The kidneys are a pair of bean-shaped organs located retroperitoneally against the posterior wall of the abdomen on either side of the spine Spine The human spine, or vertebral column, is the most important anatomical and functional axis of the human body. It consists of 7 cervical vertebrae, 12 thoracic vertebrae, and 5 lumbar vertebrae and is limited cranially by the skull and caudally by the sacrum. Vertebral Column: Anatomy. As part of the urinary tract Urinary tract The urinary tract is located in the abdomen and pelvis and consists of the kidneys, ureters, urinary bladder, and urethra. The structures permit the excretion of urine from the body. Urine flows from the kidneys through the ureters to the urinary bladder and out through the urethra. Urinary Tract: Anatomy, the kidneys are responsible for blood filtration and excretion of water-soluble waste in the urine. The kidneys also play a major role in homeostatic processes, including electrolyte concentration, blood pressure, and acid–base regulation. Grossly, they consist of an outer cortex and inner medulla. Microscopic functional units known as nephrons filter the blood through a structure called the glomerulus, and this filtrate is then modified and concentrated as it moves through a complex tubular system. The renal arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology supply the kidneys via a central opening, known as the renal hilum Hilum Lungs: Anatomy, on its medial side; large renal veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology empty directly into the vena cava.
Last updated: Dec 15, 2025
The kidney develops from embryonic mesoderm Mesoderm The middle germ layer of an embryo derived from three paired mesenchymal aggregates along the neural tube. Gastrulation and Neurulation in 3 successive forms from the nephrogenic cords Nephrogenic cords Development of the Urogenital System as they elongate in a cranial-to-caudal direction.
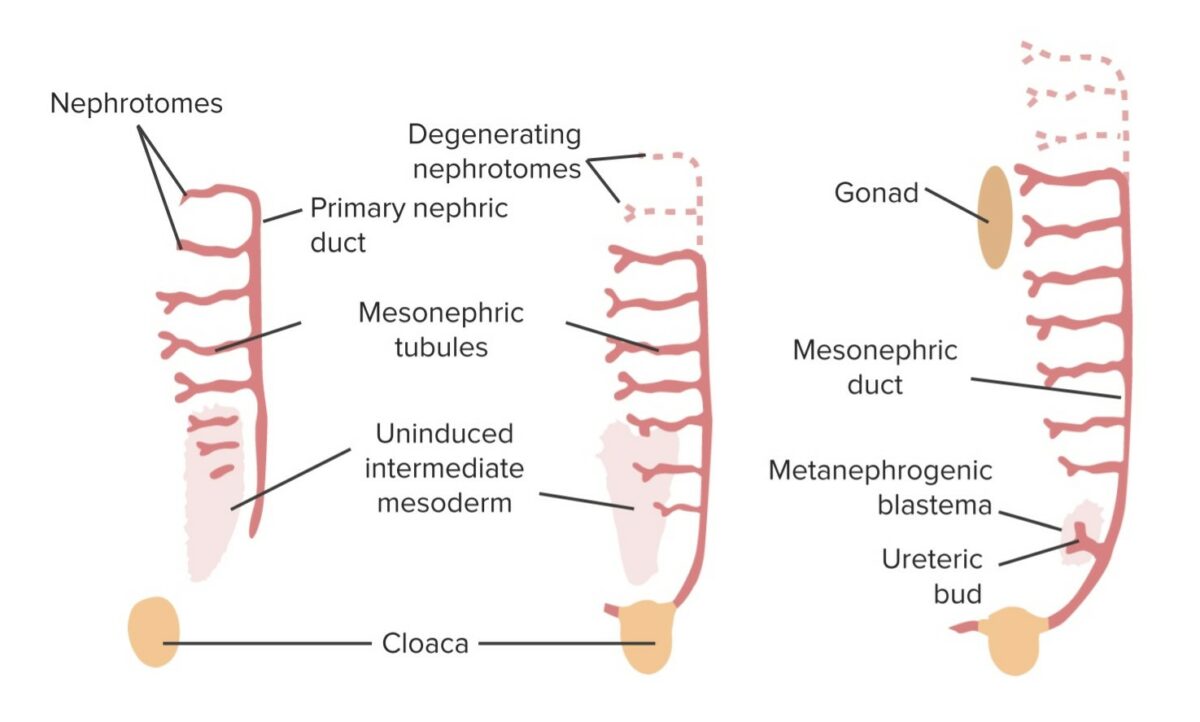
Graphical summary of the developing kidney:
The ureteric bud grows off of the mesonephric duct and into a collection of intermediate mesoderm cells known as the metanephric blastema. Together, this is known as the mesonephros, which develops into the kidney. The mesonephric tubules regress. In males, the mesonephric duct persists in the ejaculatory system.
The permanent kidney is formed from the metanephros Metanephros Development of the Urogenital System.
