The knee joint is made up of the articulations between the femur, tibia, and patella bones, and is one of the largest and most complex joints of the human body. The knee is classified as a synovial hinge joint, which primarily allows for flexion Flexion Examination of the Upper Limbs and extension Extension Examination of the Upper Limbs with a more limited degree of translation Translation Translation is the process of synthesizing a protein from a messenger RNA (mRNA) transcript. This process is divided into three primary stages: initiation, elongation, and termination. Translation is catalyzed by structures known as ribosomes, which are large complexes of proteins and ribosomal RNA (rRNA). Stages and Regulation of Translation and rotation Rotation Motion of an object in which either one or more points on a line are fixed. It is also the motion of a particle about a fixed point. X-rays. The supporting structures of the knee joint include a joint capsule Capsule An envelope of loose gel surrounding a bacterial cell which is associated with the virulence of pathogenic bacteria. Some capsules have a well-defined border, whereas others form a slime layer that trails off into the medium. Most capsules consist of relatively simple polysaccharides but there are some bacteria whose capsules are made of polypeptides. Bacteroides, the lateral and medial menisci Menisci Meniscus Tear, and multiple ligaments that help ensure mobility and stability of the knee.
Last updated: Dec 15, 2025
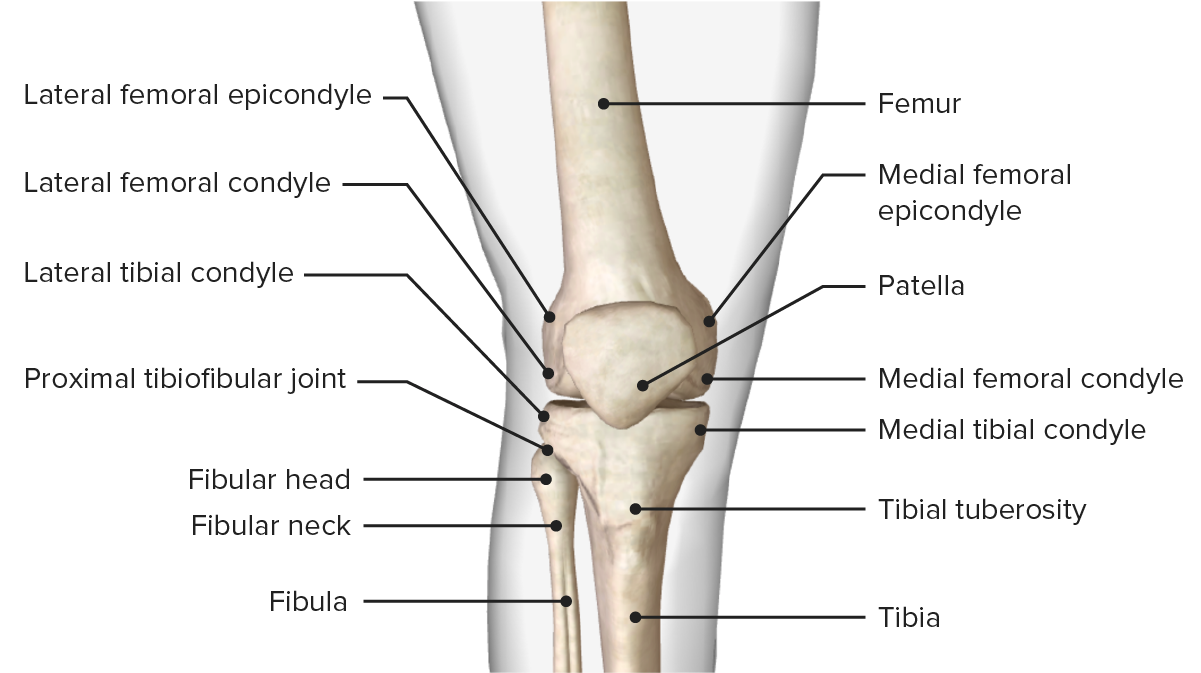
Anterior view of the bony structure of the knee, featuring the bony landmarks of the femur, tibia, and patella bones
Image by BioDigital, edited by Lecturio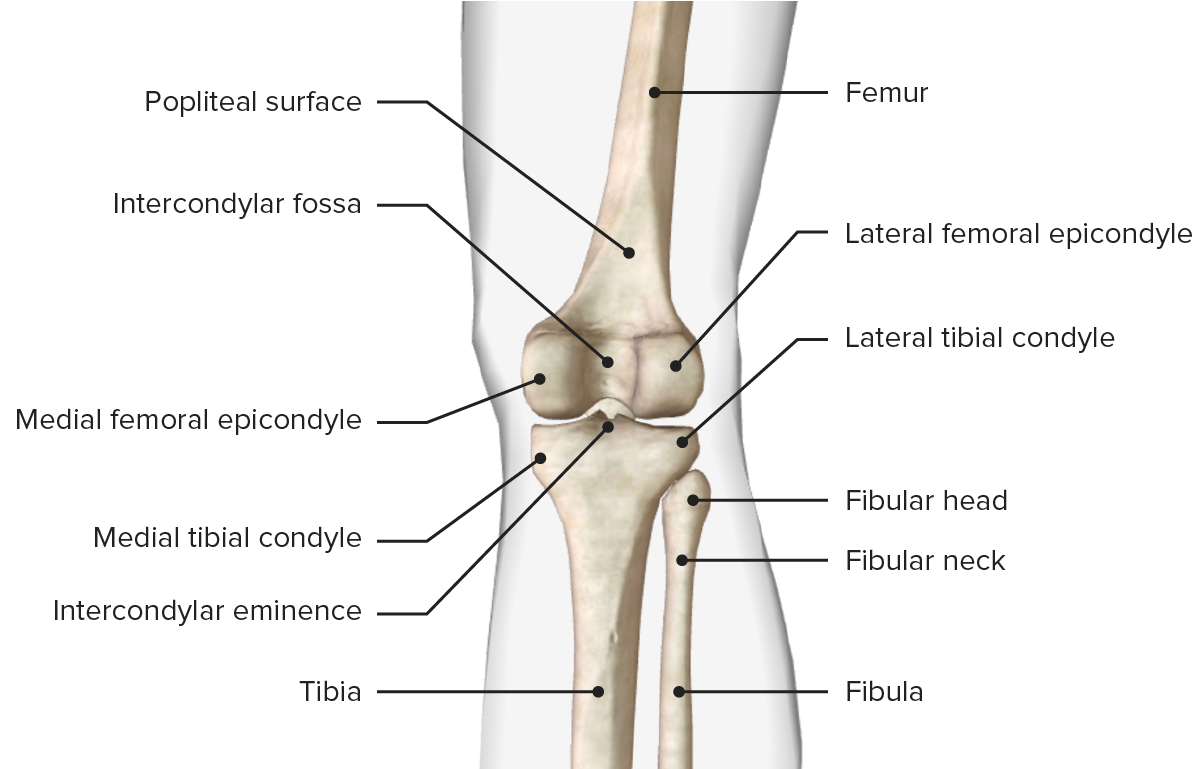
Posterior view of the bony structure of the knee, featuring the bony landmarks of the femur, tibia, and patella bones
Image by BioDigital, edited by LecturioThe knee is a modified hinge joint; a double condyloid articulation. Although the motions of the knee are primarily flexion Flexion Examination of the Upper Limbs and extension Extension Examination of the Upper Limbs, it has a complex movement pattern consisting of 6 degrees of motion during dynamic activities:
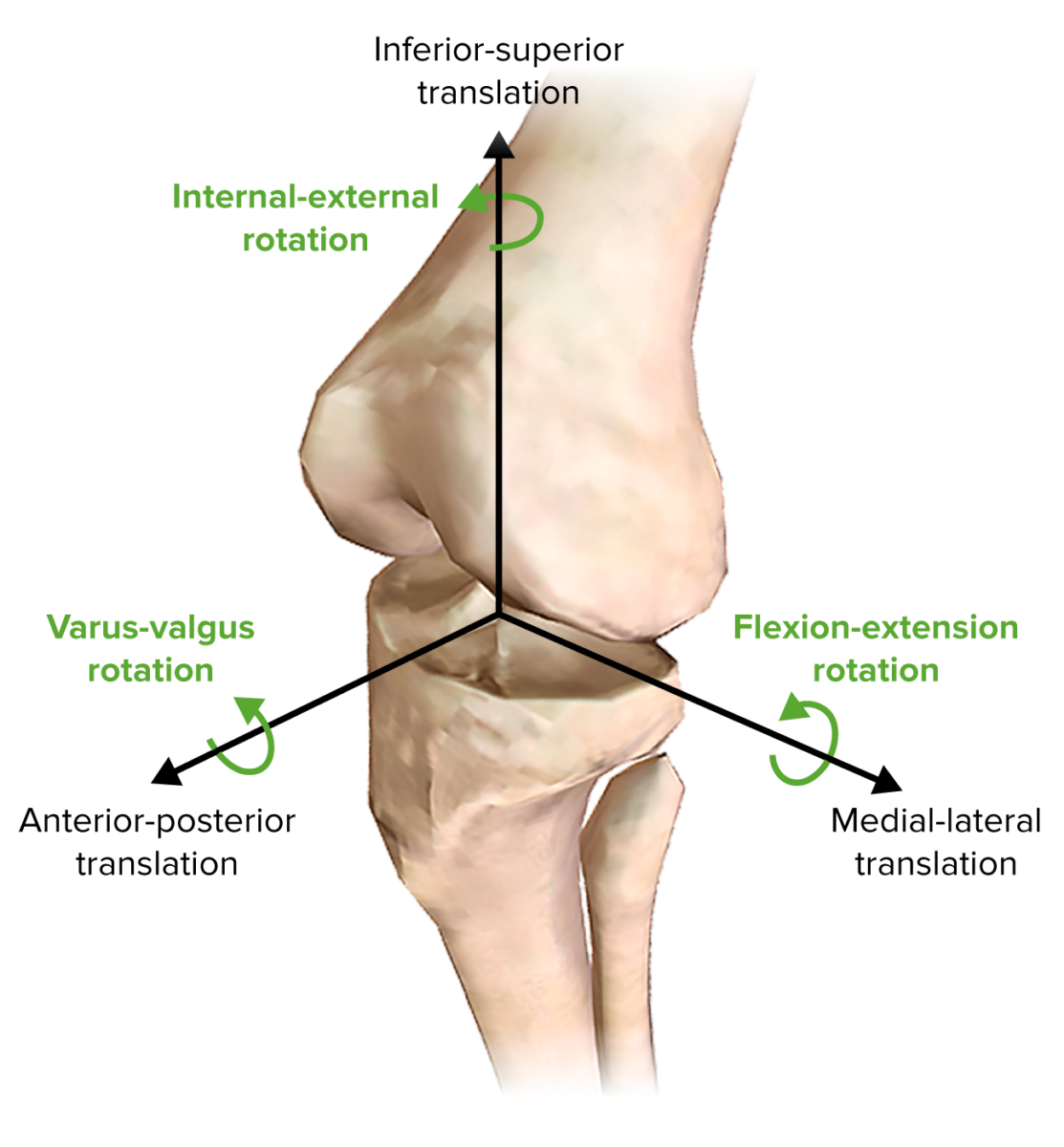
Motions of the knee
Image by BioDigital, edited by Lecturio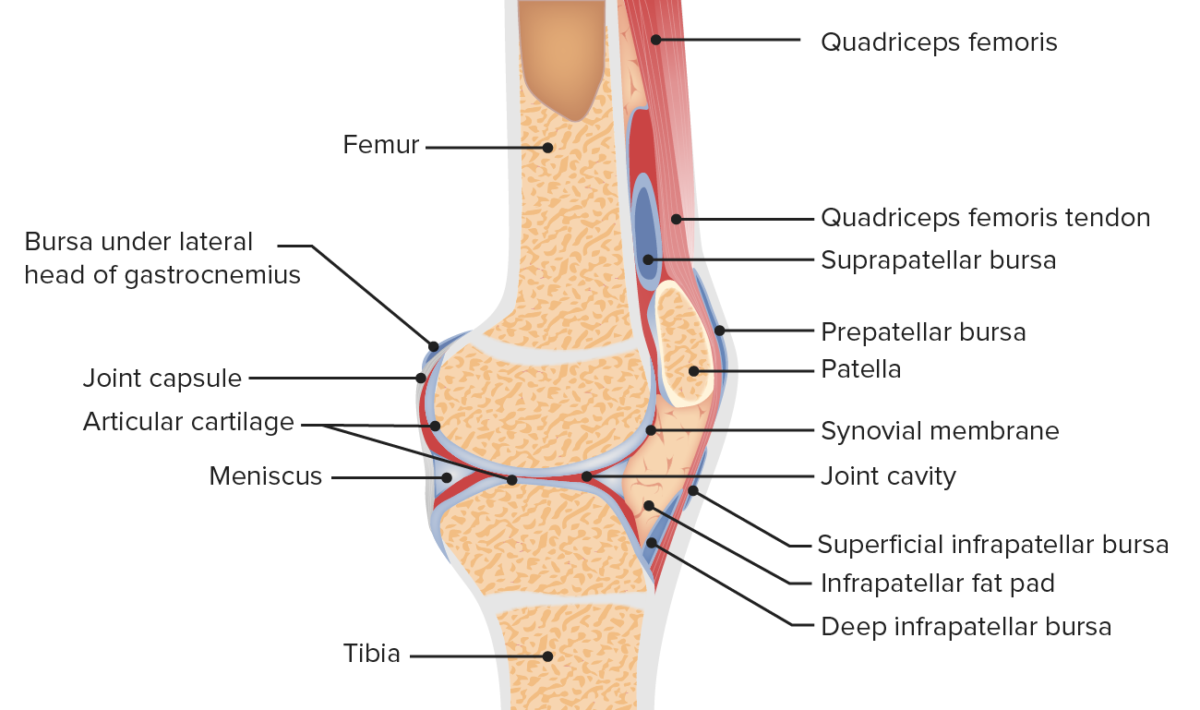
Anatomy of the patellofemoral joint
Image by Lecturio. License: CC BY-NC-SA 4.0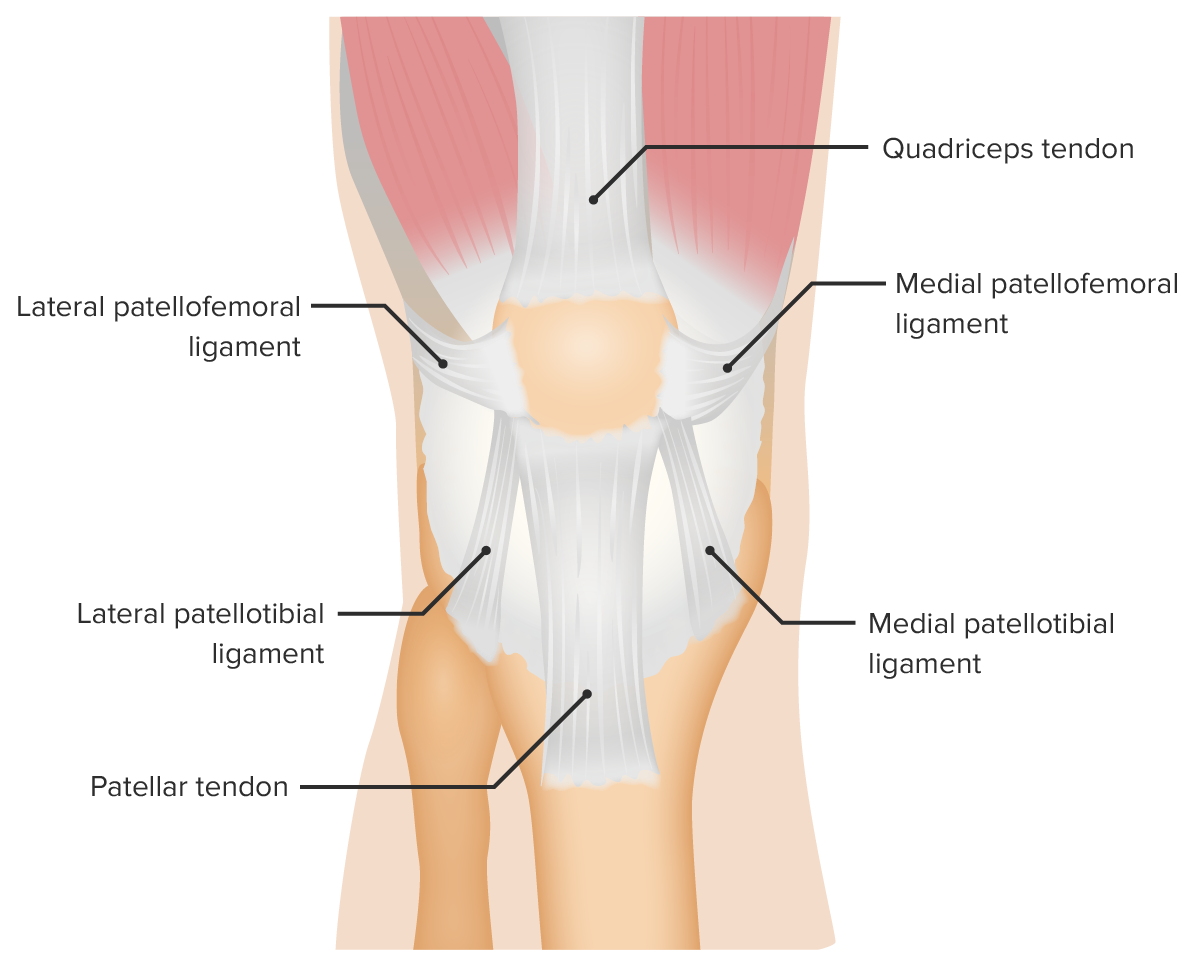
Supporting ligaments of the patellofemoral joint
Image by Lecturio. License: CC BY-NC-SA 4.0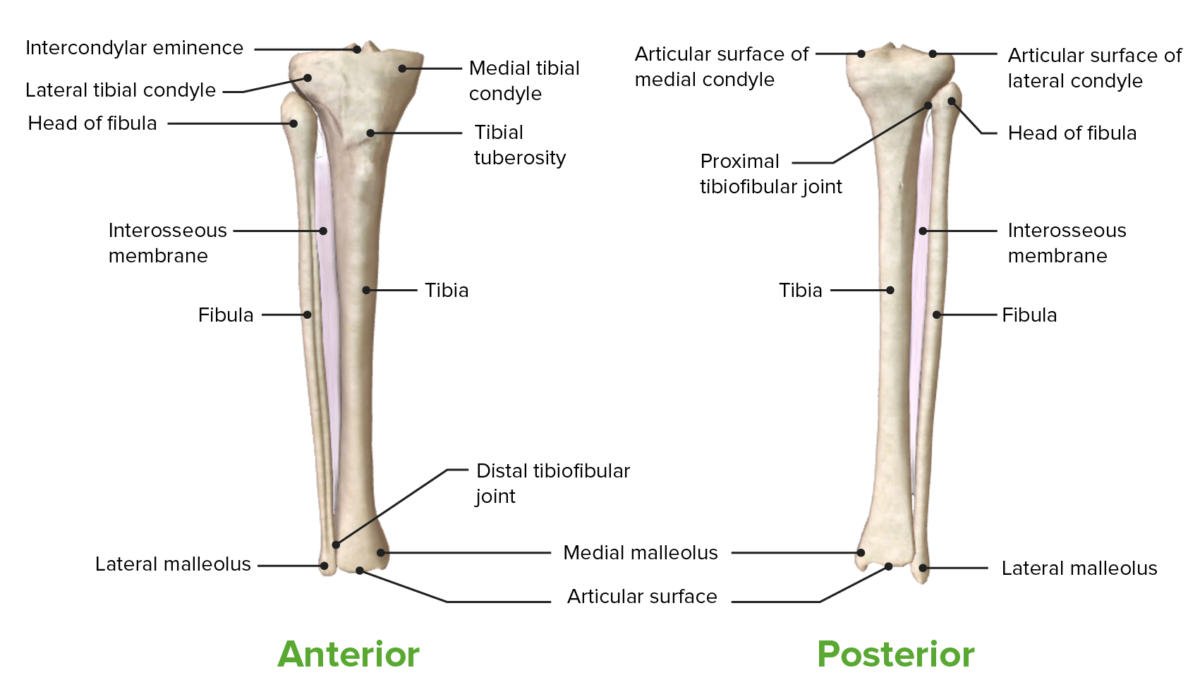
Anterior and posterior views of the tibia, fibula, and tibiofibular joints
Image by BioDigital, edited by LecturioThe menisci Menisci Meniscus Tear are semilunar-shaped fibrocartilage Fibrocartilage A type of cartilage whose matrix contains large bundles of collagen type I. Fibrocartilage is typically found in the intervertebral disk; pubic symphysis; tibial menisci; and articular discs in synovial joints. Cartilage: Histology wedges between the femur and tibia and made of type I collagen Type I Collagen Ehlers-Danlos Syndrome fibers. Menisci Menisci Meniscus Tear are shock Shock Shock is a life-threatening condition associated with impaired circulation that results in tissue hypoxia. The different types of shock are based on the underlying cause: distributive (↑ cardiac output (CO), ↓ systemic vascular resistance (SVR)), cardiogenic (↓ CO, ↑ SVR), hypovolemic (↓ CO, ↑ SVR), obstructive (↓ CO), and mixed. Types of Shock absorbers, improve the congruence of the tibiofemoral joint, and are vital for the normal functioning and health of the knee.
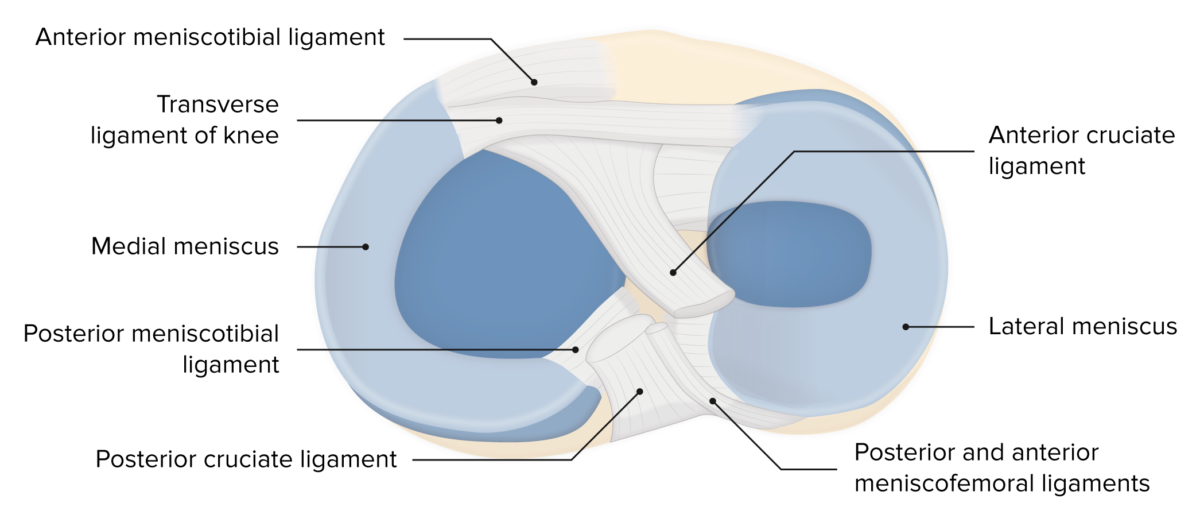
Menisci of the knee
Image by Lecturio. License: CC BY-NC-SA 4.0
Image displaying the menisci, ligaments, and bony surfaces, and their relation to one another
Image by Lecturio. License: CC BY-NC-SA 4.0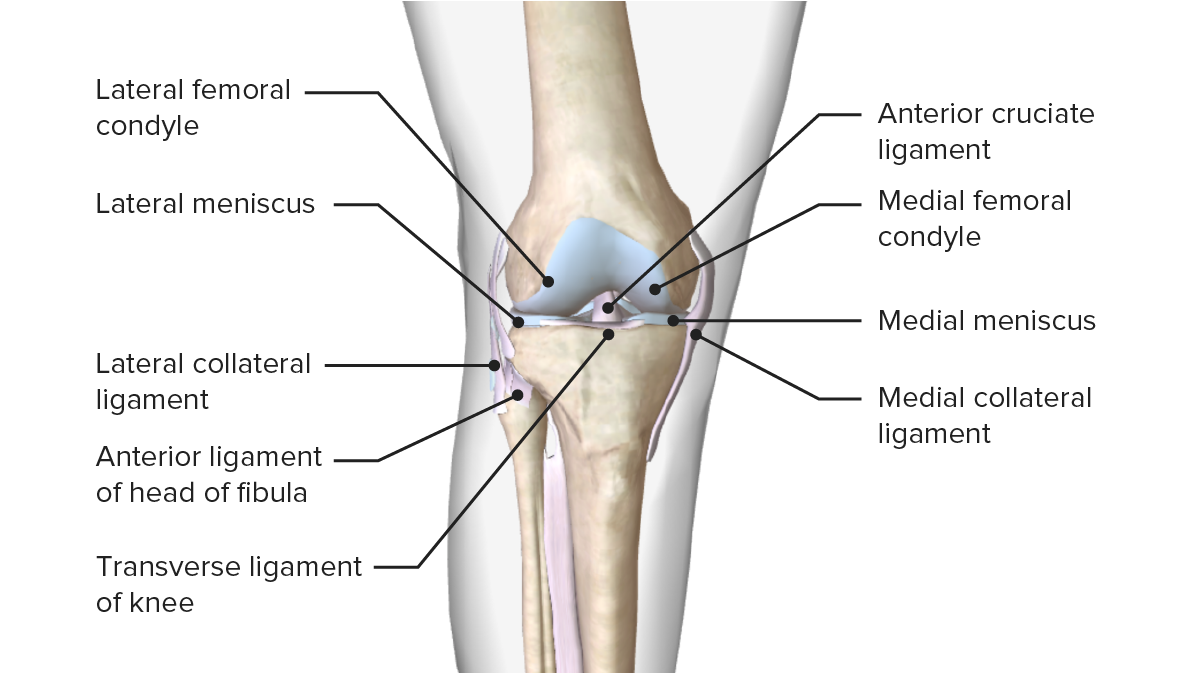
Image displaying the menisci and their relation with other articular surfaces that compose the knee joint
Image by BioDigital, edited by LecturioA 2-layered joint capsule Capsule An envelope of loose gel surrounding a bacterial cell which is associated with the virulence of pathogenic bacteria. Some capsules have a well-defined border, whereas others form a slime layer that trails off into the medium. Most capsules consist of relatively simple polysaccharides but there are some bacteria whose capsules are made of polypeptides. Bacteroides provides support to the knee. These layers are the external fibrous Fibrous Fibrocystic Change membrane and internal synovial membrane Synovial Membrane The inner membrane of a joint capsule surrounding a freely movable joint. It is loosely attached to the external fibrous capsule and secretes synovial fluid. Hip Joint: Anatomy.
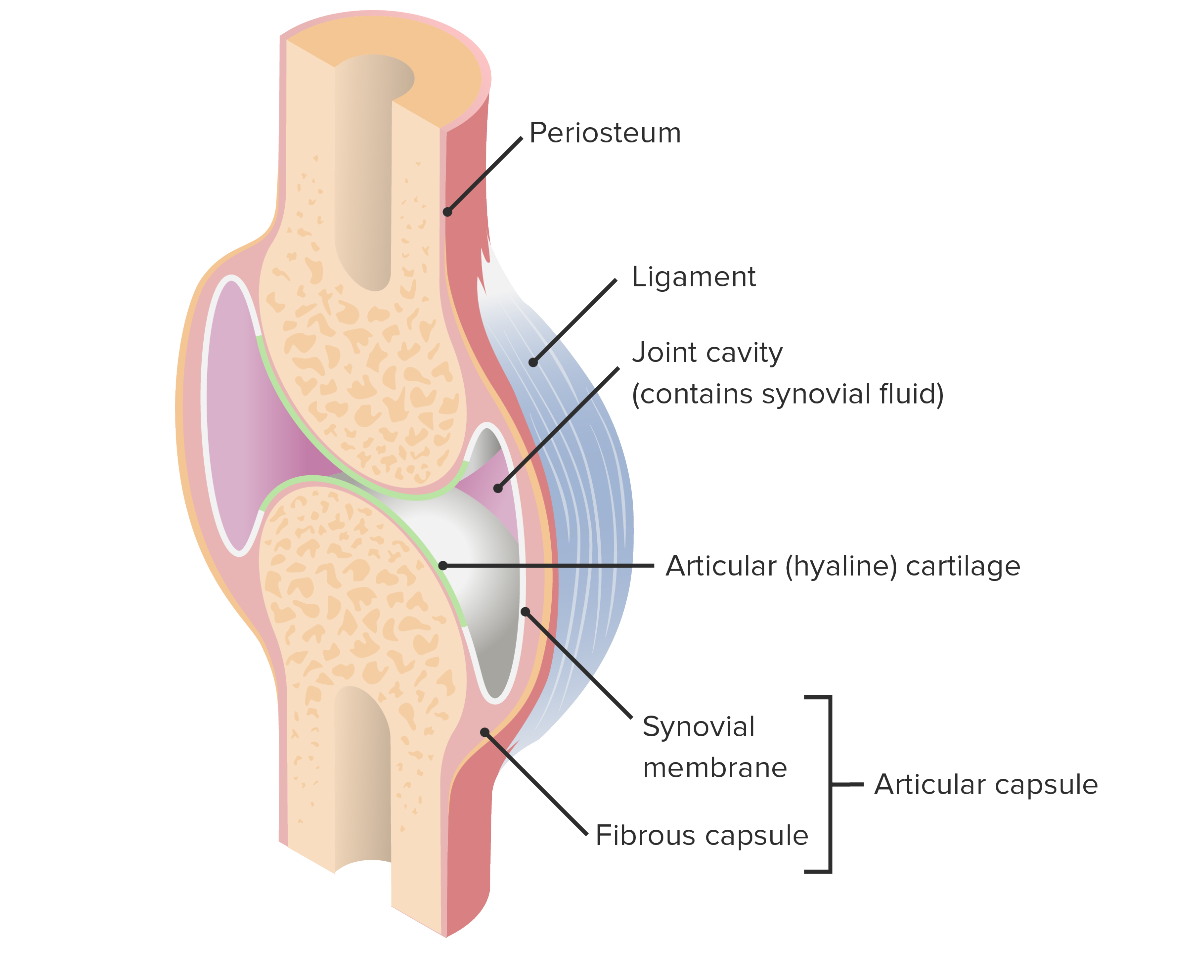
Articular capsule and its components
Image by Lecturio. License: CC BY-NC-SA 4.0Ligaments and tendons of the knee provide stability to the knee during motion and increase the efficiency of the knee.
| Ligament/tendon | Origin | Insertion | Function |
|---|---|---|---|
| Anterior cruciate ligament (ACL) is composed of 2 bundles:
|
Inner lateral femoral condyle | Roof of the intercondylar fossa |
|
| Posterior cruciate ligament (PCL) is composed of 2 bundles:
|
Inner surface of the medial femoral condyle | Posterior intercondylar area of the tibia |
|
| Medial collateral ligament (MCL) | Medial femoral epicondyle | Medial condyle of the tibia | Stabilizes the knee joint against valgus stress |
| Lateral/fibular collateral ligament | Lateral femoral epicondyle | Head of the fibula Fibula The bone of the lower leg lateral to and smaller than the tibia. In proportion to its length, it is the most slender of the long bones. Leg: Anatomy | Stabilizes the knee joint against varus stress |
| Patellar ligament Patellar ligament A band of fibrous tissue that attaches the apex of the patella to the lower part of the tubercle of the tibia. The ligament is actually the caudal continuation of the common tendon of the quadriceps femoris. The patella is embedded in that tendon. As such, the patellar ligament can be thought of as connecting the quadriceps femoris tendon to the tibia, and therefore it is sometimes called the patellar tendon. Osgood-Schlatter Disease | Distal patella | Tuberosity of the tibia | Component of the extensor mechanism of the knee |
| Quadriceps tendon | Quadriceps muscles | Proximal patella | Component of the extensor mechanism of the knee |
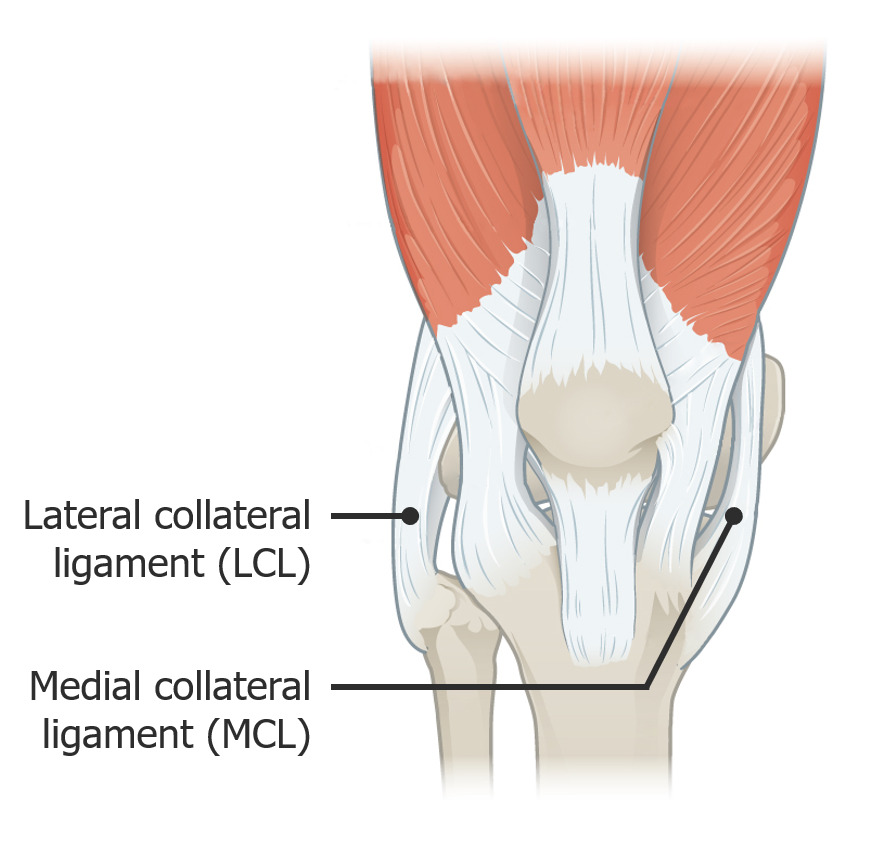
Image showing the lateral and medial collateral ligaments
Image: “917 Knee Joint” by OpenStax College. License: CC BY 3.0, edited by Lecturio.
Image displaying the menisci, ligaments, and bony surfaces, and their relation to one another
Image by Lecturio. License: CC BY-NC-SA 4.0Bursae are serous membranes/synovial fluid-filled sacs with a small amount of fluid facilitating movement around a joint. There are multiple bursae described around the knee joint.
| Bursae | Location |
|---|---|
| Suprapatellar | Between the femur and tendon of the quadriceps muscle |
| Prepatellar | Between the patella and skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions |
| Infrapatellar (superficial and deep) |
|
| Pes anserinus Pes anserinus Thigh: Anatomy | Medial knee/proximal medial tibia |
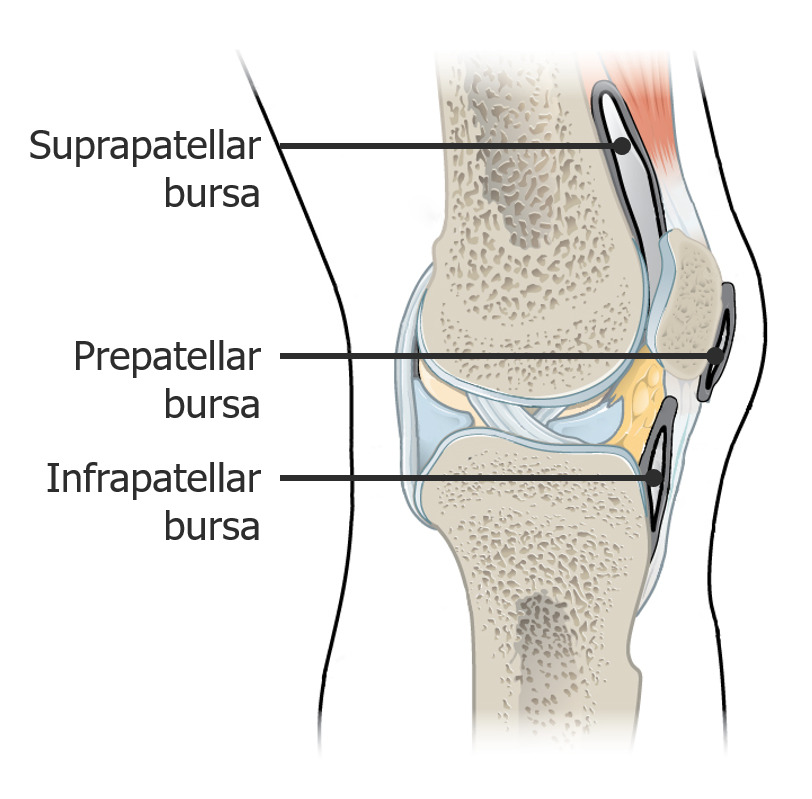
Image showing the bursae
Image: “917 Knee Joint” by OpenStax College. License: CC BY 3.0, edited by Lecturio.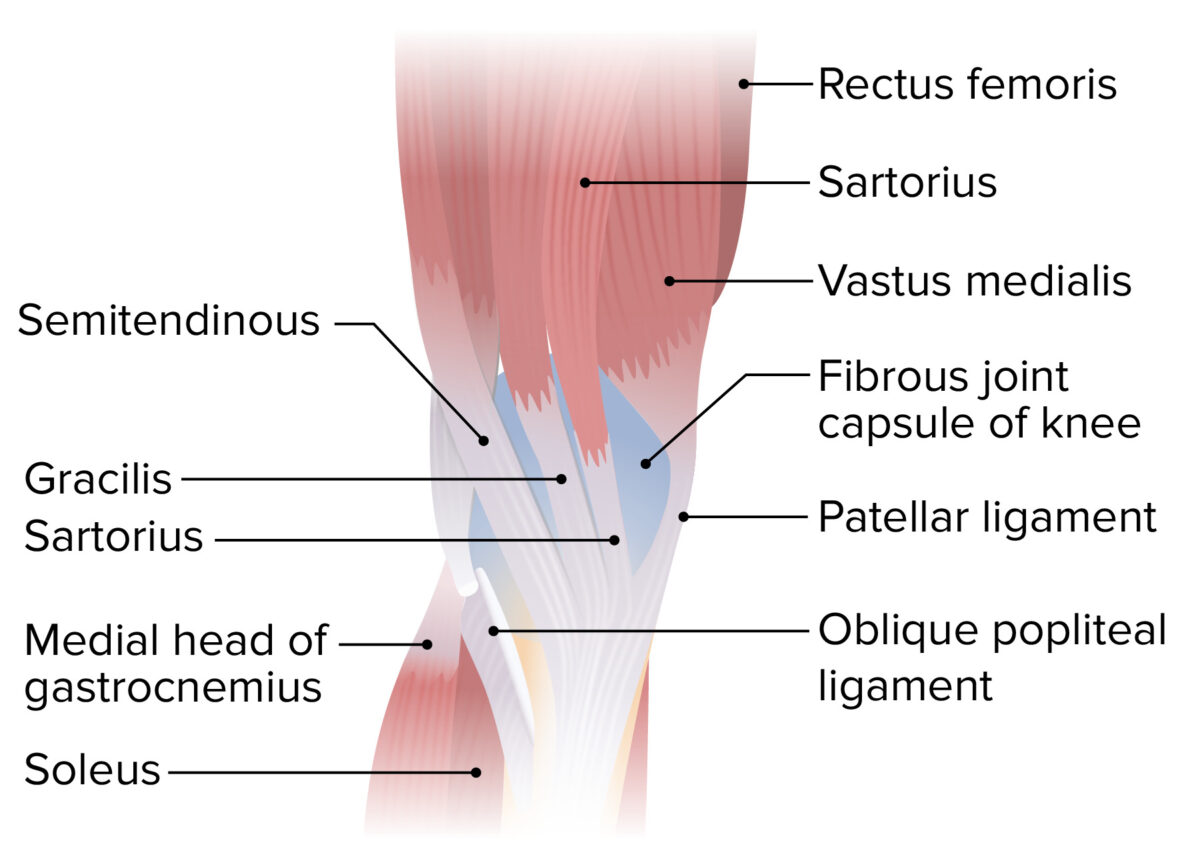
Medial view of the lower thigh and knee joint featuring the insertion of the sartorius, gracilis, and semitendinosus muscles, forming the pes anserinus (“goose’s foot”)
Image by Lecturio. License: CC BY-NC-SA 4.0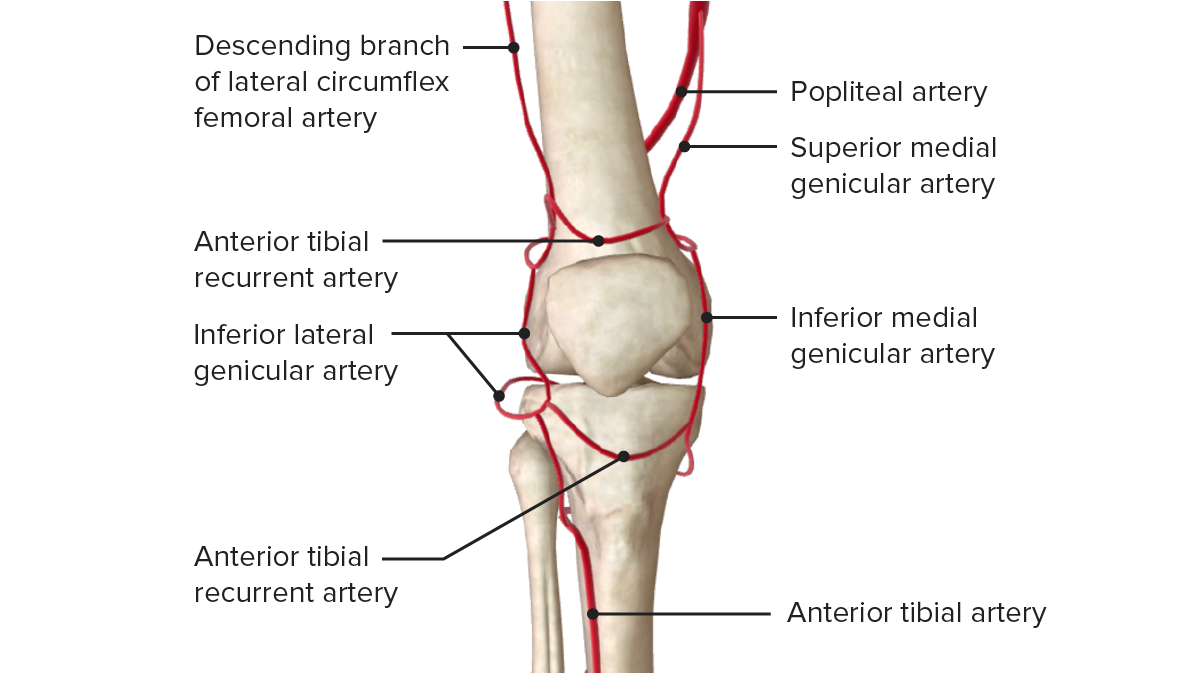
Anterior view of the vascular supply of the knee joint
Image by BioDigital, edited by Lecturio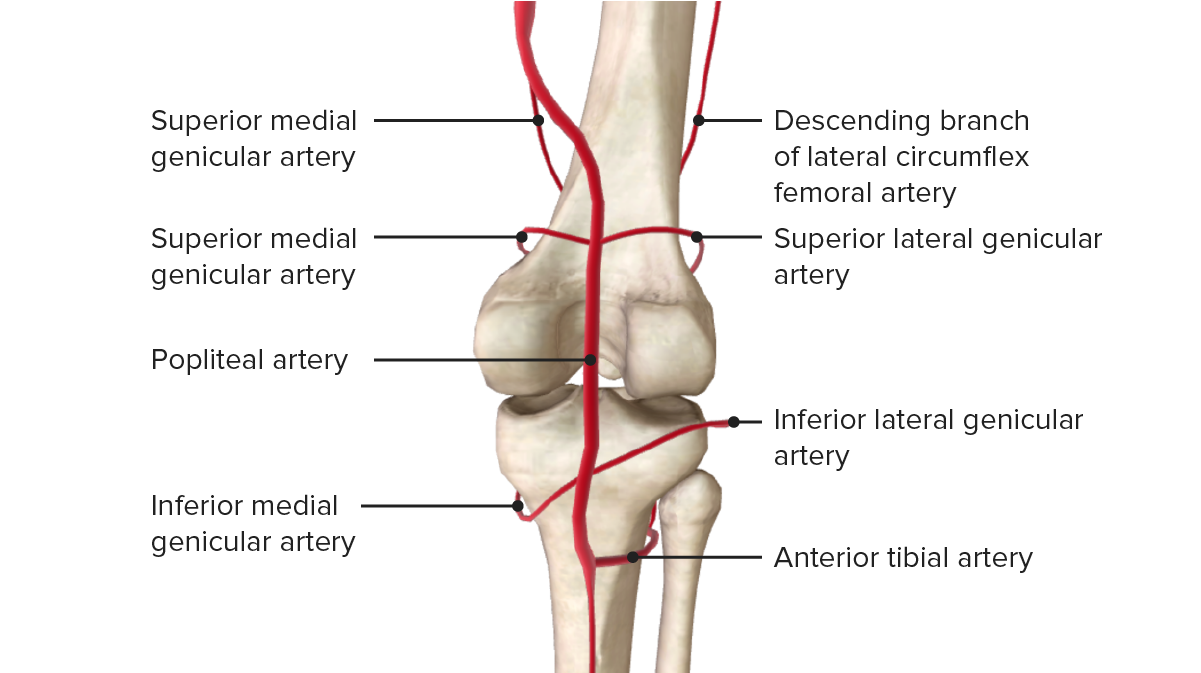
Posterior view of the vascular supply of the knee joint
Image by BioDigital, edited by LecturioThe following common conditions are associated with the knee: