Ketone bodies are an important source of energy and their metabolism is a tightly regulated process. When glucose reserves in the body run low, more fatty acids are made available to the liver for oxidation, leading to the consequent production of energy-rich molecules, most notably acetyl-CoA. Acetyl-CoA can either enter the citric acid cycle in the liver or be used for the synthesis of ketone bodies. The ketone bodies can then travel via the blood throughout the body. Cells (especially in skeletal muscle and the brain) can then convert the ketone bodies back into acetyl-CoA, which can enter the citric acid cycle to produce ATP. Ketone bodies are a way for the body to use the energy stored in fat when glucose is unavailable or unable to be used.
Last updated: Apr 17, 2025
Acetone, a ketone body
Image: “Skeletal formula of acetone” by Fvasconcellos. License: Public Domain
Acetoacetic acid, a ketone body
Image: “Acetoacetic acid” by Jü. License: Public Domain
β-Hydroxybutyrate, a ketone body
Image: “Strukturformel von (R)-3-Hydroxybuttersäure” by Jü. License: Public DomainKetogenesis is the process of generating ketone bodies, which occurs in the mitochondria Mitochondria Semiautonomous, self-reproducing organelles that occur in the cytoplasm of all cells of most, but not all, eukaryotes. Each mitochondrion is surrounded by a double limiting membrane. The inner membrane is highly invaginated, and its projections are called cristae. Mitochondria are the sites of the reactions of oxidative phosphorylation, which result in the formation of ATP. They contain distinctive ribosomes, transfer RNAs; amino Acyl tRNA synthetases; and elongation and termination factors. Mitochondria depend upon genes within the nucleus of the cells in which they reside for many essential messenger RNAs. Mitochondria are believed to have arisen from aerobic bacteria that established a symbiotic relationship with primitive protoeukaryotes. The Cell: Organelles of hepatocytes Hepatocytes The main structural component of the liver. They are specialized epithelial cells that are organized into interconnected plates called lobules. Liver: Anatomy.
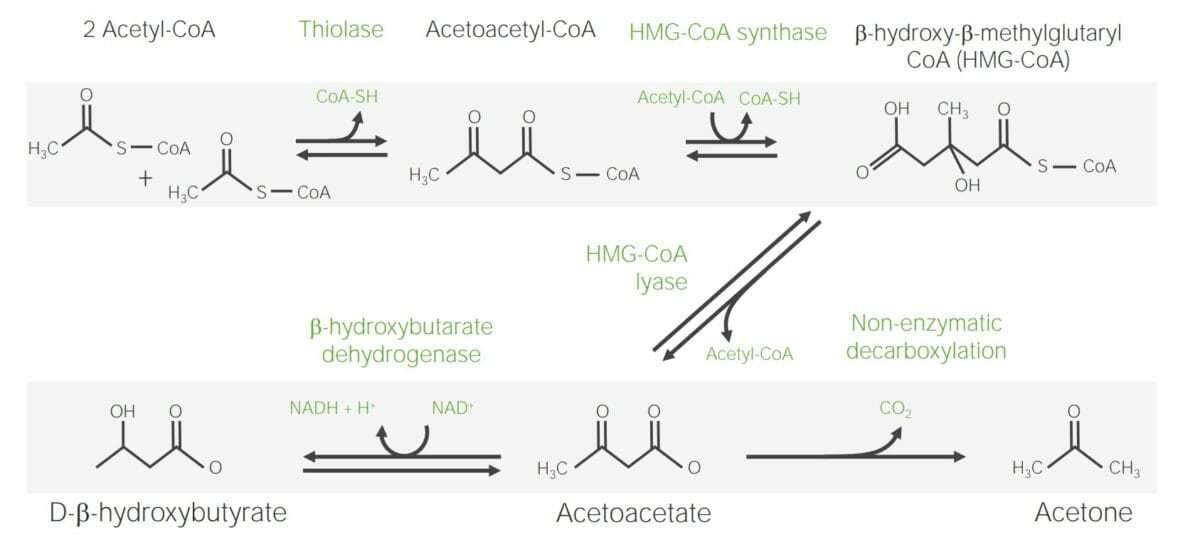
Steps required for the synthesis of ketone bodies
Image by Lecturio.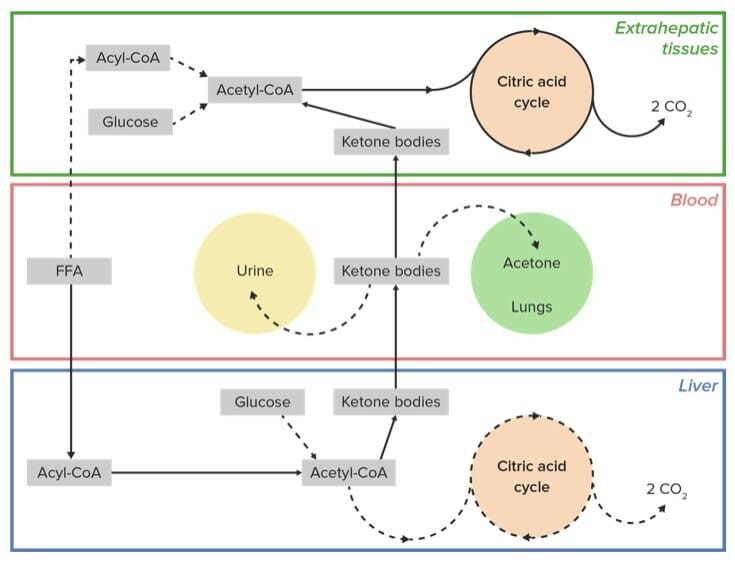
Citric acid cycle:
Free fatty acids (FFA) are brought to the liver (and some extrahepatic sites) where they are activated into fatty acyl-CoA chains and then broken down via β-oxidation into individual molecules of acetyl-CoA. When glucose is in limited supply, acetyl-CoA is converted into ketone bodies. Acetoacetate and β-hydroxybutyrate travel via the blood to the extrahepatic tissues where they are needed (e.g., muscle, brain) and converted back into acetyl-CoA, which then enters the citric acid cycle to generate ATP energy. Some acetoacetate undergoes nonenzymatic conversion into the ketone body acetone, which enters the blood and is exhaled by the lungs. Additional ketone bodies are excreted by the urine prior to reaching their target extrahepatic tissue.
FFA: free fatty acid
Solid line: primary pathway
Dotted line: Minor pathways