Inhaled anesthetics Anesthetics Agents that are capable of inducing a total or partial loss of sensation, especially tactile sensation and pain. They may act to induce general anesthesia, in which an unconscious state is achieved, or may act locally to induce numbness or lack of sensation at a targeted site. Anesthesiology: History and Basic Concepts are chemical compounds that can induce and maintain general anesthesia General anesthesia Procedure in which patients are induced into an unconscious state through use of various medications so that they do not feel pain during surgery. Anesthesiology: History and Basic Concepts when delivered by inhalation. Inhaled anesthetics Anesthetics Agents that are capable of inducing a total or partial loss of sensation, especially tactile sensation and pain. They may act to induce general anesthesia, in which an unconscious state is achieved, or may act locally to induce numbness or lack of sensation at a targeted site. Anesthesiology: History and Basic Concepts can be divided into 2 groups: volatile anesthetics Anesthetics Agents that are capable of inducing a total or partial loss of sensation, especially tactile sensation and pain. They may act to induce general anesthesia, in which an unconscious state is achieved, or may act locally to induce numbness or lack of sensation at a targeted site. Anesthesiology: History and Basic Concepts and gases. Volatile anesthetics Anesthetics Agents that are capable of inducing a total or partial loss of sensation, especially tactile sensation and pain. They may act to induce general anesthesia, in which an unconscious state is achieved, or may act locally to induce numbness or lack of sensation at a targeted site. Anesthesiology: History and Basic Concepts include halothane, isoflurane, desflurane, and sevoflurane. Nitrous oxide (N2O) is the most common of the anesthetic gases; cyclopropane and xenon are less commonly used. While the exact mechanism of action of the inhaled anesthetics Anesthetics Agents that are capable of inducing a total or partial loss of sensation, especially tactile sensation and pain. They may act to induce general anesthesia, in which an unconscious state is achieved, or may act locally to induce numbness or lack of sensation at a targeted site. Anesthesiology: History and Basic Concepts is unknown, the drugs are believed to have variable Variable Variables represent information about something that can change. The design of the measurement scales, or of the methods for obtaining information, will determine the data gathered and the characteristics of that data. As a result, a variable can be qualitative or quantitative, and may be further classified into subgroups. Types of Variables effects on GABA GABA The most common inhibitory neurotransmitter in the central nervous system. Receptors and Neurotransmitters of the CNS, glycine Glycine A non-essential amino acid. It is found primarily in gelatin and silk fibroin and used therapeutically as a nutrient. It is also a fast inhibitory neurotransmitter. Synthesis of Nonessential Amino Acids, glutamate Glutamate Derivatives of glutamic acid. Included under this heading are a broad variety of acid forms, salts, esters, and amides that contain the 2-aminopentanedioic acid structure. Synthesis of Nonessential Amino Acids, and NMDA receptors Receptors Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors in the CNS. Inhaled anesthetics Anesthetics Agents that are capable of inducing a total or partial loss of sensation, especially tactile sensation and pain. They may act to induce general anesthesia, in which an unconscious state is achieved, or may act locally to induce numbness or lack of sensation at a targeted site. Anesthesiology: History and Basic Concepts have been used for medical purposes for the last 200 years.