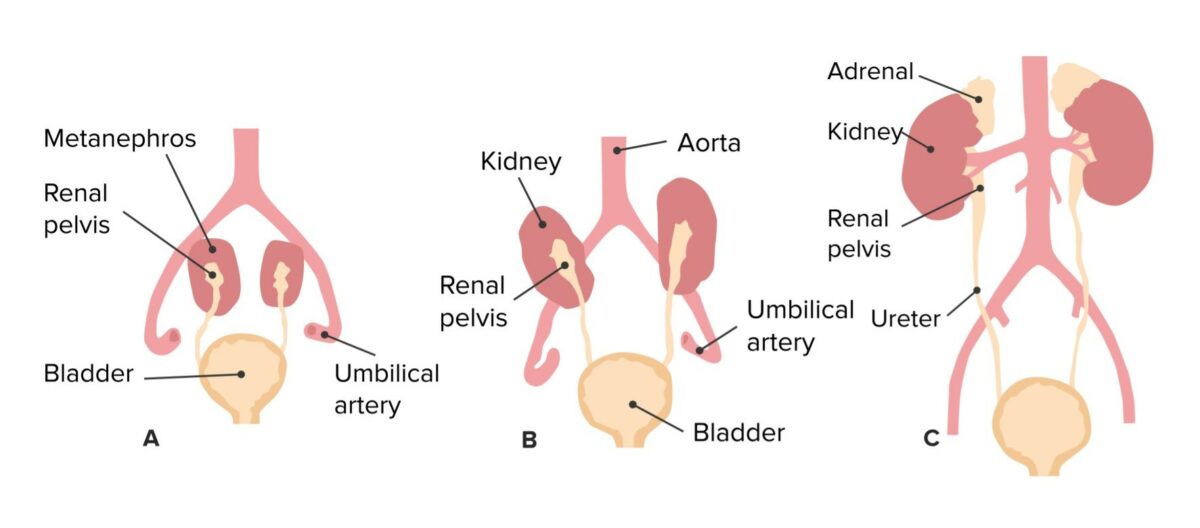
Ascent of the kidneys and corresponding change in vascular supply
Image by Lecturio.| Direction (in relation to the kidney) | Right | Left |
|---|---|---|
| Superior | Right adrenal gland | Left adrenal gland |
| Anterior |
|
|
| Lateral | Liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy |
|
| Posterior |
|
|
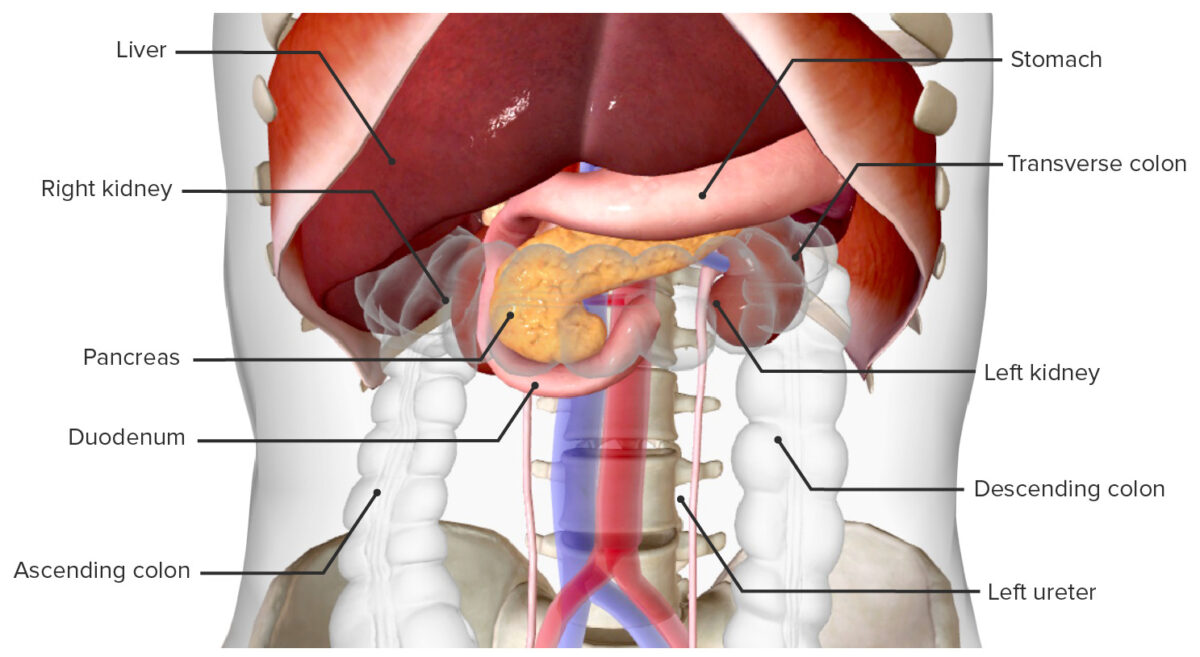
Kidneys in situ (anterior view)
Image by BioDigital, edited by Lecturio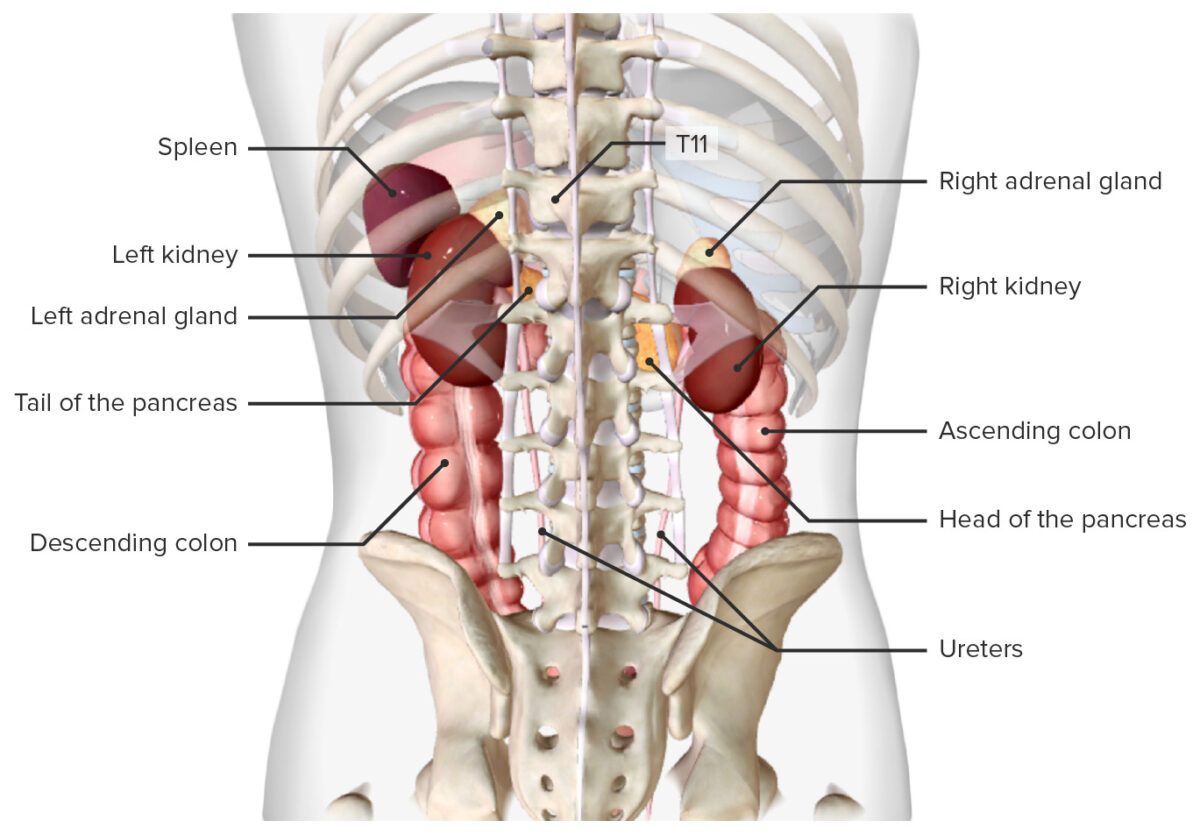
Location of the kidneys in situ (posterior view)
Image by BioDigital, edited by Lecturio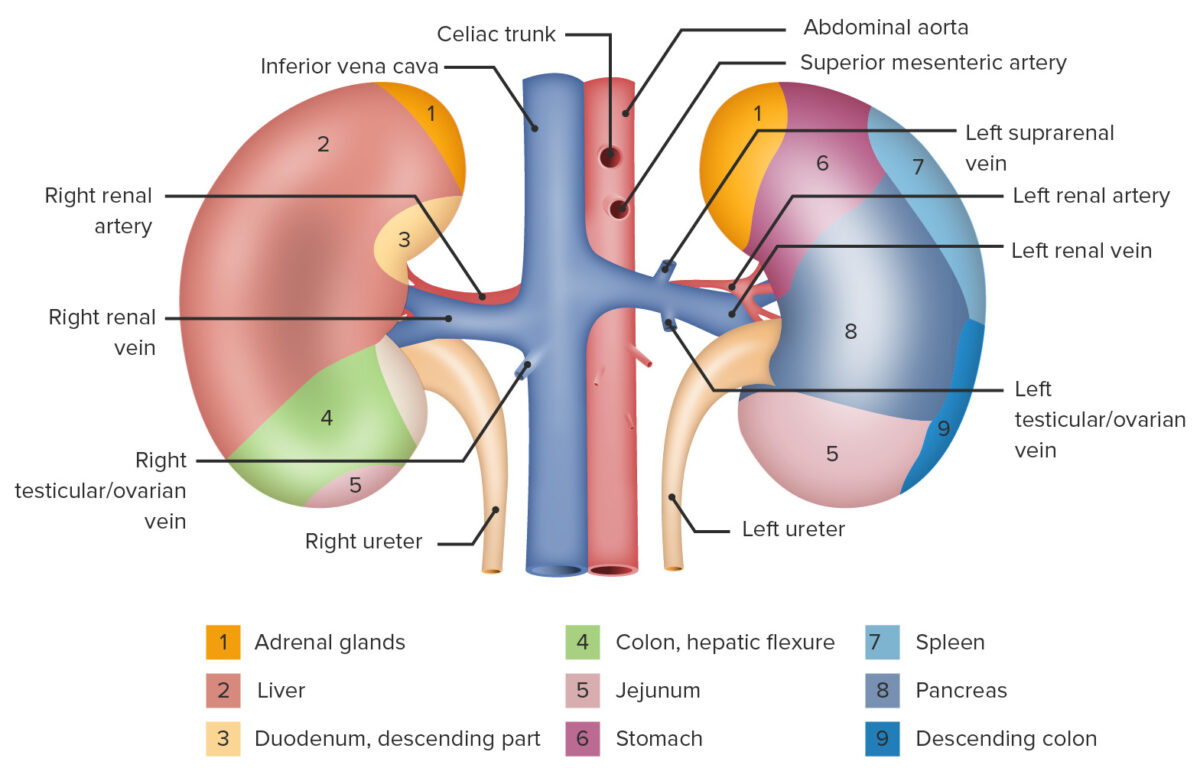
