Worldwide, the most frequent cause of death is heart disease. Thus, the common conditions that are evaluated in healthcare facilities are often related to the heart or the cardiovascular system: hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension, atherosclerotic disease, and heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR). In radiologic terms, this region is likely the most frequently studied aspect of human anatomy in healthcare delivery settings. Multiple methods are used, including X-ray X-ray Penetrating electromagnetic radiation emitted when the inner orbital electrons of an atom are excited and release radiant energy. X-ray wavelengths range from 1 pm to 10 nm. Hard x-rays are the higher energy, shorter wavelength x-rays. Soft x-rays or grenz rays are less energetic and longer in wavelength. The short wavelength end of the x-ray spectrum overlaps the gamma rays wavelength range. The distinction between gamma rays and x-rays is based on their radiation source. Pulmonary Function Tests, CT, MRI, echocardiography Echocardiography Ultrasonic recording of the size, motion, and composition of the heart and surrounding tissues. The standard approach is transthoracic. Tricuspid Valve Atresia (TVA), nuclear imaging Nuclear Imaging Nuclear imaging is the radiologic examination using radiopharmaceuticals, which are radioactive substances taken up by specific types of cells. Nuclear medicine is more concerned with the functional and molecular aspects of the organ or pathology being investigated rather than the structure. Nuclear Imaging, and angiography Angiography Radiography of blood vessels after injection of a contrast medium. Cardiac Surgery. Each test has its advantages and disadvantages and is obtained on the basis of the clinical presentation, acuity of symptoms, and risks and benefits to the patient. It is important to know the roles of imaging studies to help determine the proper treatment.
Last updated: Jan 17, 2024
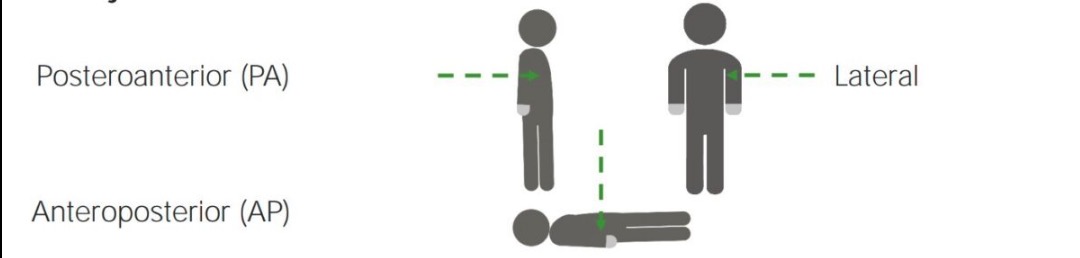
Different standard projections:
Chest X-rays can be taken from multiple directions, called “views.” Each view has benefits and drawbacks for different pathologies. The 3 common views are posteroanterior, anteroposterior, and lateral.
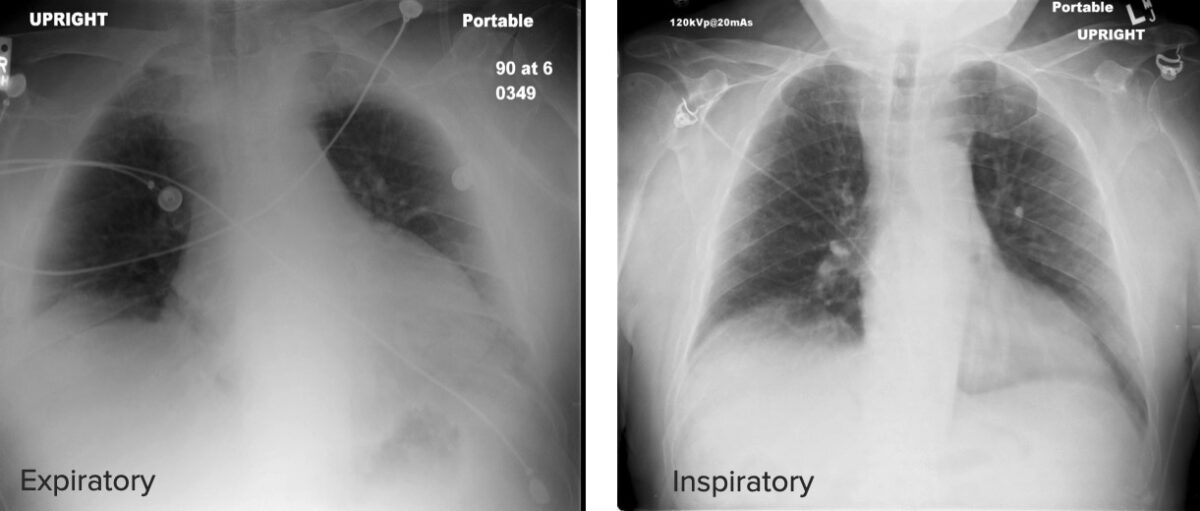
Differences between an expiratory and an inspiratory chest X-ray:
Note that in the inspiratory X-ray, the posterior ribs and the pulmonary parenchyma are more easily seen, while in the expiratory X-ray, the parenchyma looks hazy and lacks definition.
