Laxatives are medications used to promote defecation Defecation The normal process of elimination of fecal material from the rectum. Gastrointestinal Motility. Most often, laxatives are used to treat constipation Constipation Constipation is common and may be due to a variety of causes. Constipation is generally defined as bowel movement frequency < 3 times per week. Patients who are constipated often strain to pass hard stools. The condition is classified as primary (also known as idiopathic or functional constipation) or secondary, and as acute or chronic. Constipation or for bowel preparation for certain procedures. There are 4 main classes of laxatives: bulk-forming, stimulant, osmotic, and emollient. Often, a combination of these medications is required to have the desired effect. All laxatives can result in bloating Bloating Constipation. Laxative Laxative Agents that produce a soft formed stool, and relax and loosen the bowels, typically used over a protracted period, to relieve constipation. Hypokalemia overuse can induce diarrhea Diarrhea Diarrhea is defined as ≥ 3 watery or loose stools in a 24-hour period. There are a multitude of etiologies, which can be classified based on the underlying mechanism of disease. The duration of symptoms (acute or chronic) and characteristics of the stools (e.g., watery, bloody, steatorrheic, mucoid) can help guide further diagnostic evaluation. Diarrhea and dehydration Dehydration The condition that results from excessive loss of water from a living organism. Volume Depletion and Dehydration. Non– anion gap Anion gap Metabolic Acidosis metabolic acidosis Acidosis A pathologic condition of acid accumulation or depletion of base in the body. The two main types are respiratory acidosis and metabolic acidosis, due to metabolic acid build up. Respiratory Acidosis occurs owing to bicarbonate Bicarbonate Inorganic salts that contain the -HCO3 radical. They are an important factor in determining the ph of the blood and the concentration of bicarbonate ions is regulated by the kidney. Levels in the blood are an index of the alkali reserve or buffering capacity. Electrolytes loss in the feces, while metabolic alkalosis Alkalosis A pathological condition that removes acid or adds base to the body fluids. Respiratory Alkalosis occurs because of volume contraction.
Last updated: Apr 22, 2025
Laxatives are medications that increase the frequency of bowel movements.
Bulk-forming laxatives tend to be either:
Adverse effects tend to be minimal with these agents but may include:
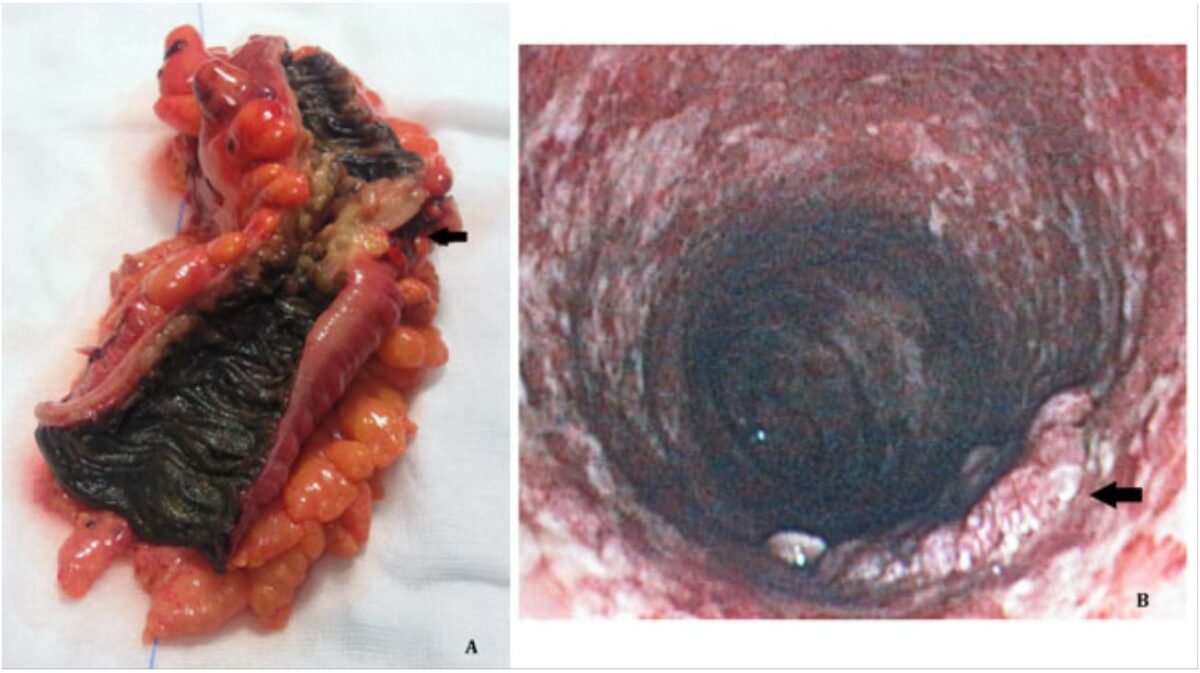
Melanosis coli is a black discoloration of the colon associated with stimulant laxative use.
Image: “Melanosis coli in the elderly: a look beyond what can be seen” by BMC Surgery. License: CC BY 2.0Osmotic laxatives are often:
Lactulose should not be used in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with galactosemia Galactosemia Galactosemia is a disorder caused by defects in galactose metabolism. Galactosemia is an inherited, autosomal-recessive condition, which results in inadequate galactose processing and high blood levels of monosaccharide. The rare disorder often presents in infants with symptoms of lethargy, nausea, vomiting, diarrhea, and jaundice. Galactosemia.
Docusate (Colace) is a common emollient laxative Laxative Agents that produce a soft formed stool, and relax and loosen the bowels, typically used over a protracted period, to relieve constipation. Hypokalemia, also known as a “stool softener.”
Side effects are generally mild but may include:
The following table compares and contrasts members of the laxative Laxative Agents that produce a soft formed stool, and relax and loosen the bowels, typically used over a protracted period, to relieve constipation. Hypokalemia drug class:
| Class | Examples | Mechanism of action | Side effects |
|---|---|---|---|
| Bulk-forming laxatives |
|
|
|
| Stimulant laxatives |
|
Myenteric plexus Myenteric plexus One of two ganglionated neural networks which together form the enteric nervous system. The myenteric (Auerbach’s) plexus is located between the longitudinal and circular muscle layers of the gut. Its neurons project to the circular muscle, to other myenteric ganglia, to submucosal ganglia, or directly to the epithelium, and play an important role in regulating and patterning gut motility. Gastrointestinal Neural and Hormonal Signaling stimulation resulting in colonic contractions |
|
| Osmotic laxatives |
|
Draws water into GI lumen, softening the stools |
|
| Emollient laxatives | Docusate |
|
|