Kidneys with shadings showing their anatomical relations
Image by Lecturio.Surrounding the kidneys are several layers of adipose and connective tissue Connective tissue Connective tissues originate from embryonic mesenchyme and are present throughout the body except inside the brain and spinal cord. The main function of connective tissues is to provide structural support to organs. Connective tissues consist of cells and an extracellular matrix. Connective Tissue: Histology (from outside in):
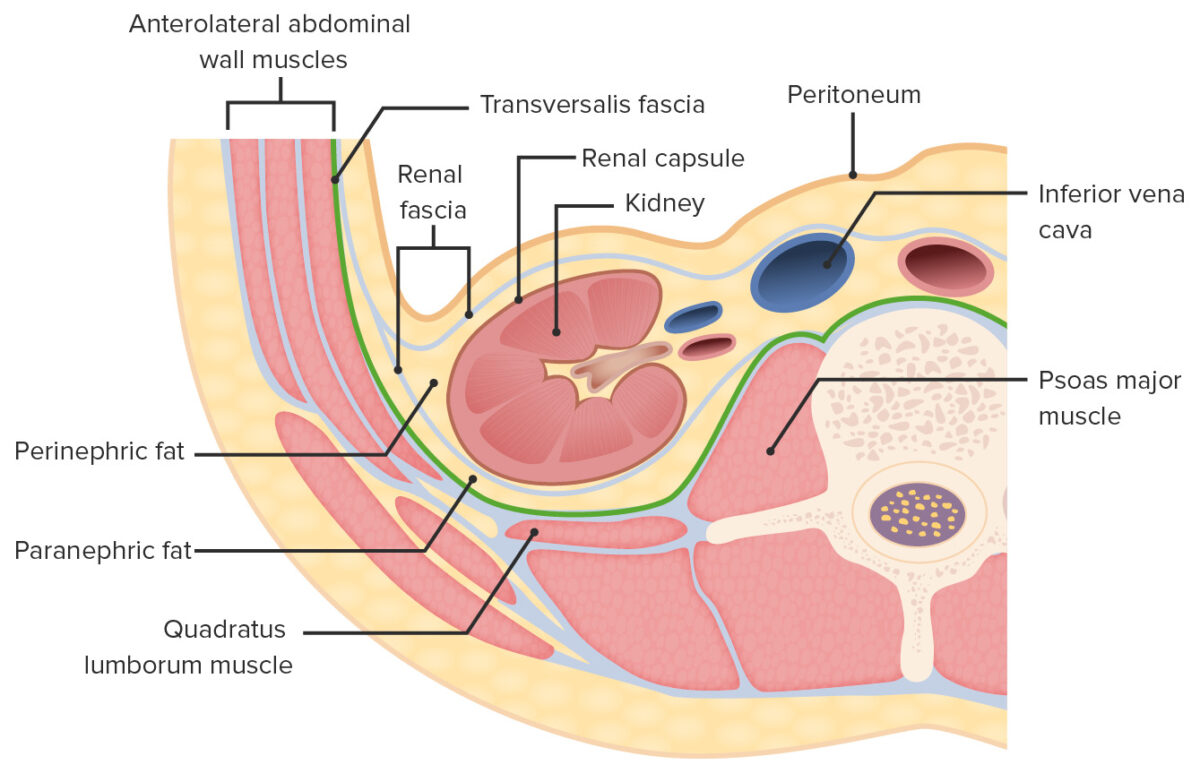
Layers of adipose and connective tissue surrounding the kidneys (transverse section)
Image by Lecturio.The parenchyma consists of:
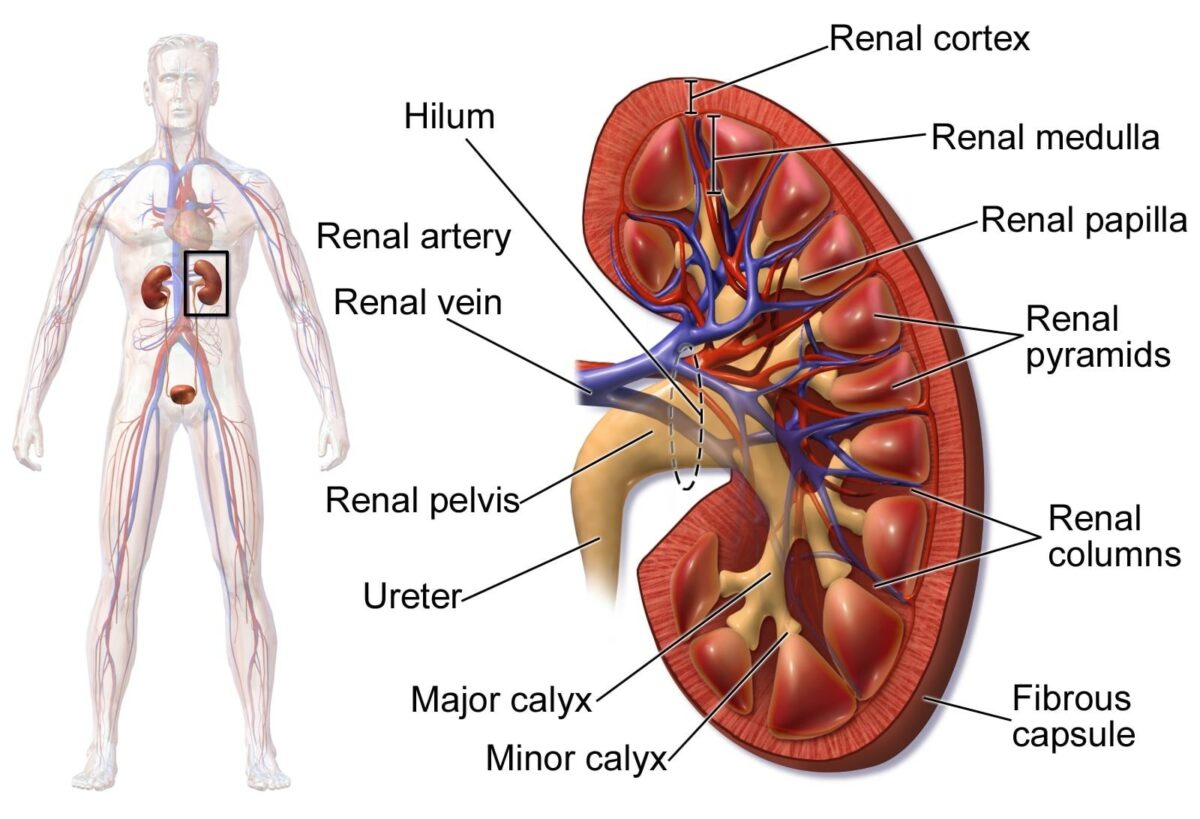
Diagram depicting the renal anatomy
Image: “Human Kidney Anatomy” by Blausen.com staff. License: CC BY 3.0, cropped by Lecturio.Nephrons are the functional units of the kidney; there are approximately 1.2 million nephrons in each kidney. The nephron is divided into 2 main parts: the renal corpuscle and the renal tubule, which has multiple defined segments.
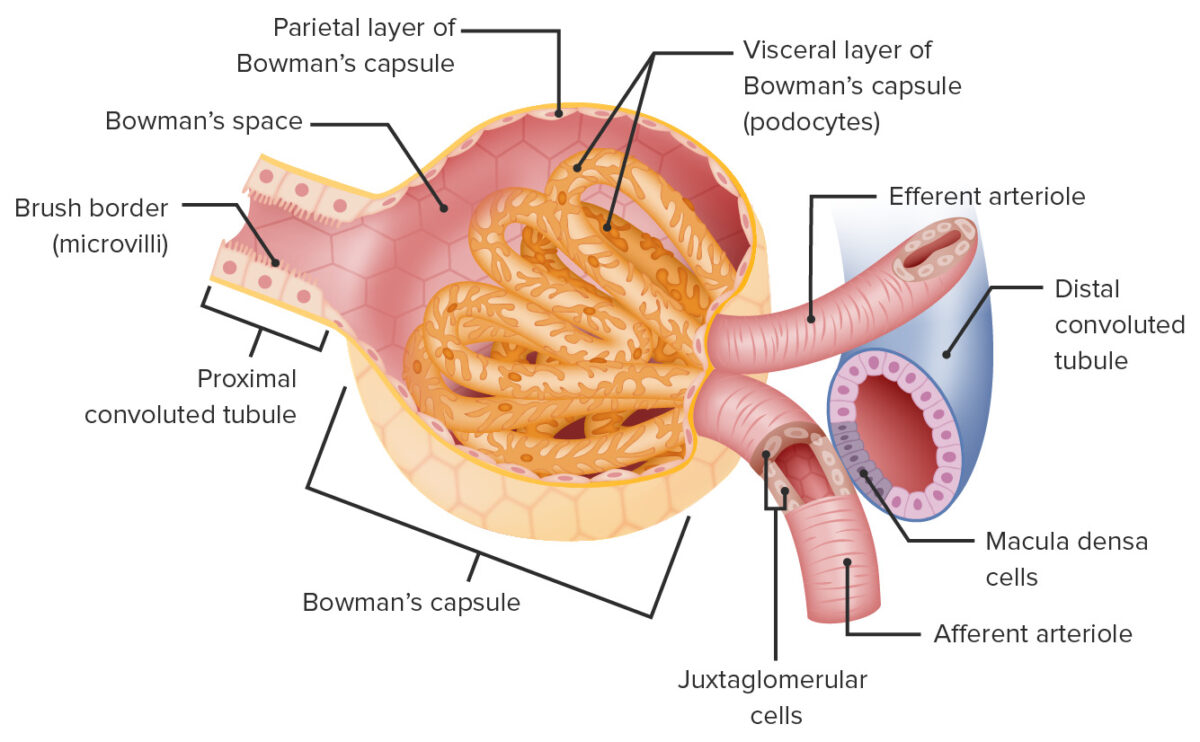
The renal corpuscle is where the blood plasma Plasma The residual portion of blood that is left after removal of blood cells by centrifugation without prior blood coagulation. Transfusion Products is filtered.