The following structures must be identified and checked for abnormalities in size or shape:

Posteroanterior projection of the chest identifying the mediastinal structures:
PA: pulmonary artery
SVC: superior vena cava

Lateral projection of the chest identifying the mediastinal structures
Image by Hetal Verma.| Cause | Observation |
|---|---|
| Rotation Rotation Motion of an object in which either one or more points on a line are fixed. It is also the motion of a particle about a fixed point. X-rays | The shadow of the heart appears bigger in the projection because of the rotation Rotation Motion of an object in which either one or more points on a line are fixed. It is also the motion of a particle about a fixed point. X-rays of the subject to either side. |
| Suboptimal inspiration Inspiration Ventilation: Mechanics of Breathing | The diaphragm Diaphragm The diaphragm is a large, dome-shaped muscle that separates the thoracic cavity from the abdominal cavity. The diaphragm consists of muscle fibers and a large central tendon, which is divided into right and left parts. As the primary muscle of inspiration, the diaphragm contributes 75% of the total inspiratory muscle force. Diaphragm: Anatomy moves upward and compresses the heart. |
| Portable supine film | Cardiac silhouette undergoes magnification because the cassette is placed in contact with the posterior aspect of the patient and the X-ray X-ray Penetrating electromagnetic radiation emitted when the inner orbital electrons of an atom are excited and release radiant energy. X-ray wavelengths range from 1 pm to 10 nm. Hard x-rays are the higher energy, shorter wavelength x-rays. Soft x-rays or grenz rays are less energetic and longer in wavelength. The short wavelength end of the x-ray spectrum overlaps the gamma rays wavelength range. The distinction between gamma rays and x-rays is based on their radiation source. Pulmonary Function Tests beam penetrates from the anterior aspect. |
| Pectus excavatum Pectus Excavatum Cardiovascular Examination | The heart is compressed between the sternum Sternum A long, narrow, and flat bone commonly known as breastbone occurring in the midsection of the anterior thoracic segment or chest region, which stabilizes the rib cage and serves as the point of origin for several muscles that move the arms, head, and neck. Chest Wall: Anatomy and the spine Spine The human spine, or vertebral column, is the most important anatomical and functional axis of the human body. It consists of 7 cervical vertebrae, 12 thoracic vertebrae, and 5 lumbar vertebrae and is limited cranially by the skull and caudally by the sacrum. Vertebral Column: Anatomy. |
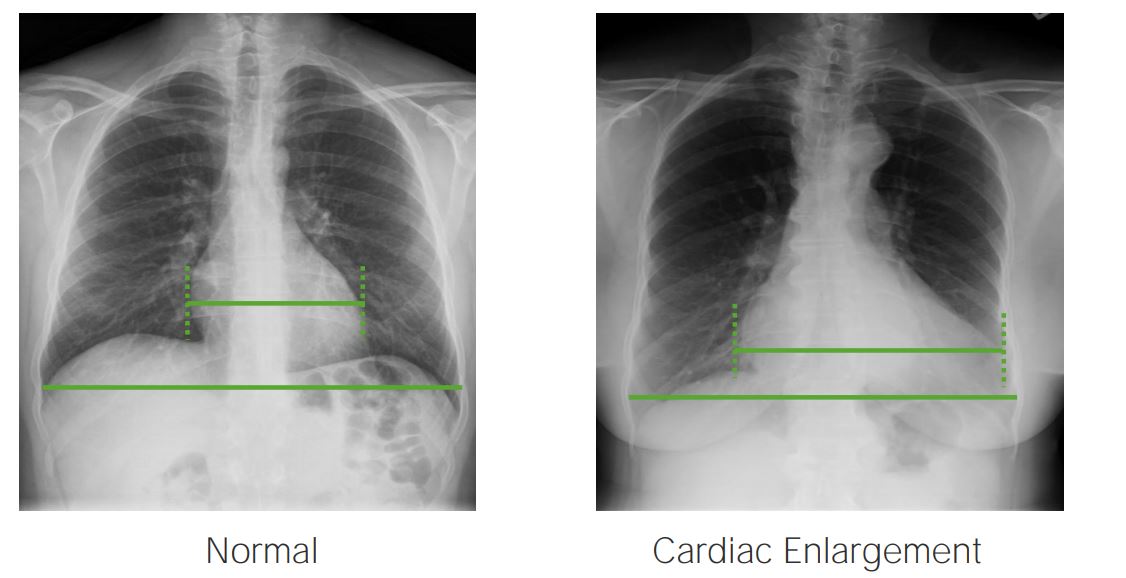
Left: Normal index (< 50%)
Right: Cardiac index > 50%, indicative of cardiac enlargement. Image by Hetal Verma.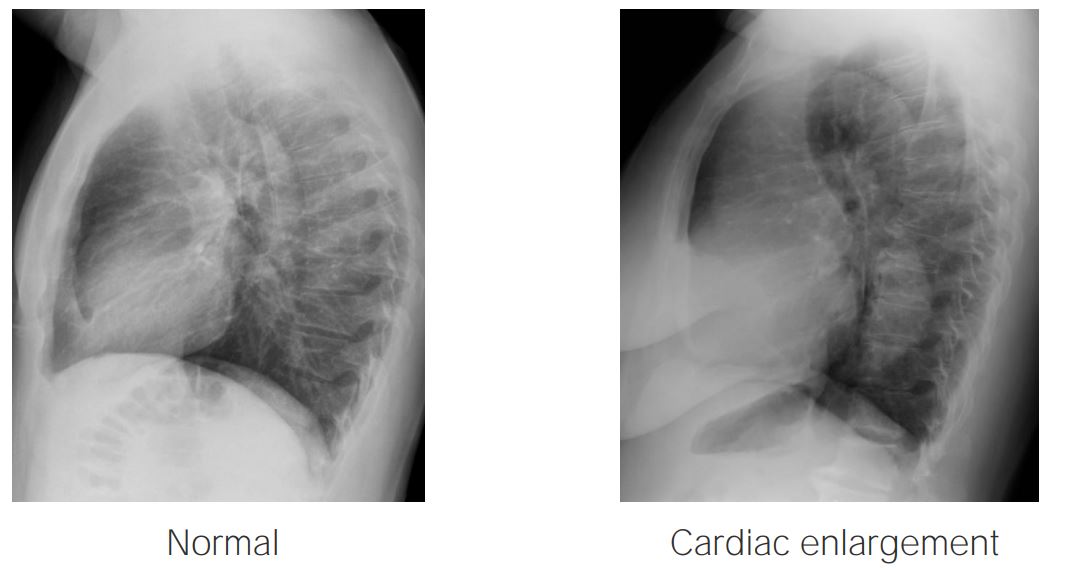
Lateral X-ray projections showing a normal heart (left) and an enlarged heart (right):
On the left, note how the anterior and posterior spaces of the heart are preserved, while on the right the posterior aspect of the heart is almost in contact with the thoracic spine.
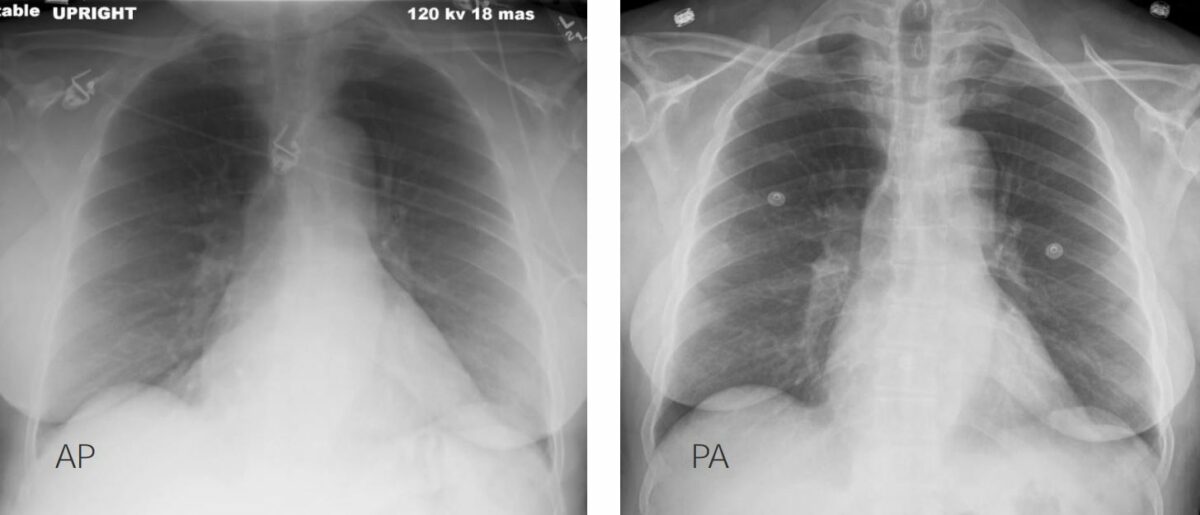
Differences between anteroposterior (AP) (left) and posteroanterior (PA) (right) X-ray projections:
In the AP view, the structures that are farther away from the cassette, such as the heart, are magnified.
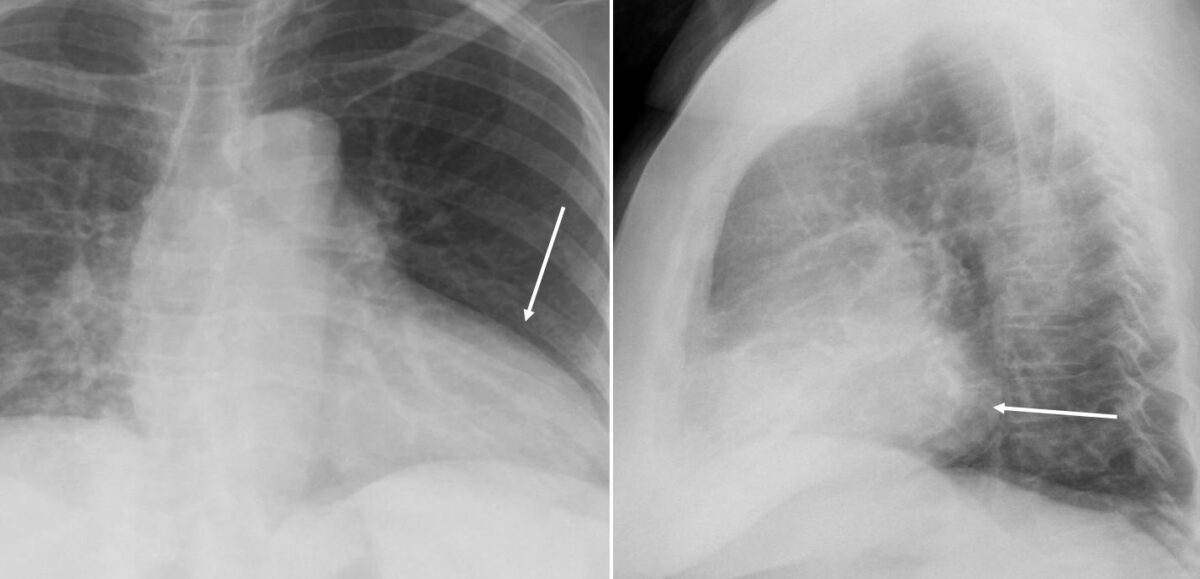
Posteroanterior (PA) (left) and lateral (right) X-ray projections of the chest showing left ventricular enlargement:
On the PA projection, note the enlargement of the left cardiac margin (arrow). On the lateral projection, note the posterior cardiac margin occupying the posterior cardiac space (arrow).

Chest X-ray showing right atrial enlargement:
Note the enlargement of the right cardiac margin.
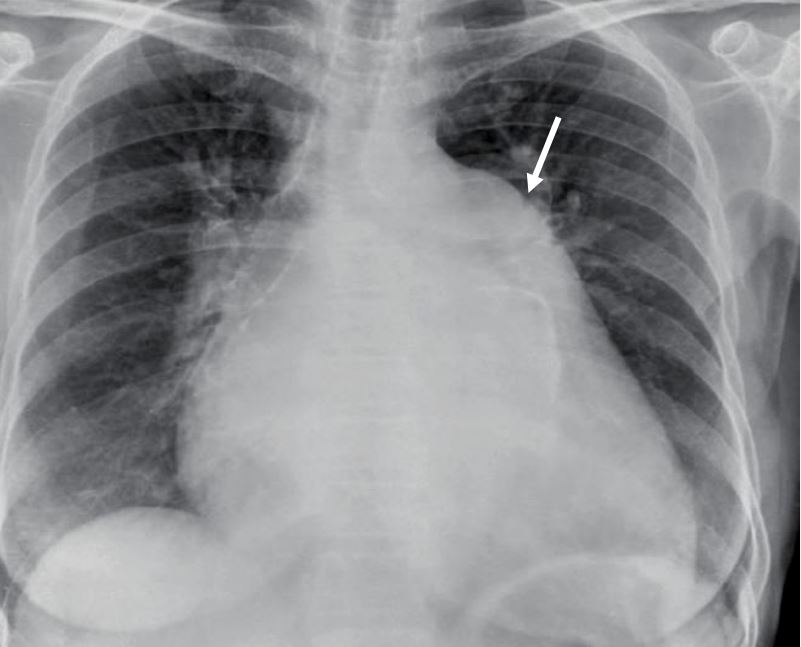
Chest X-ray showing left atrial enlargement:
Note the enlargement of the upper portion of the left cardiac margin.

Process of obtaining transthoracic echocardiographic imaging: transducer is placed on the chest to obtain views of the heart.
Image: “Heart lpla echocardiography diagram” by Patrick J. Lynch, medical illustrator; C. Carl Jaffe, MD, cardiologist. License: CC BY 2.5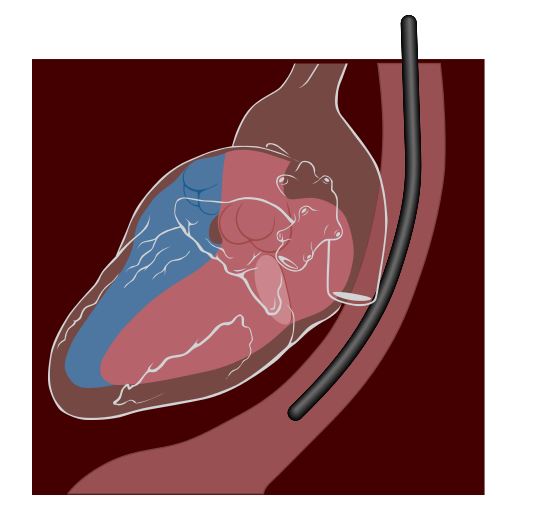
Transesophageal echocardiogram:
An endoscope is used to guide the transducer into the esophagus. In most adults, the probe is advanced to the proximal esophagus or midesophagus (or a depth of 28 to 30 cm from the incisors).
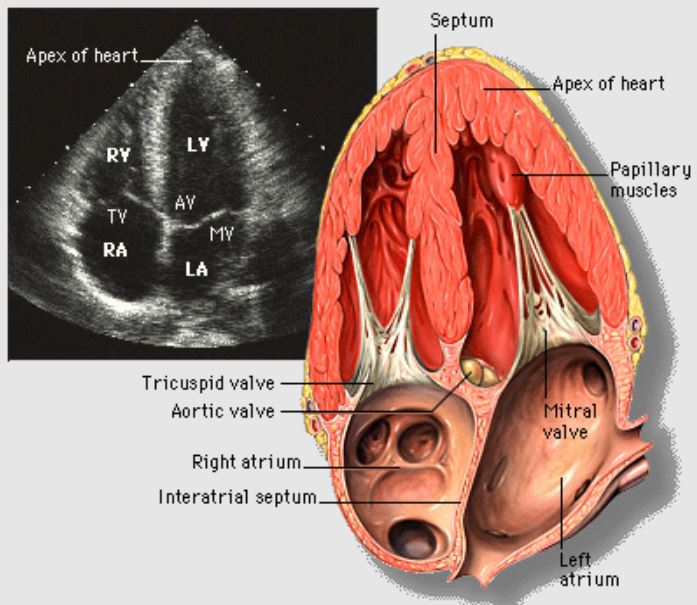
Echocardiogram:
Apical 4-chamber view of the heart
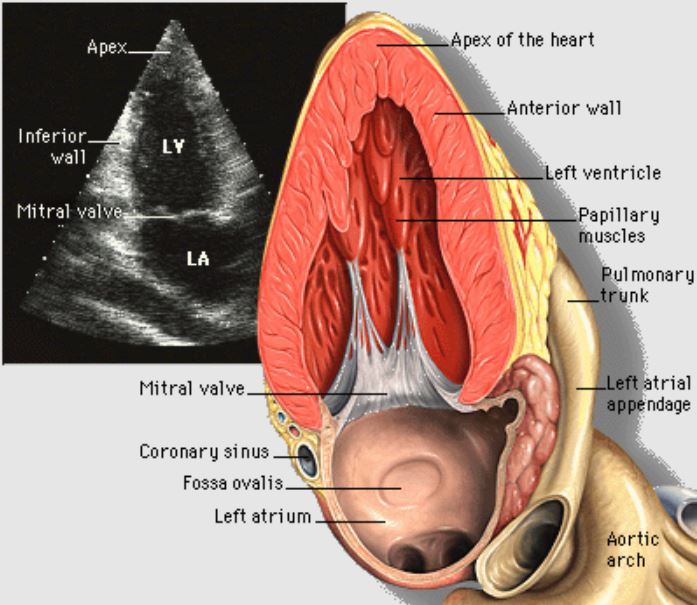
Echocardiogram:
Apical 2-chamber view of the heart
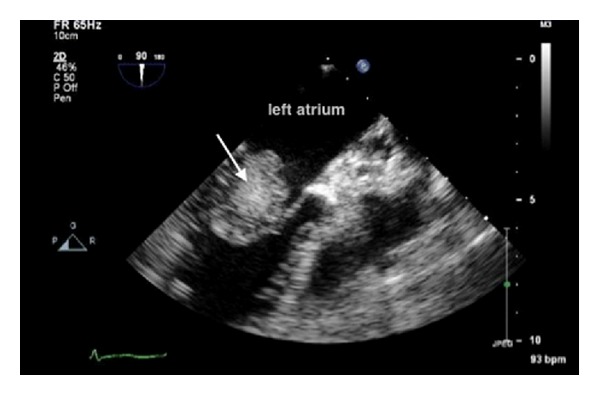
Echocardiogram showing a left atrial myxoma
Image: “ Echocardiogram showing left atrial myxoma (arrow)” by Al-Said Y, Al-Rached H, Baeesa S, Kurdi K, Zabani I, Hassan A. License: CC BY 3.0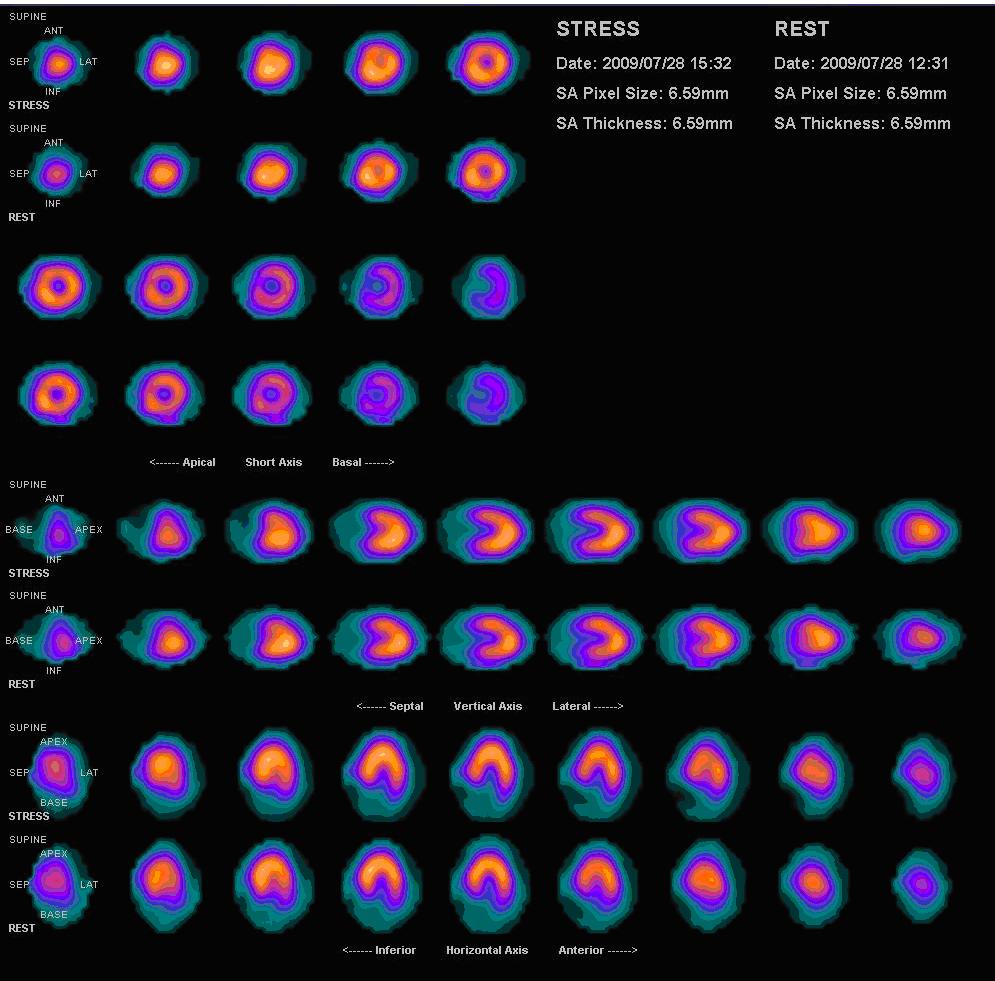
Normal myocardial perfusion scan with thallium-201 for the rest images (bottom rows) and technetium-sestamibi for the stress images (top rows)