Last updated: Dec 15, 2025
| Agent | Characteristics | Minimum alveolar concentration (MAC) |
|---|---|---|
| Nitrous oxide (N2O) |
|
104% |
| Halothane |
|
0.75% |
| Desflurane |
|
6.6% |
| Sevoflurane |
|
1.8% |
| Isoflurane |
|
1.2% |
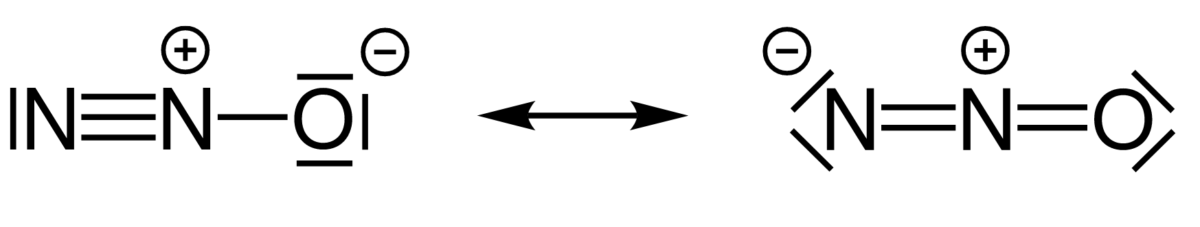
Structure of nitrous oxide (N2O)
Image: “Resonance structures of nitrous oxide” by Chem Sim 2001. License: Public Domain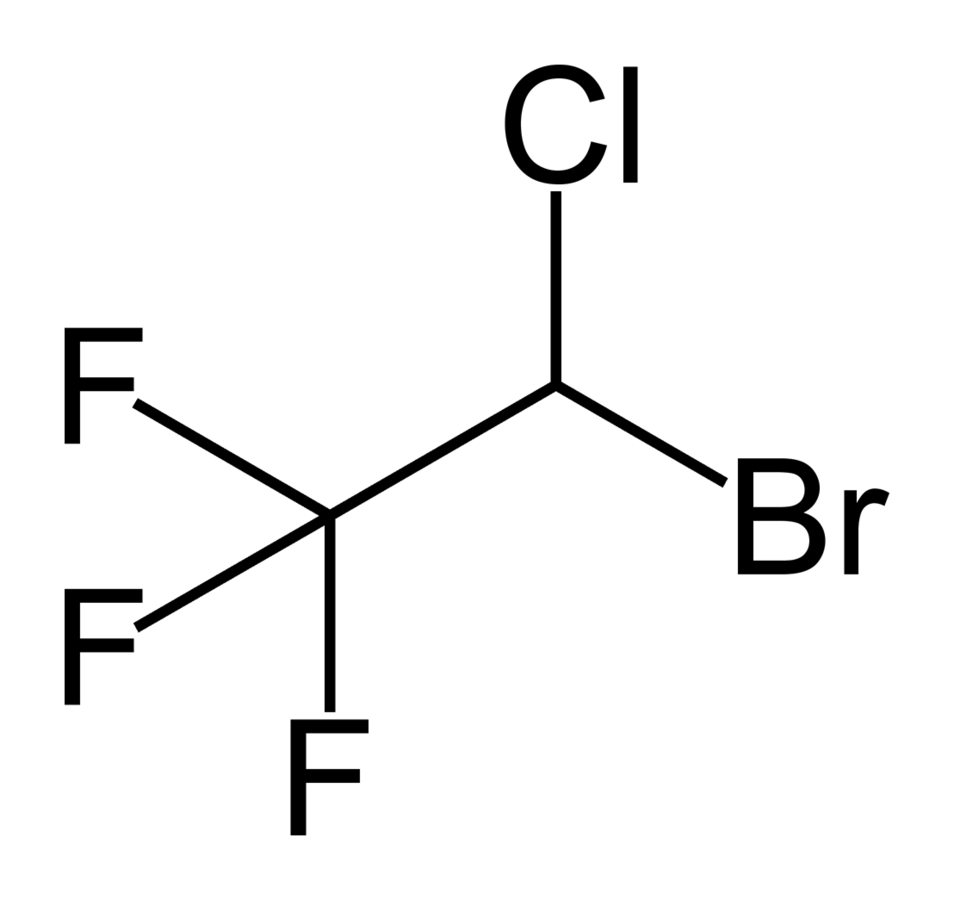
Structure of halothane
Image: “Halothane2” by Benjah-bmm27 . License: Public Domain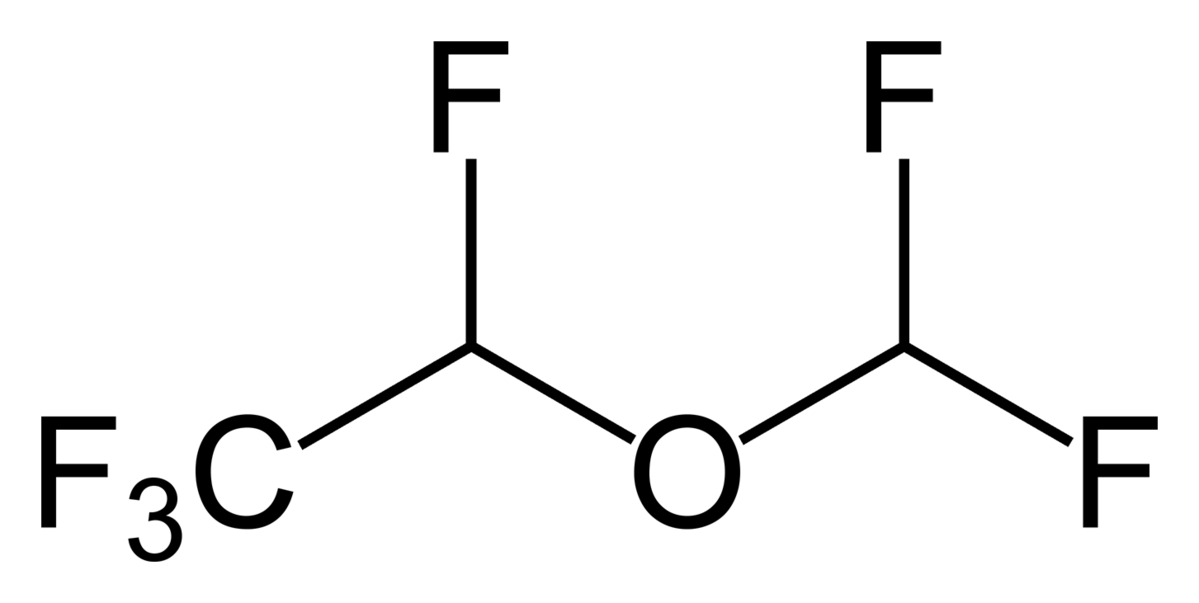
Structure of desflurane
Image: “Desflurane2” by Benjah-bmm27. License: Public Domain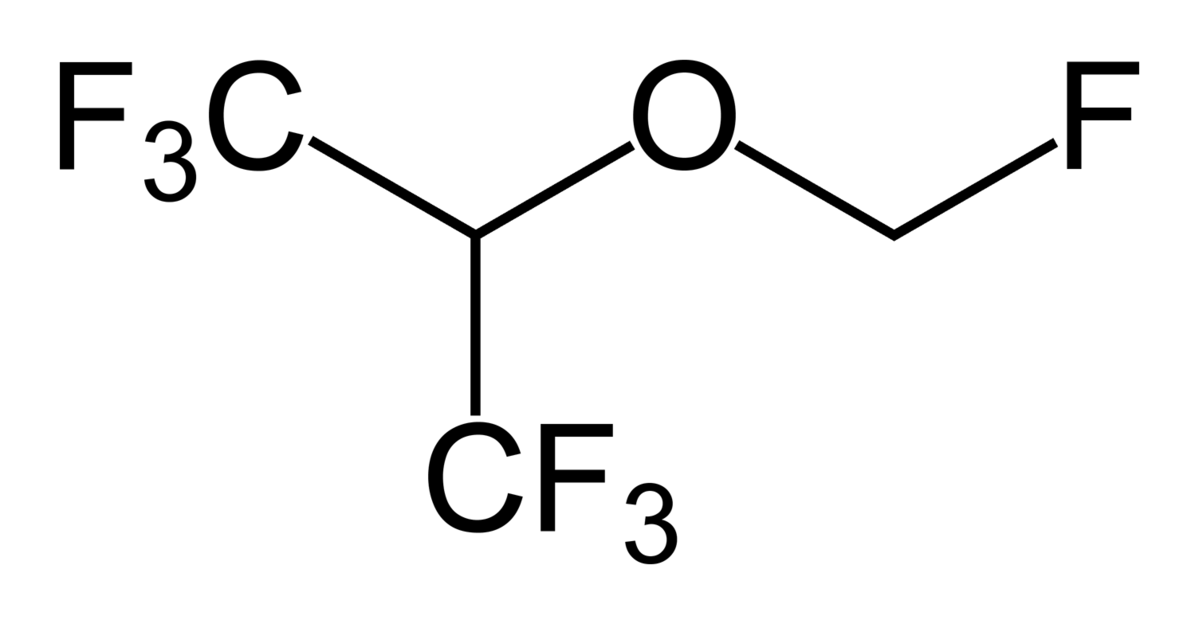
Structure of sevoflurane
Image: “Sevoflurane2” by Ben Mills. License: Public Domain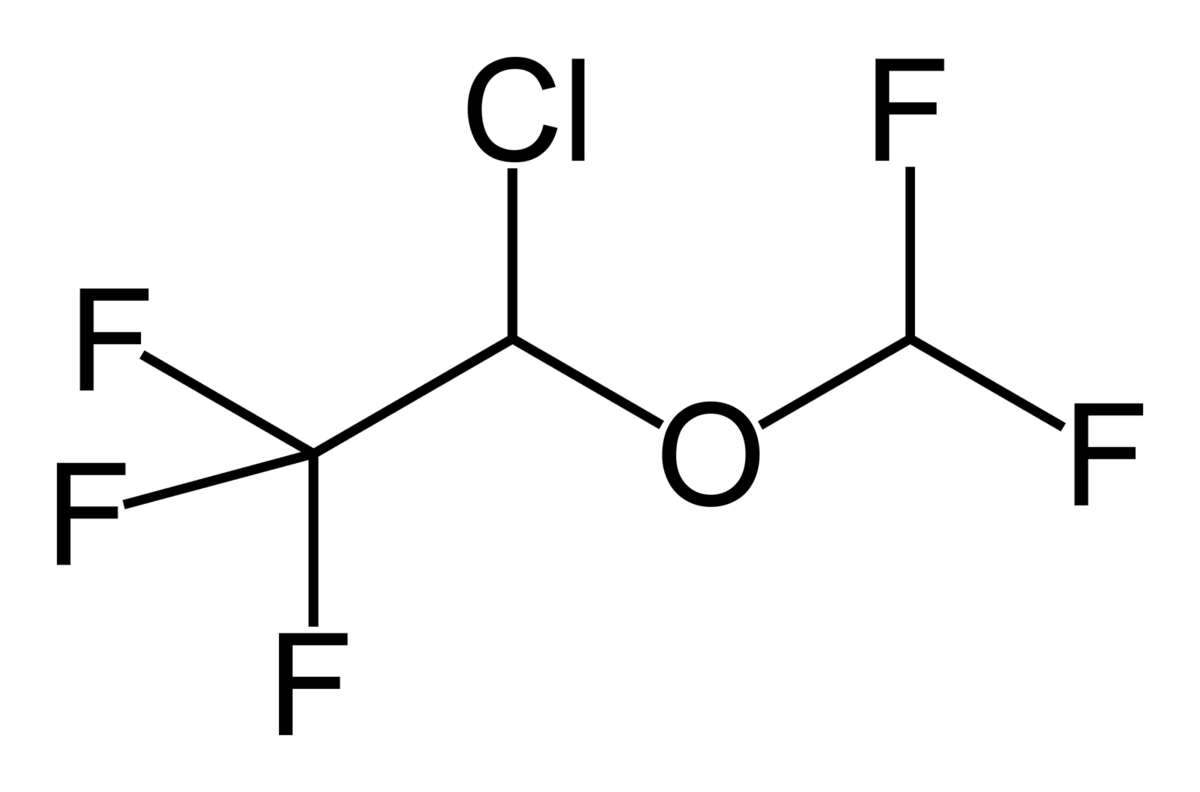
Structure of isoflurane
Image: “Isoflurane2” by Benjah-bmm27. License: Public DomainGeneral class effects (individual agents may have unique properties):
Administration by inhalation:
Delivery by anesthesia Anesthesia A state characterized by loss of feeling or sensation. This depression of nerve function is usually the result of pharmacologic action and is induced to allow performance of surgery or other painful procedures. Anesthesiology: History and Basic Concepts machine:
Inhaled anesthetic dosing:

Anesthesia machine
Image: “Datex – Ohmeda” by Kitmondo Marketplace. License: CC BY 2.0Partition coefficient (Ostwald coefficient):
Inspiratory concentration (FI):
Alveolar concentration (FA):
Partial pressure Partial pressure The pressure that would be exerted by one component of a mixture of gases if it were present alone in a container. Gas Exchange:
Effects of ventilation Ventilation The total volume of gas inspired or expired per unit of time, usually measured in liters per minute. Ventilation: Mechanics of Breathing rate:
Effects of cardiac output Cardiac output The volume of blood passing through the heart per unit of time. It is usually expressed as liters (volume) per minute so as not to be confused with stroke volume (volume per beat). Cardiac Mechanics:
Effects of pulmonary circulation Circulation The movement of the blood as it is pumped through the cardiovascular system. ABCDE Assessment:
Effects of concentration:
Summary of determinants of induction speed:
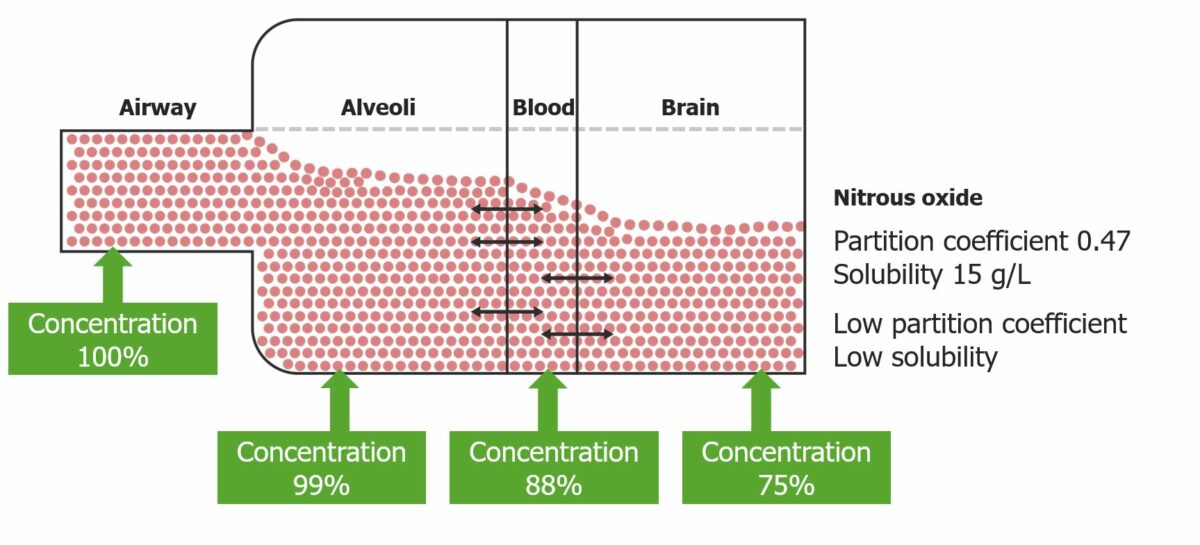
Graphic representation of the partition coefficient of nitrous oxide: Note the final concentration depends directly on the partition coefficient.
Image by Lecturio.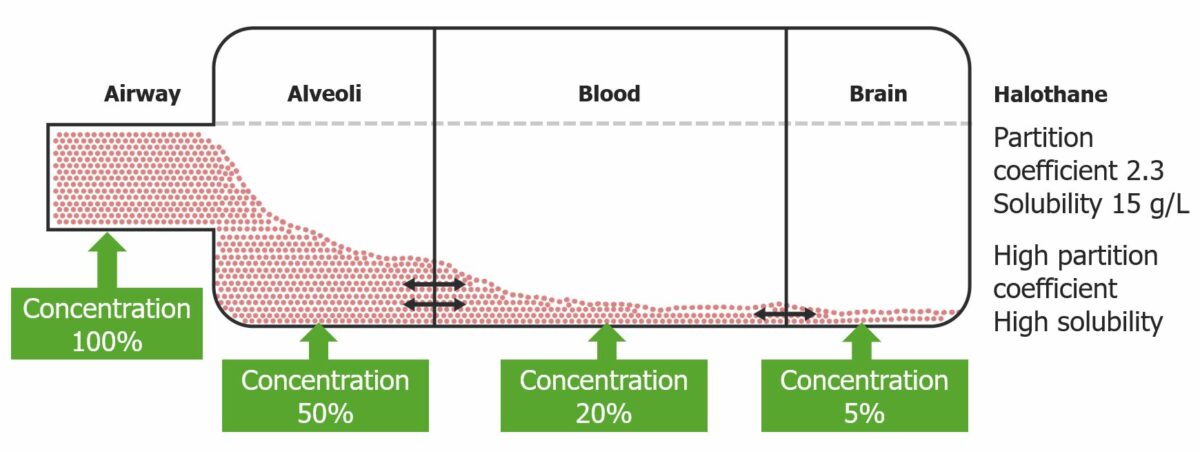
Graphic representation of the partition coefficient of halothane: Halothane has an increased solubility, which reduces the blood concentration.
Image by Lecturio.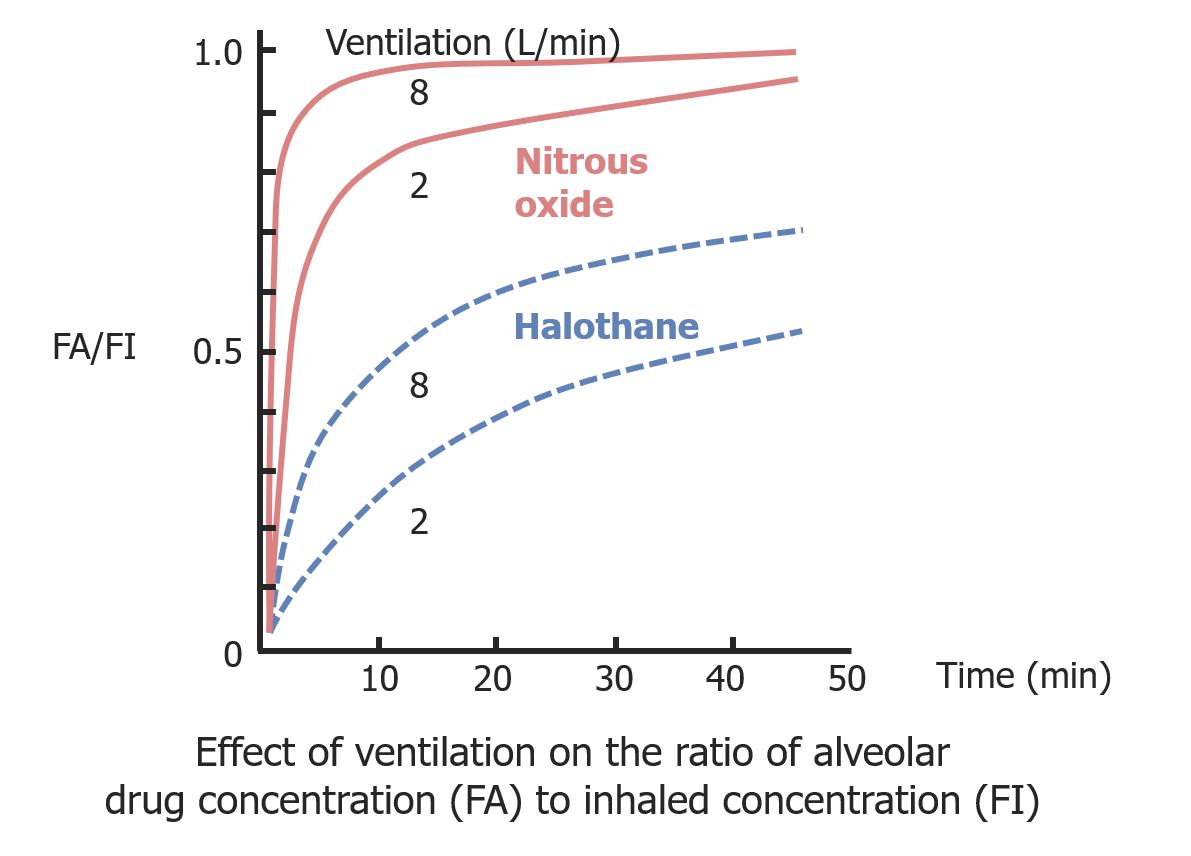
Effect of ventilation on the ratio of alveolar drug concentration (FA) to inhaled concentration (FI)
Image by Lecturio.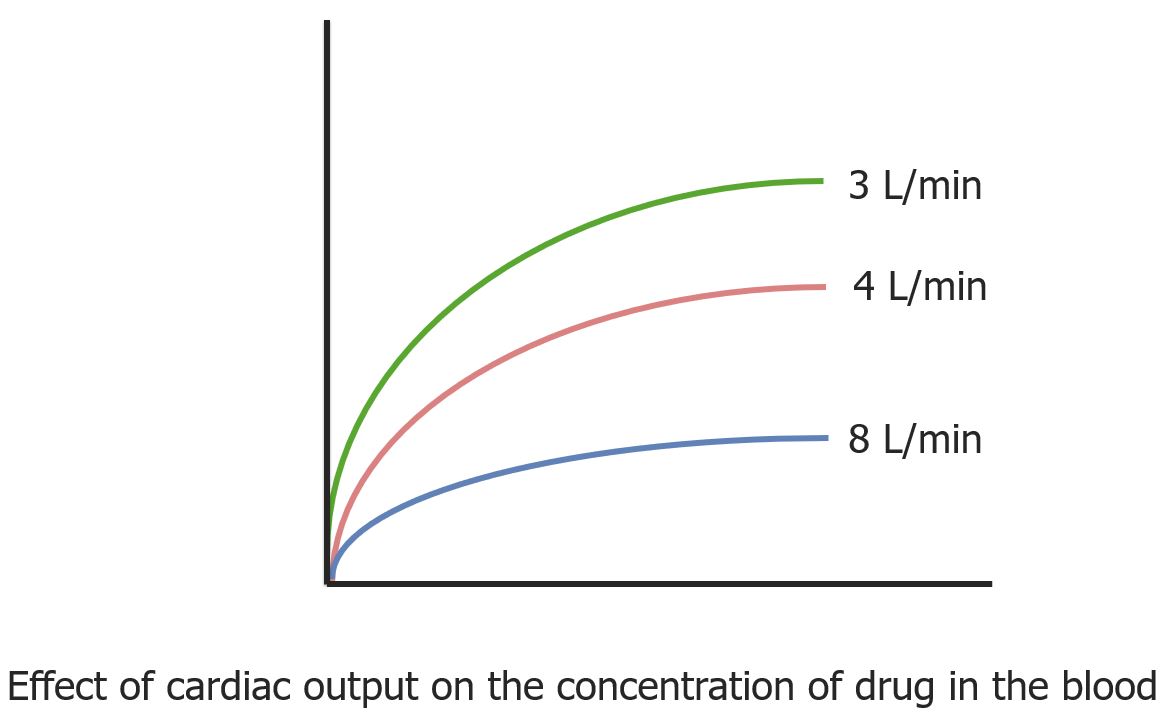
A diagram of the inverse relationship between drug concentration in the blood and cardiac output
Image by Lecturio.| Group | Organs | Description |
|---|---|---|
| Vessel-rich group | Brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification, heart, liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy, kidney, and endocrine organs |
|
| Muscle group | Skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions and muscles |
|
| Fat group | Adipose tissue Adipose tissue Adipose tissue is a specialized type of connective tissue that has both structural and highly complex metabolic functions, including energy storage, glucose homeostasis, and a multitude of endocrine capabilities. There are three types of adipose tissue, white adipose tissue, brown adipose tissue, and beige or “brite” adipose tissue, which is a transitional form. Adipose Tissue: Histology |
|
| Vessel-poor group | Bones, ligaments, teeth Teeth Normally, an adult has 32 teeth: 16 maxillary and 16 mandibular. These teeth are divided into 4 quadrants with 8 teeth each. Each quadrant consists of 2 incisors (dentes incisivi), 1 canine (dens caninus), 2 premolars (dentes premolares), and 3 molars (dentes molares). Teeth are composed of enamel, dentin, and dental cement. Teeth: Anatomy, hair, and cartilage Cartilage Cartilage is a type of connective tissue derived from embryonic mesenchyme that is responsible for structural support, resilience, and the smoothness of physical actions. Perichondrium (connective tissue membrane surrounding cartilage) compensates for the absence of vasculature in cartilage by providing nutrition and support. Cartilage: Histology |
|
| Agent | Advantages | Disadvantages |
|---|---|---|
| Nitrous oxide (N2O) |
|
|
| Isoflurane |
|
|
| Sevoflurane |
|
More expensive than isoflurane |
| Desflurane |
|
|
| Agent | Adverse effects |
|---|---|
| Nitrous oxide (N2O) |
|
| Halothane |
|
| Desflurane |
|
| Sevoflurane |
|
| Isoflurane |
|
| Agent | Contraindications Contraindications A condition or factor associated with a recipient that makes the use of a drug, procedure, or physical agent improper or inadvisable. Contraindications may be absolute (life threatening) or relative (higher risk of complications in which benefits may outweigh risks). Noninvasive Ventilation |
|---|---|
| Nitrous oxide (N2O) |
|
| Halothane | Unexplained liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy dysfunction after exposure in a previous procedure |
| Desflurane |
|
| Sevoflurane | |
| Isoflurane | Severe hypovolemia Hypovolemia Sepsis in Children |