Glomerular (Bowman) capsule Capsule An envelope of loose gel surrounding a bacterial cell which is associated with the virulence of pathogenic bacteria. Some capsules have a well-defined border, whereas others form a slime layer that trails off into the medium. Most capsules consist of relatively simple polysaccharides but there are some bacteria whose capsules are made of polypeptides. Bacteroides:
Structure of the renal corpuscle
Image by Lecturio.Blood vessels associated with the renal corpuscle:
Filtration membrane:
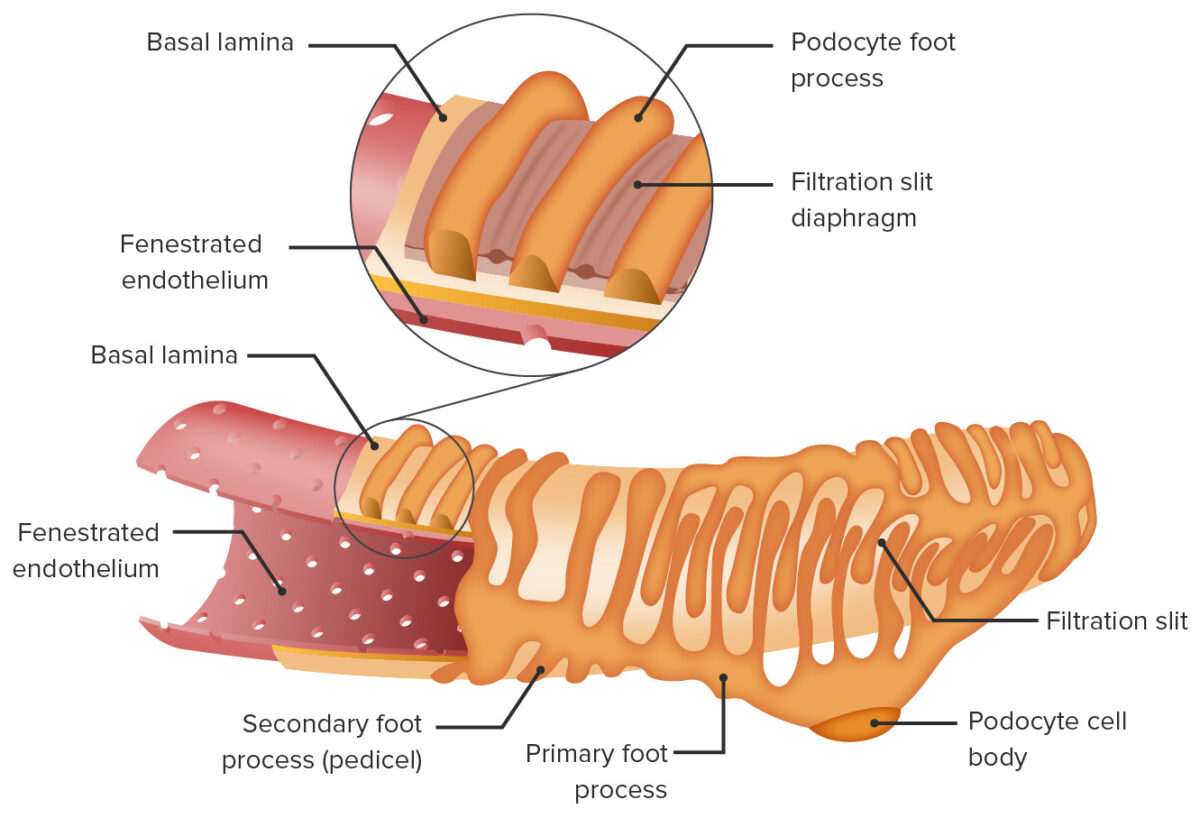
Filtration apparatus in the glomerulus
Image by Lecturio.The renal tubule is a long continuous tube that adjusts the contents of the filtrate received from the renal corpuscle. The tubules ultimately drain through the papilla into the calyces. Segments of the tubule, in order, are:
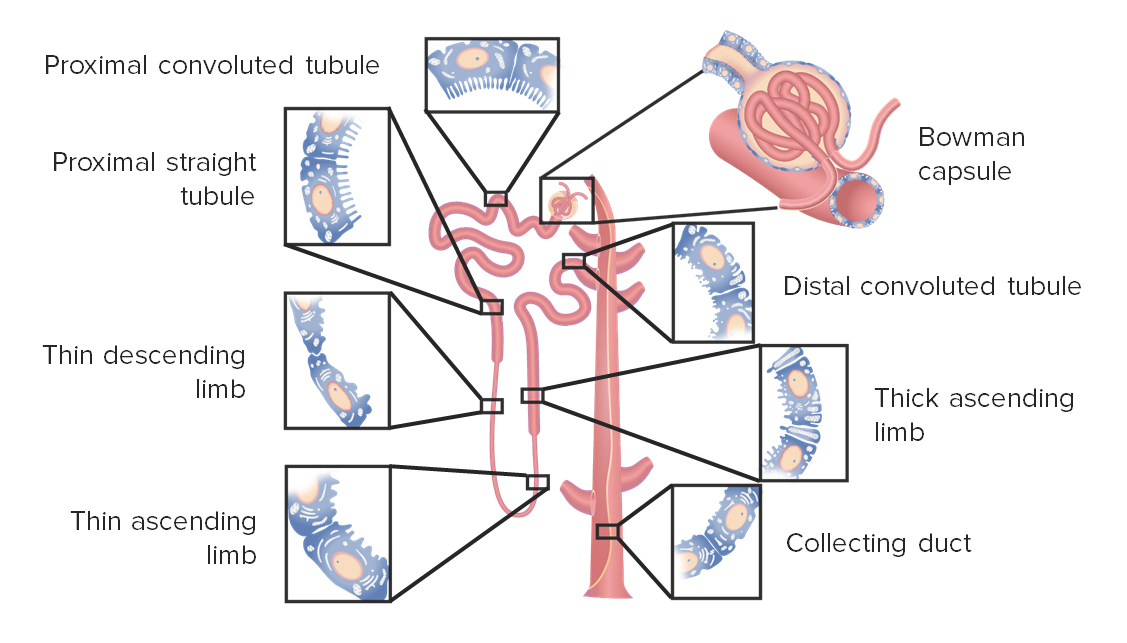
Segments of the nephron
Image by Lecturio.A specialized group of 3 cell types in close proximity to the glomerulus. The JGA plays an important role in maintaining blood pressure and fluid homeostasis Homeostasis The processes whereby the internal environment of an organism tends to remain balanced and stable. Cell Injury and Death.
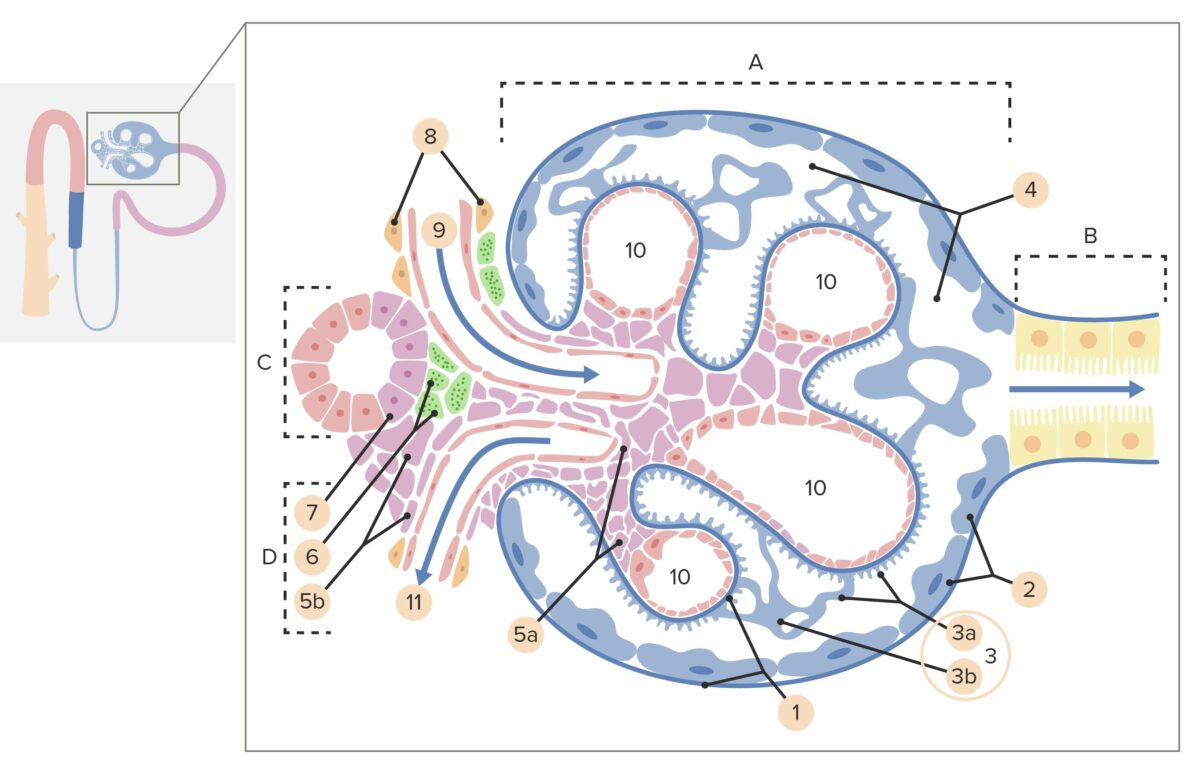
Structure of a renal corpuscle and the juxtaglomerular apparatus:
A: Renal corpuscle
B: Proximal tubule
C: Distal convoluted tube
D: Juxtaglomerular apparatus
1: Basement membrane
2: Bowman capsule, parietal layer
3: Bowman capsule, visceral layer
3a: Podocyte pedicles
3b: Podocyte
4: Bowman space (urinary space)
5a: Mesangium—intraglomerular mesangial cells
5b: Mesangium—extraglomerular mesangial cells
6: Juxtaglomerular cells
7: Macula densa
8: Myocytes (cells of smooth muscle)
9: Afferent arteriole
10: Glomerulus capillaries
11: Efferent arteriole.
Nephrons are divided into cortical and juxtamedullary nephrons based on their location.
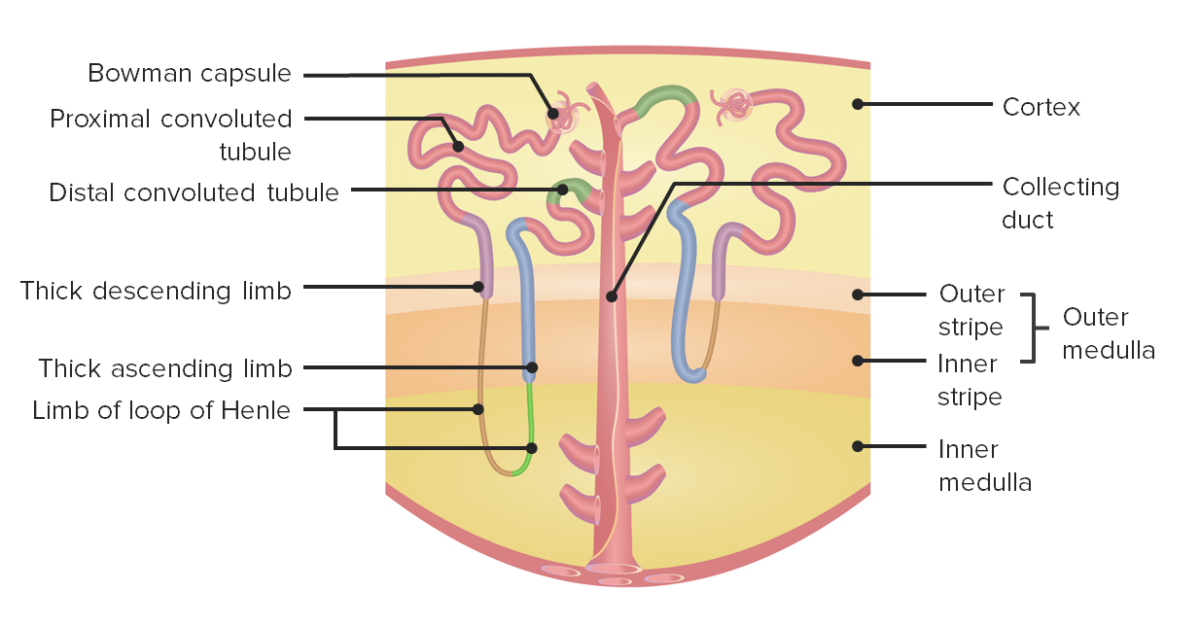
Nephron anatomy:
The left side shows a juxtamedullary nephron, while the right side shows a cortical nephron.
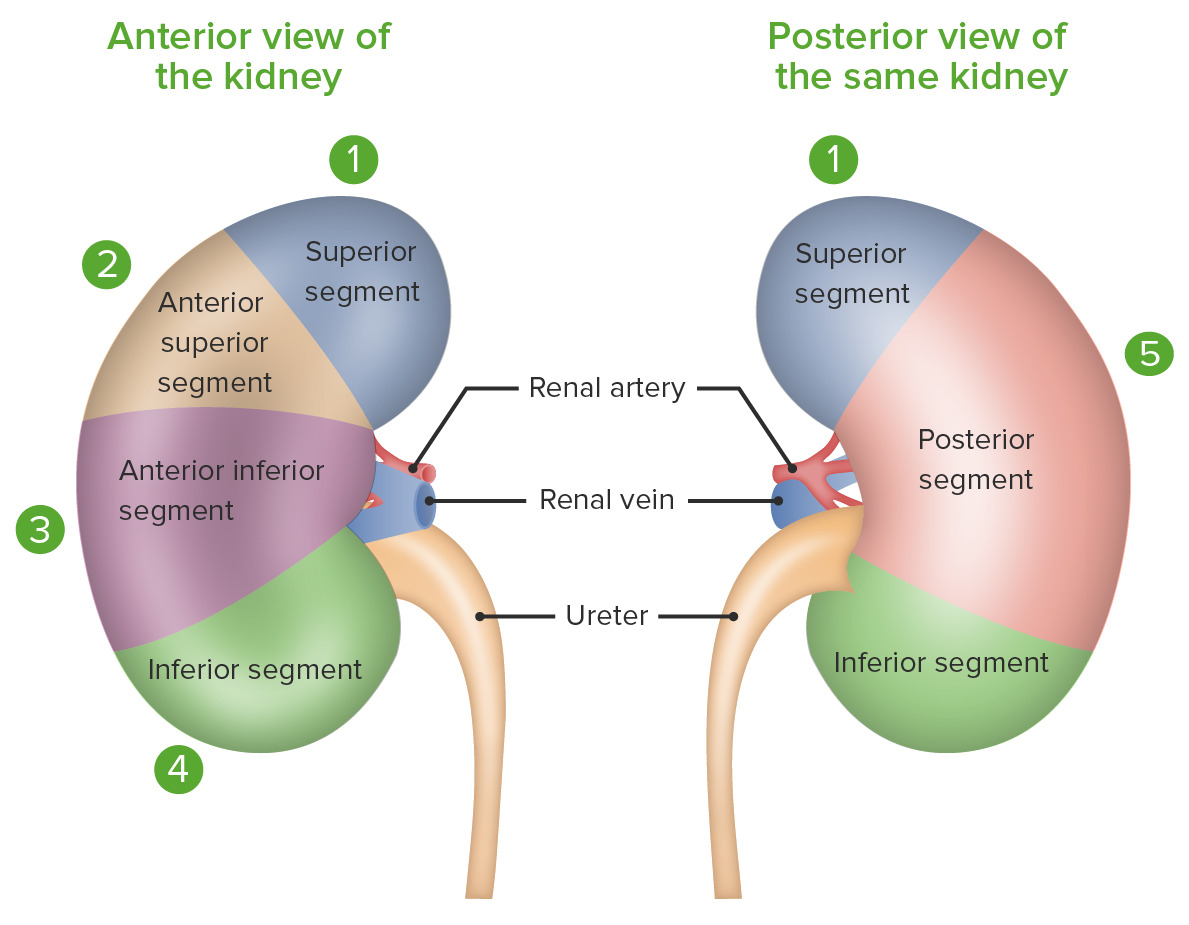
Segments of the kidney
Image by Lecturio.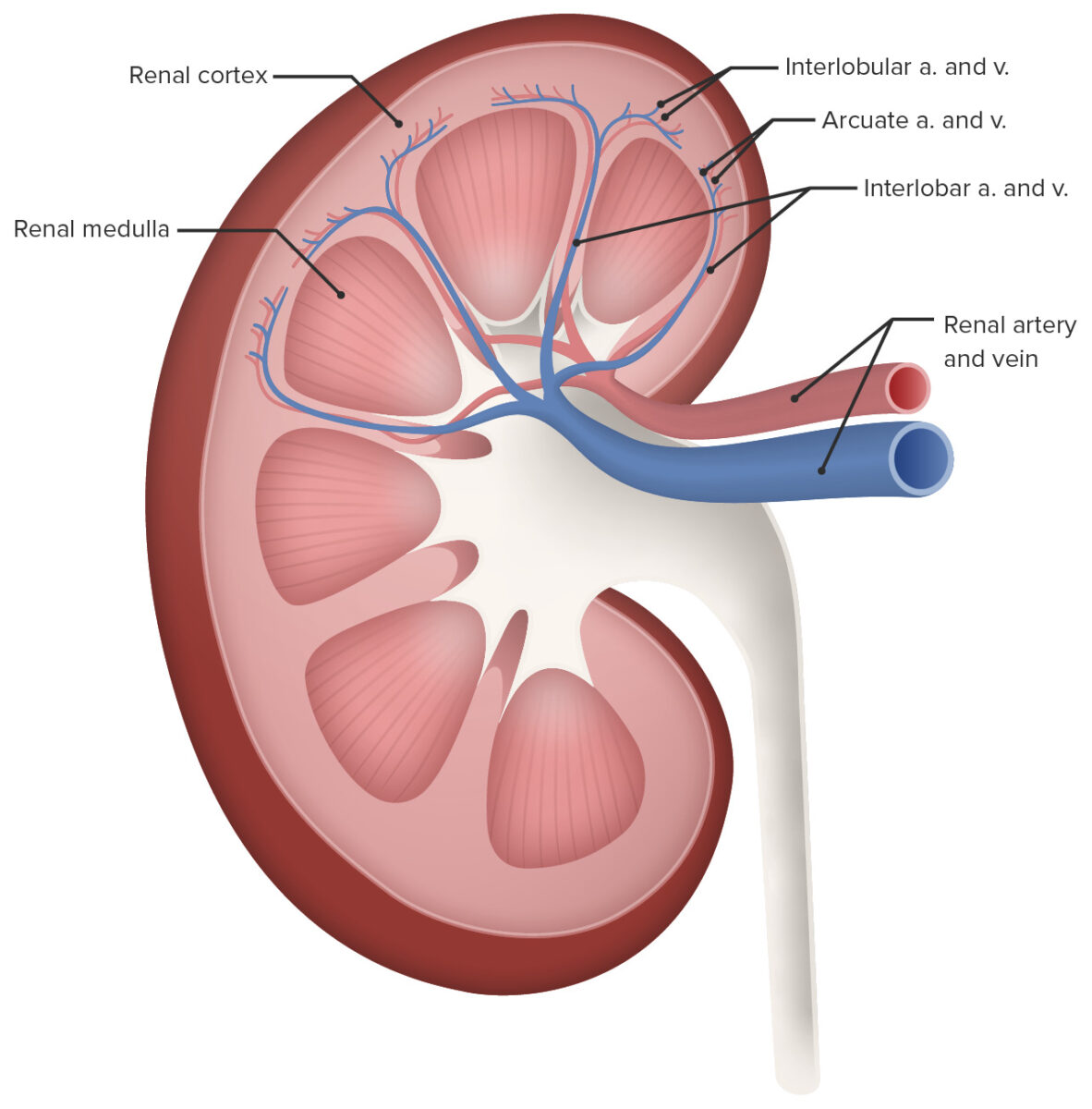
Renal circulation
Image by Lecturio.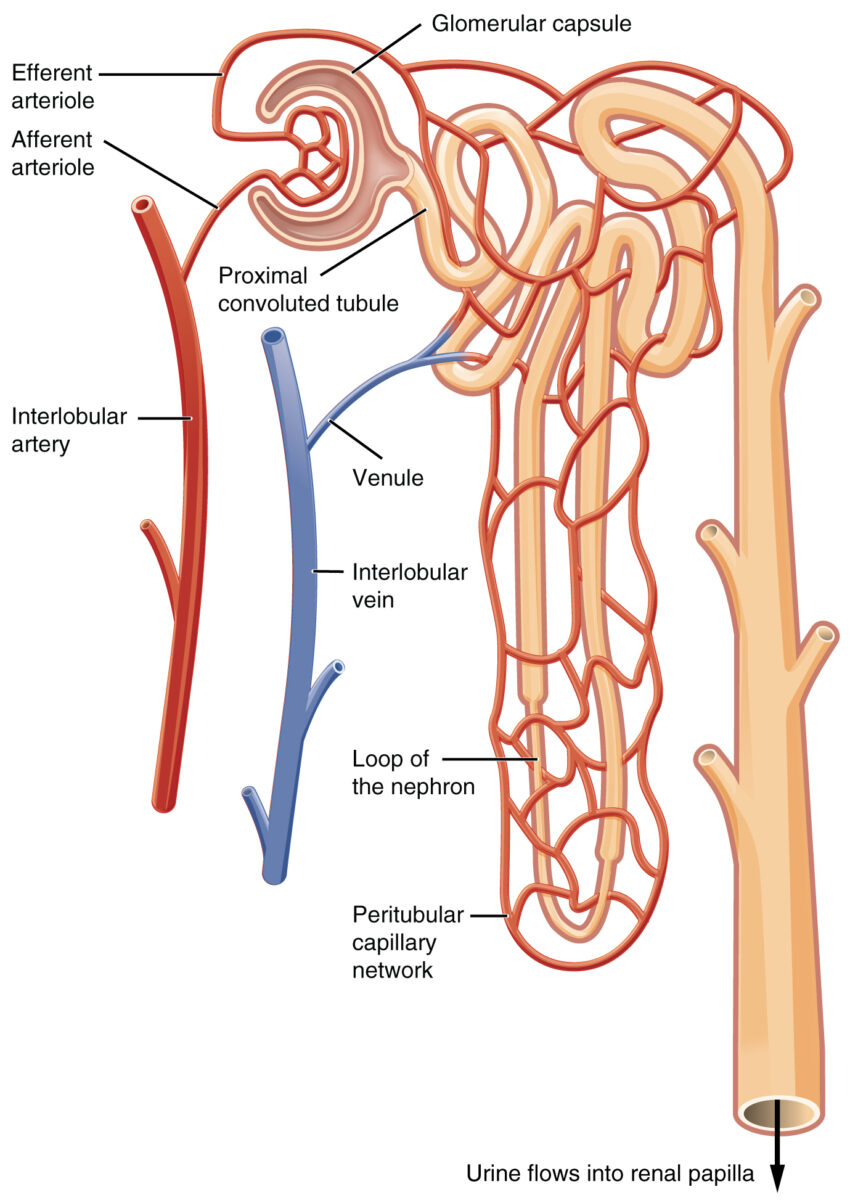
Blood flow within the nephron
Image: “The two capillary beds” by Phil Schatz. License: CC BY 4.0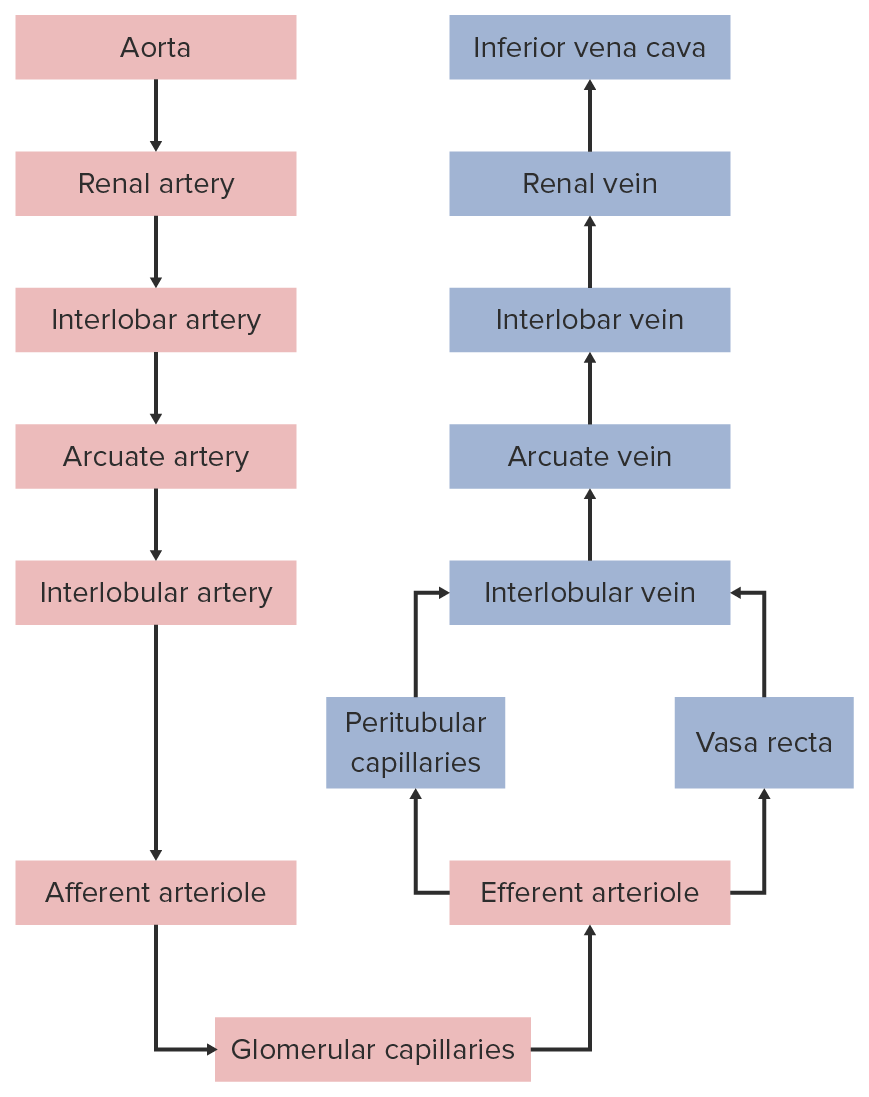
Renal circulation
Image by Lecturio.Renal innervation includes both afferent Afferent Neurons which conduct nerve impulses to the central nervous system. Nervous System: Histology and efferent Efferent Neurons which send impulses peripherally to activate muscles or secretory cells. Nervous System: Histology nerves through the renal nerve plexus. Innervation is via the autonomic nervous system Autonomic nervous system The ANS is a component of the peripheral nervous system that uses both afferent (sensory) and efferent (effector) neurons, which control the functioning of the internal organs and involuntary processes via connections with the CNS. The ANS consists of the sympathetic and parasympathetic nervous systems. Autonomic Nervous System: Anatomy, primarily through sympathetic fibers:
Functions of the kidneys include: