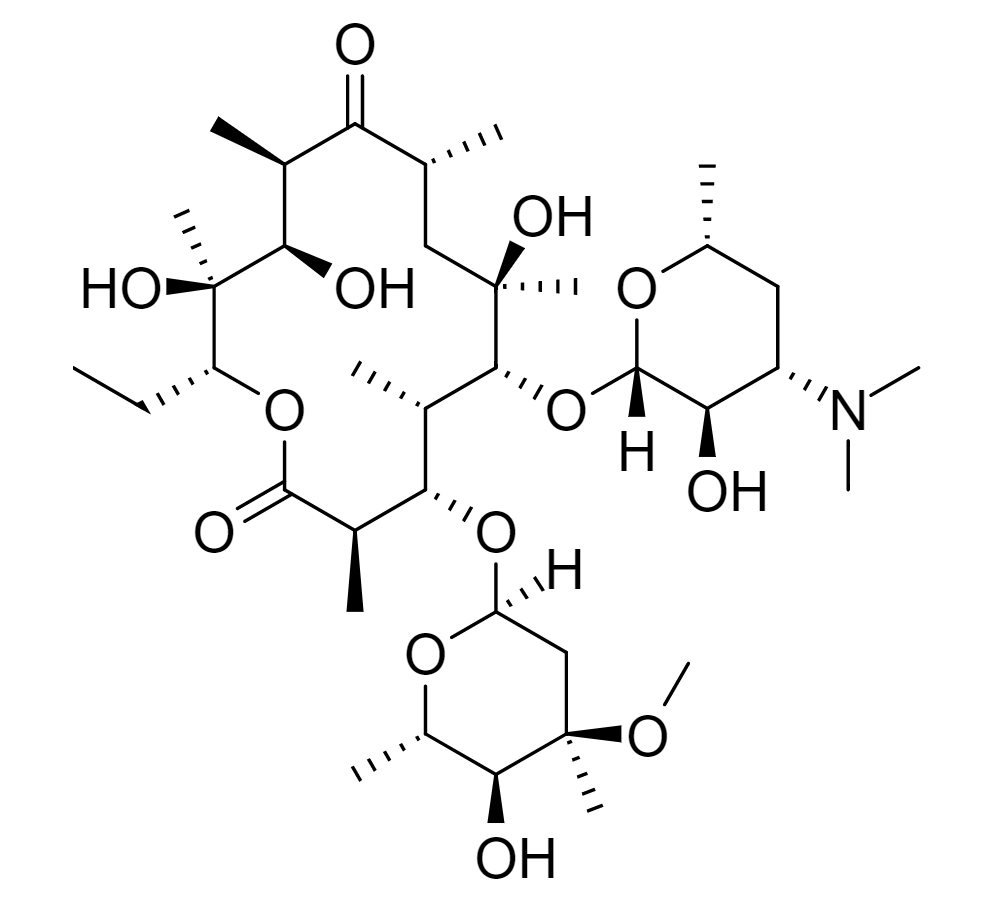
Chemical structure of erythromycin (the prototype drug of the macrolide class), featuring a macrocyclic lactone ring with 2 sugars attached
Image: “Erythromycin” by Edgar181. License: Public Domain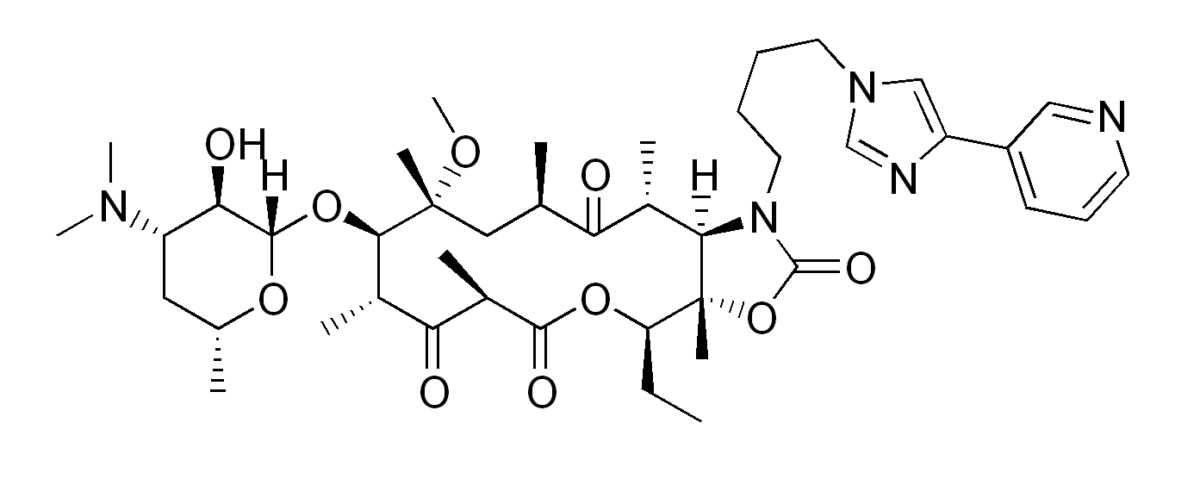
The chemical structure of telithromycin (a ketolide):
Notice the similar structure to erythromycin, with a keto group replacing a sugar.
General:
Fidaxomicin is an exception:
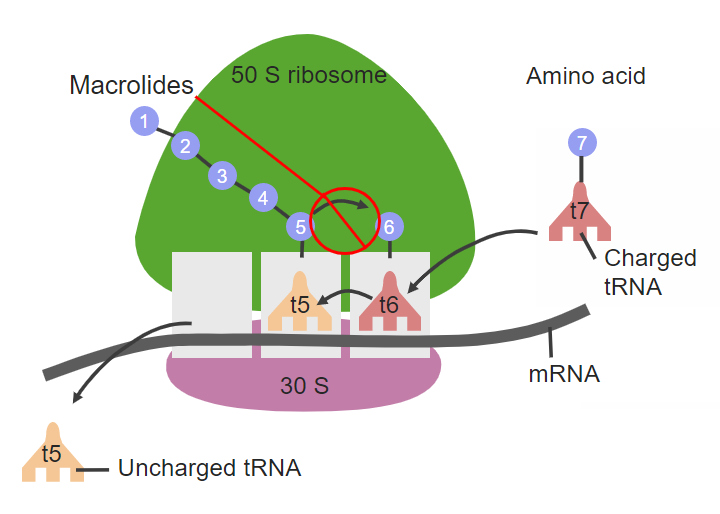
The site of action for macrolides on the 50S ribosomal subunit
tRNA: transfer RNA
mRNA: messenger RNA
| Macrolides | Ketolides | |
|---|---|---|
| Absorption Absorption Absorption involves the uptake of nutrient molecules and their transfer from the lumen of the GI tract across the enterocytes and into the interstitial space, where they can be taken up in the venous or lymphatic circulation. Digestion and Absorption | Erythromycin:
|
Rapid absorption Absorption Absorption involves the uptake of nutrient molecules and their transfer from the lumen of the GI tract across the enterocytes and into the interstitial space, where they can be taken up in the venous or lymphatic circulation. Digestion and Absorption |
| Distribution |
|
|
| Metabolism |
|
|
| Excretion |
|
|
There are 3 methods of resistance Resistance Physiologically, the opposition to flow of air caused by the forces of friction. As a part of pulmonary function testing, it is the ratio of driving pressure to the rate of air flow. Ventilation: Mechanics of Breathing to macrolides:
| Drug class | Mechanism of action | Coverage | Adverse effects |
|---|---|---|---|
| Amphenicols |
|
|
|
| Lincosamides Lincosamides The lincosamides, lincomycin and clindamycin, are inhibitors of bacterial protein synthesis. Drugs in this class share the same binding site as that of macrolides and amphenicols; however, they differ in chemical structure. Lincosamides target the 50S ribosomal subunit and interfere with transpeptidation. Lincosamides |
|
|
|
| Macrolides |
|
|
|
| Oxazolidinones Oxazolidinones The oxazolidinones (linezolid and tedizolid) are bacterial protein synthesis inhibitors. Their unique binding site on the 23S ribosomal RNA of the 50S ribosome gives them zero cross-resistance with other antibiotics. Oxazolidinones |
|
Gram-positive
Gram-Positive
Penicillins
cocci
Cocci
Bacteriology:
|
|
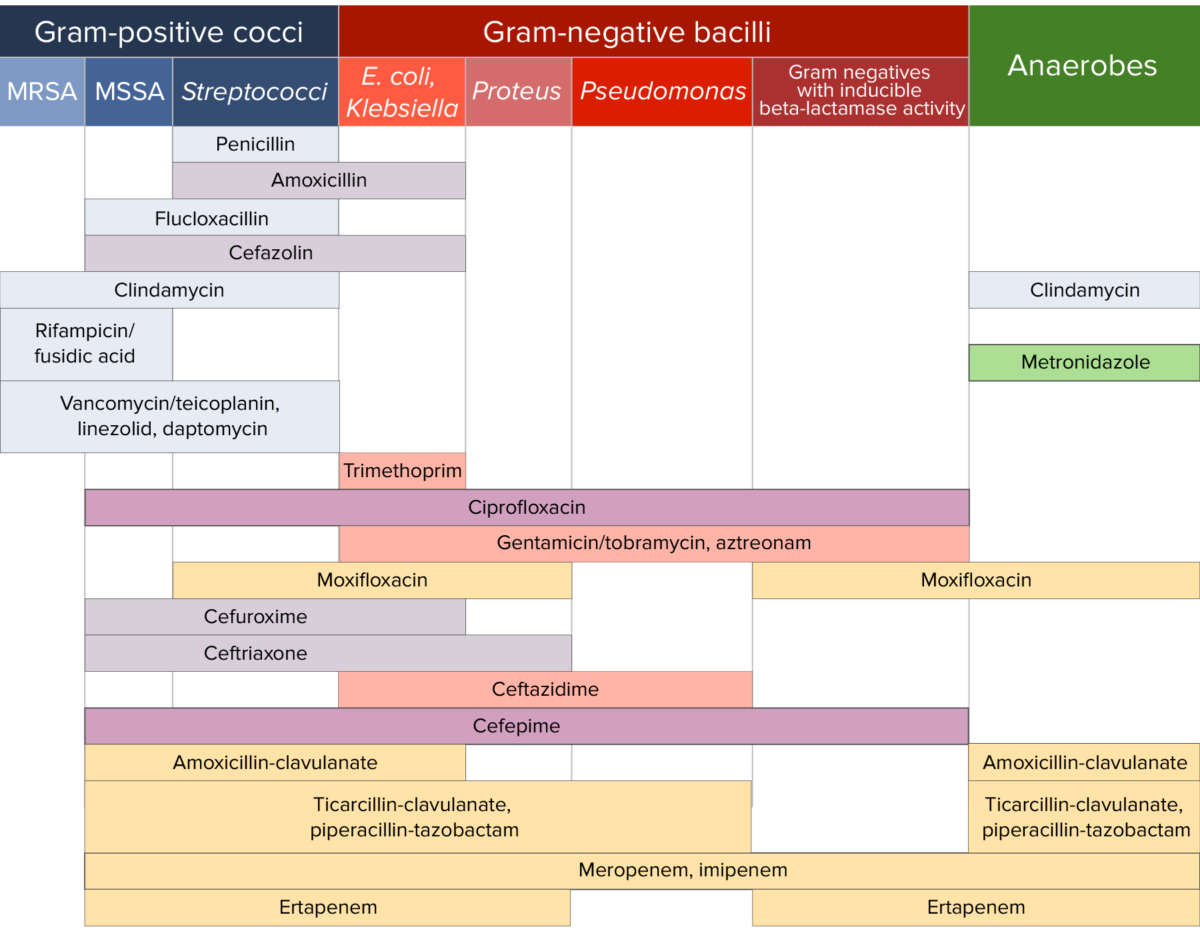
Antibiotic sensitivity:
Chart comparing the microbial coverage of different antibiotics for gram-positive cocci, gram-negative bacilli, and anaerobes.