Impetigo Impetigo Impetigo is a highly contagious superficial bacterial infection typically caused by Staphylococcus aureus (most common) and Streptococcus pyogenes. Impetigo most commonly presents in children aged 2 to 5 years with lesions that evolve from papules to vesicles to pustules, which eventually break down to form characteristic "honey-colored" crusts. Impetigo is a highly contagious superficial bacterial infection typically caused by Staphylococcus aureus Staphylococcus aureus Potentially pathogenic bacteria found in nasal membranes, skin, hair follicles, and perineum of warm-blooded animals. They may cause a wide range of infections and intoxications. Brain Abscess (most common) and Streptococcus Streptococcus Streptococcus is one of the two medically important genera of gram-positive cocci, the other being Staphylococcus. Streptococci are identified as different species on blood agar on the basis of their hemolytic pattern and sensitivity to optochin and bacitracin. There are many pathogenic species of streptococci, including S. pyogenes, S. agalactiae, S. pneumoniae, and the viridans streptococci. Streptococcus pyogenes. Impetigo Impetigo Impetigo is a highly contagious superficial bacterial infection typically caused by Staphylococcus aureus (most common) and Streptococcus pyogenes. Impetigo most commonly presents in children aged 2 to 5 years with lesions that evolve from papules to vesicles to pustules, which eventually break down to form characteristic "honey-colored" crusts. Impetigo most commonly presents in children aged 2 to 5 years with lesions that evolve from papules to vesicles Vesicles Female Genitourinary Examination to pustules, which eventually break down to form characteristic “honey-colored” crusts. Infection can either be primary (bacterial infection of healthy, intact skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions) or secondary (infection of pre-existing abrasions Abrasions Corneal Abrasions, Erosion, and Ulcers). The diagnosis is clinical, and management includes topical or systemic antibiotic therapy. Complications of impetigo Impetigo Impetigo is a highly contagious superficial bacterial infection typically caused by Staphylococcus aureus (most common) and Streptococcus pyogenes. Impetigo most commonly presents in children aged 2 to 5 years with lesions that evolve from papules to vesicles to pustules, which eventually break down to form characteristic "honey-colored" crusts. Impetigo include post-streptococcal glomerulonephritis, cellulitis Cellulitis Cellulitis is a common infection caused by bacteria that affects the dermis and subcutaneous tissue of the skin. It is frequently caused by Staphylococcus aureus and Streptococcus pyogenes. The skin infection presents as an erythematous and edematous area with warmth and tenderness. Cellulitis, and scarlet fever Scarlet fever Infection with group a Streptococci that is characterized by tonsillitis and pharyngitis. An erythematous rash is commonly present. Scarlet Fever.
Last updated: Dec 15, 2025
There are 3 variants of impetigo Impetigo Impetigo is a highly contagious superficial bacterial infection typically caused by Staphylococcus aureus (most common) and Streptococcus pyogenes. Impetigo most commonly presents in children aged 2 to 5 years with lesions that evolve from papules to vesicles to pustules, which eventually break down to form characteristic “honey-colored” crusts. Impetigo:

Crusted non-bullous impetigo on the upper extremity of a pediatric patient
Image: “ Impetigo” by Saint Louis University, Cardinal Glennon Children’s Hospital, 1465 South Grand Avenue, St. Louis, MO 63104, USA. License: CC BY 4.0
A child with honey-colored crust due to impetigo
Image: “OSC Microbio 21 02 impetigo” by CNX OpenStax. License: CC BY 4.0
Bullous impetigo on the gluteal region of an infected infant
Image: “Skin lesions that proved to be impetigo” by US Department of Health and Human Services. License: Public Domain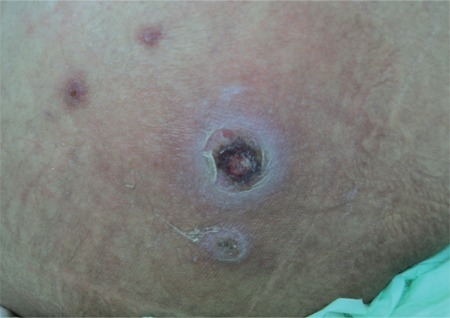
Coin-sized crusted ulcer typical of ecthyma (fusariosis is a fungal mold infection caused by Fusarium spp.)
Image: “Ectyhma gangrenosum” by İstanbul University Cerrahpasa Medical Faculty, Infectious Diseases and Clinical Microbiology İstanbul, Turkey. License: CC BY 2.5Diagnosis is usually clinical, based on the natural sequence of the lesions and the presence of honey-colored crusts on pediatric patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship aged 2–5 years.[5,6]
Management depends on the type and severity of the infection. Recommendations are based on current US and UK guidelines.
| Antibiotic | Adult dosage Dosage Dosage Calculation | Pediatric dosage Dosage Dosage Calculation | |
|---|---|---|---|
| Methicillin-sensitive Staphylococcus Staphylococcus Staphylococcus is a medically important genera of Gram-positive, aerobic cocci. These bacteria form clusters resembling grapes on culture plates. Staphylococci are ubiquitous for humans, and many strains compose the normal skin flora. Staphylococcus and Streptococcus Streptococcus Streptococcus is one of the two medically important genera of gram-positive cocci, the other being Staphylococcus. Streptococci are identified as different species on blood agar on the basis of their hemolytic pattern and sensitivity to optochin and bacitracin. There are many pathogenic species of streptococci, including S. pyogenes, S. agalactiae, S. pneumoniae, and the viridans streptococci. Streptococcus (no penicillin Penicillin Rheumatic Fever allergy Allergy An abnormal adaptive immune response that may or may not involve antigen-specific IgE Type I Hypersensitivity Reaction) | Dicloxacillin Dicloxacillin One of the penicillins which is resistant to penicillinase. Penicillins | 250‒500 mg by mouth 4x a day | 6.25‒12.5 mg/kg/dose 4x a day |
| Flucloxacillin (UK) | 250‒500 mg 4x a day | ||
| Amoxicillin Amoxicillin A broad-spectrum semisynthetic antibiotic similar to ampicillin except that its resistance to gastric acid permits higher serum levels with oral administration. Penicillins–clavulanate | 875/125 mg 2x a day | 25 mg/kg/day (based on amoxicillin Amoxicillin A broad-spectrum semisynthetic antibiotic similar to ampicillin except that its resistance to gastric acid permits higher serum levels with oral administration. Penicillins) in 2 divided doses | |
| Cephalexin | 250 mg 4x a day | 25–50 mg/kg/day in 3–4 divided doses | |
| Methicillin-sensitive Staphylococcus Staphylococcus Staphylococcus is a medically important genera of Gram-positive, aerobic cocci. These bacteria form clusters resembling grapes on culture plates. Staphylococci are ubiquitous for humans, and many strains compose the normal skin flora. Staphylococcus and Streptococcus Streptococcus Streptococcus is one of the two medically important genera of gram-positive cocci, the other being Staphylococcus. Streptococci are identified as different species on blood agar on the basis of their hemolytic pattern and sensitivity to optochin and bacitracin. There are many pathogenic species of streptococci, including S. pyogenes, S. agalactiae, S. pneumoniae, and the viridans streptococci. Streptococcus (with penicillin Penicillin Rheumatic Fever allergy Allergy An abnormal adaptive immune response that may or may not involve antigen-specific IgE Type I Hypersensitivity Reaction) | Erythromycin Erythromycin A bacteriostatic antibiotic macrolide produced by streptomyces erythreus. Erythromycin a is considered its major active component. In sensitive organisms, it inhibits protein synthesis by binding to 50s ribosomal subunits. This binding process inhibits peptidyl transferase activity and interferes with translocation of amino acids during translation and assembly of proteins. Macrolides and Ketolides | 250 mg 4x a day | 40 mg/kg/day in 3–4 divided doses |
| Clindamycin Clindamycin An antibacterial agent that is a semisynthetic analog of lincomycin. Lincosamides | 300–450 mg 4x a day | 20 mg/kg/day in 3 divided doses | |
| MRSA MRSA A strain of Staphylococcus aureus that is non-susceptible to the action of methicillin. The mechanism of resistance usually involves modification of normal or the presence of acquired penicillin binding proteins. Staphylococcus | Doxycycline | 100 mg 2x a day | > 8 years: 2.2 mg/kg/dose every 12 hours |
| Clindamycin Clindamycin An antibacterial agent that is a semisynthetic analog of lincomycin. Lincosamides | 300–450 mg 4x a day | 20 mg/kg/day in 3 divided doses | |
| Trimethoprim Trimethoprim The sulfonamides are a class of antimicrobial drugs inhibiting folic acid synthesize in pathogens. The prototypical drug in the class is sulfamethoxazole. Although not technically sulfonamides, trimethoprim, dapsone, and pyrimethamine are also important antimicrobial agents inhibiting folic acid synthesis. The agents are often combined with sulfonamides, resulting in a synergistic effect. Sulfonamides and Trimethoprim– sulfamethoxazole Sulfamethoxazole A bacteriostatic antibacterial agent that interferes with folic acid synthesis in susceptible bacteria. Its broad spectrum of activity has been limited by the development of resistance. Sulfonamides and Trimethoprim | 1–2 double-strength tablets 2x a day | 8–12 mg/kg (based on trimethoprim Trimethoprim The sulfonamides are a class of antimicrobial drugs inhibiting folic acid synthesize in pathogens. The prototypical drug in the class is sulfamethoxazole. Although not technically sulfonamides, trimethoprim, dapsone, and pyrimethamine are also important antimicrobial agents inhibiting folic acid synthesis. The agents are often combined with sulfonamides, resulting in a synergistic effect. Sulfonamides and Trimethoprim) in 2 divided doses |
Skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions hygiene measures[5]
The following conditions also present with bullae Bullae Erythema Multiforme and serve as differential diagnoses for bullous impetigo Bullous Impetigo Impetigo:
The following conditions are other types of superficial skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease that are included in the differential diagnoses of impetigo Impetigo Impetigo is a highly contagious superficial bacterial infection typically caused by Staphylococcus aureus (most common) and Streptococcus pyogenes. Impetigo most commonly presents in children aged 2 to 5 years with lesions that evolve from papules to vesicles to pustules, which eventually break down to form characteristic “honey-colored” crusts. Impetigo:
Diagnosis Codes:
These codes are used to diagnose
impetigo
Impetigo
Impetigo is a highly contagious superficial bacterial infection typically caused by Staphylococcus aureus (most common) and Streptococcus pyogenes. Impetigo most commonly presents in children aged 2 to 5 years with lesions that evolve from papules to vesicles to pustules, which eventually break down to form characteristic “honey-colored” crusts.
Impetigo, a common and highly contagious
skin
Skin
The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue.
Skin: Structure and Functions infection. The codes differentiate between the non-bullous (crusted) and bullous (blistering) forms.
| Coding System | Code | Description |
|---|---|---|
| ICD-10-CM | L01.00 | Impetigo Impetigo Impetigo is a highly contagious superficial bacterial infection typically caused by Staphylococcus aureus (most common) and Streptococcus pyogenes. Impetigo most commonly presents in children aged 2 to 5 years with lesions that evolve from papules to vesicles to pustules, which eventually break down to form characteristic “honey-colored” crusts. Impetigo, unspecified |
| ICD-10-CM | L01.01 | Non-bullous impetigo Non-Bullous Impetigo Impetigo |
| ICD-10-CM | L01.02 | Bullous impetigo Bullous Impetigo Impetigo |
Medications:
These codes are for the primary treatments for
impetigo
Impetigo
Impetigo is a highly contagious superficial bacterial infection typically caused by Staphylococcus aureus (most common) and Streptococcus pyogenes. Impetigo most commonly presents in children aged 2 to 5 years with lesions that evolve from papules to vesicles to pustules, which eventually break down to form characteristic “honey-colored” crusts.
Impetigo. Topical mupirocin is used for localized
infections
Infections
Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases.
Chronic Granulomatous Disease, while oral antibiotics like cephalexin are used for more widespread cases.
| Coding System | Code | Description |
|---|---|---|
| RxNorm | 7050 | Mupirocin (ingredient) |
| RxNorm | 2244 | Cephalexin (ingredient) |
| ATC | D06AX09 | Mupirocin |