Legionella is a facultative intracellular Facultative intracellular Yersinia spp./Yersiniosis, gram-negative bacilli Bacilli Shigella. Legionella does not grow on common culture media because it requires certain supplementation ( cysteine Cysteine A thiol-containing non-essential amino acid that is oxidized to form cystine. Synthesis of Nonessential Amino Acids and iron Iron A metallic element with atomic symbol fe, atomic number 26, and atomic weight 55. 85. It is an essential constituent of hemoglobins; cytochromes; and iron-binding proteins. It plays a role in cellular redox reactions and in the transport of oxygen. Trace Elements). Legionella can be isolated on a buffered charcoal Charcoal An amorphous form of carbon prepared from the incomplete combustion of animal or vegetable matter, e.g., wood. The activated form of charcoal is used in the treatment of poisoning. Antidotes of Common Poisonings yeast Yeast A general term for single-celled rounded fungi that reproduce by budding. Brewers' and bakers' yeasts are saccharomyces cerevisiae; therapeutic dried yeast is yeast, dried. Mycology extract (BCYE) medium. The habitat for Legionella is aquatic systems including human-constructed reservoirs, such as cooling towers and hot water tanks. Transmission occurs primarily through inhalation of aerosolized water droplets Droplets Varicella-Zoster Virus/Chickenpox, causing pulmonary infection. Legionella pneumophila (L. pneumophila) accounts for the majority of human infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease. The clinical presentation includes Legionnaires’ disease, atypical pneumonia Atypical pneumonia Mycoplasma, and Pontiac fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever. Diagnosis is by culture, urine antigen Antigen Substances that are recognized by the immune system and induce an immune reaction. Vaccination test, and/or polymerase chain reaction Polymerase chain reaction Polymerase chain reaction (PCR) is a technique that amplifies DNA fragments exponentially for analysis. The process is highly specific, allowing for the targeting of specific genomic sequences, even with minuscule sample amounts. The PCR cycles multiple times through 3 phases: denaturation of the template DNA, annealing of a specific primer to the individual DNA strands, and synthesis/elongation of new DNA molecules. Polymerase Chain Reaction (PCR) ( PCR PCR Polymerase chain reaction (PCR) is a technique that amplifies DNA fragments exponentially for analysis. The process is highly specific, allowing for the targeting of specific genomic sequences, even with minuscule sample amounts. The PCR cycles multiple times through 3 phases: denaturation of the template DNA, annealing of a specific primer to the individual DNA strands, and synthesis/elongation of new DNA molecules. Polymerase Chain Reaction (PCR)). Fluoroquinolones Fluoroquinolones Fluoroquinolones are a group of broad-spectrum, bactericidal antibiotics inhibiting bacterial DNA replication. Fluoroquinolones cover gram-negative, anaerobic, and atypical organisms, as well as some gram-positive and multidrug-resistant (MDR) organisms. Fluoroquinolones and macrolides Macrolides Macrolides and ketolides are antibiotics that inhibit bacterial protein synthesis by binding to the 50S ribosomal subunit and blocking transpeptidation. These antibiotics have a broad spectrum of antimicrobial activity but are best known for their coverage of atypical microorganisms. Macrolides and Ketolides are the main treatments.
Last updated: Dec 15, 2025
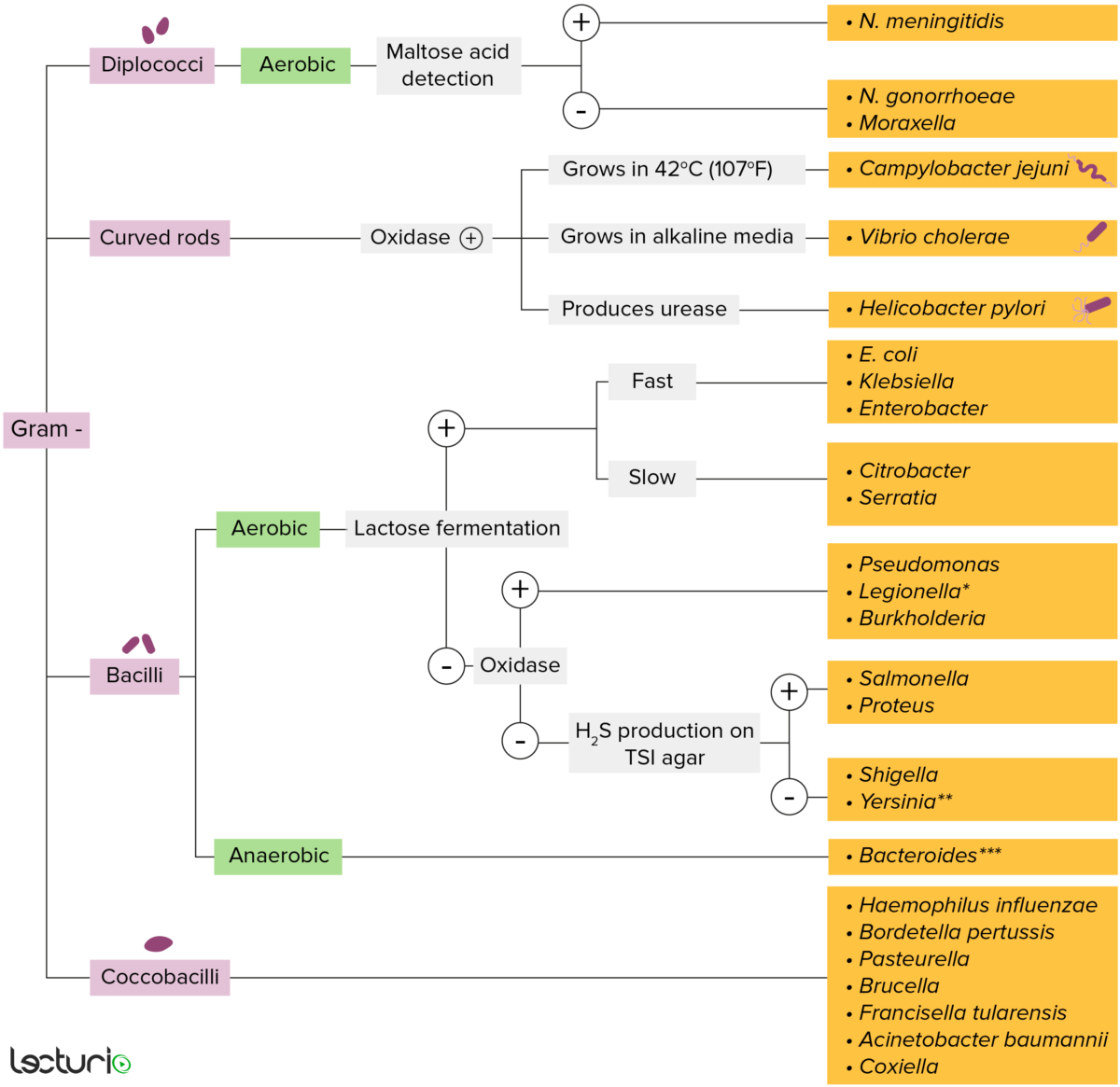
Gram-negative bacteria:
Most bacteria can be classified according to a lab procedure called Gram staining.
Bacteria with cell walls that have a thin layer of peptidoglycan do not retain the crystal violet stain utilized in Gram staining. These bacteria do, however, retain the safranin counterstain and thus appear as pinkish-red on the stain, making them gram negative. These bacteria can be further classified according to morphology (diplococci, curved rods, bacilli, and coccobacilli) and their ability to grow in the presence of oxygen (aerobic versus anaerobic). The bacteria can be more narrowly identified by growing them on specific media (triple sugar iron (TSI) agar) where their enzymes can be identified (urease, oxidase) and their ability to ferment lactose can be tested.
* Stains poorly on Gram stain
** Pleomorphic rod/coccobacillus
*** Require special transport media
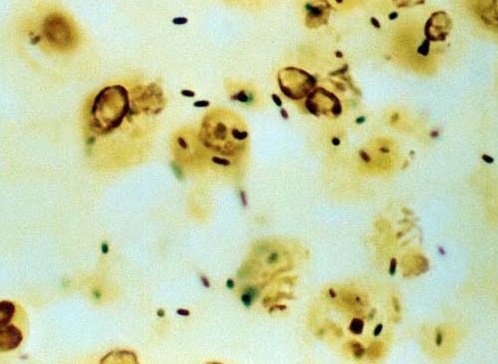
A silver stain of L. pneumophila
Image: “Legionella Silver Stain” by William Cherry. License: Public domain.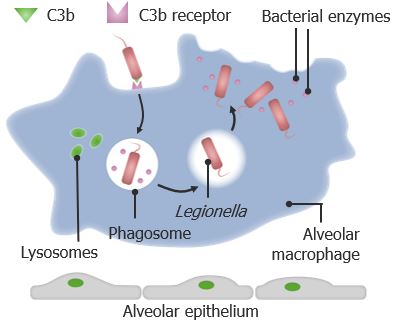
Pathogenesis of Legionella infection
The bacteria are opsonized by C3b (a cleaved component of C3) and are incorporated into the macrophages. Once inside the phagosome, the Legionella inhibits phagolysosomal fusion, which allows growth of the bacteria, producing degradative enzymes and toxins, eventually leading to apoptosis of the infected cell. The destroyed cell releases the bacteria, spreading the infection to other cells.
Infection with Legionella is known as legionellosis.
| Pontiac fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever | Legionnaires’ disease | |
|---|---|---|
| Infection rate | > 90% | < 5% |
| Time of onset | Throughout the year | Sporadic Sporadic Selective IgA Deficiency cases or outbreaks Outbreaks Sudden increase in the incidence of a disease. The concept includes epidemics and pandemics. Influenza Viruses/Influenza in late summer and early autumn |
| Incubation Incubation The amount time between exposure to an infectious agent and becoming symptomatic. Rabies Virus period | 1–2 days | 2–10 days |
| Manifestations |
|
|
| Resolution |
|
|
| Mortality Mortality All deaths reported in a given population. Measures of Health Status rate | < 1% | 15%–20% (if untreated) |
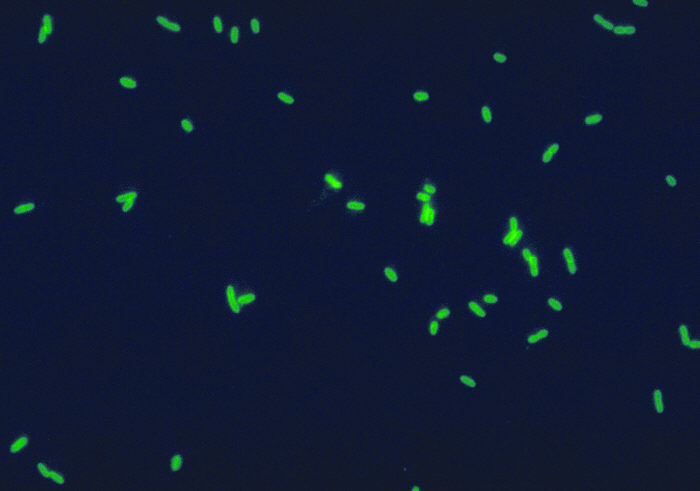
Legionella pneumophila: direct immunofluorescence staining with fluorescence-labeled antibodies
Image: “Legionella Pneumophila IF” by CDC-PHIL. License: Public domain.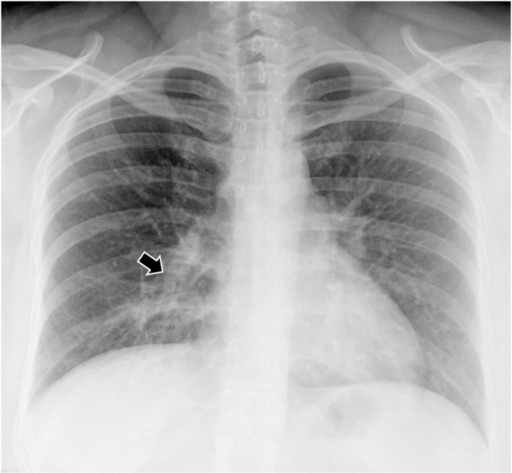
Chest X-ray of a patient with L. anisa pneumonia: Image shows right base infiltrates (arrow).
Image: “PMC4956277_pone.0159726.g002” by Vaccaro L, Izquierdo F, Magnet A, Hurtado C, Salinas MA, Gomes TS, Angulo S, Salso S, Pelaez J, Tejeda MI, Alhambra A, Gómez C, Enríquez A, Estirado E, Fenoy S, & Del Aguila C. License: CC BY 4.0.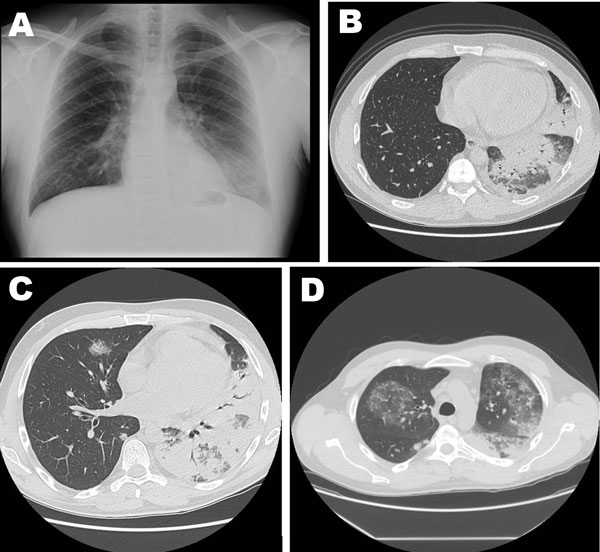
Various stages of Legionnaire’s disease in a 42-year-old man with severe pneumonia caused by L. pneumophila serogroup 11a
A: chest radiograph and B: high-resolution CT at hospital admission; C and D: repeat high-resolution CT of the chest a week after hospital admission