Image: “Nl mpi2” by Myohan. License: CC BY 3.0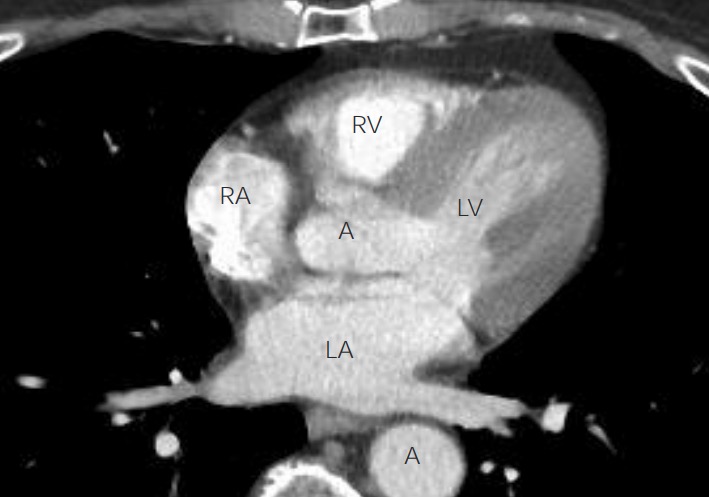
Anatomy of the heart on chest CT axial view:
A 4-chamber view of the heart can be obtained with chest CT. The left atrium (LA) can be recognized with 2 pulmonary veins returning blood to it. The left ventricle (LV), with its thicker walls, is seen in continuity with the left atrium. The right atrium (RA) and right ventricle (RV) are more difficult to see in this image. The ascending and descending aorta (A) are also visible.
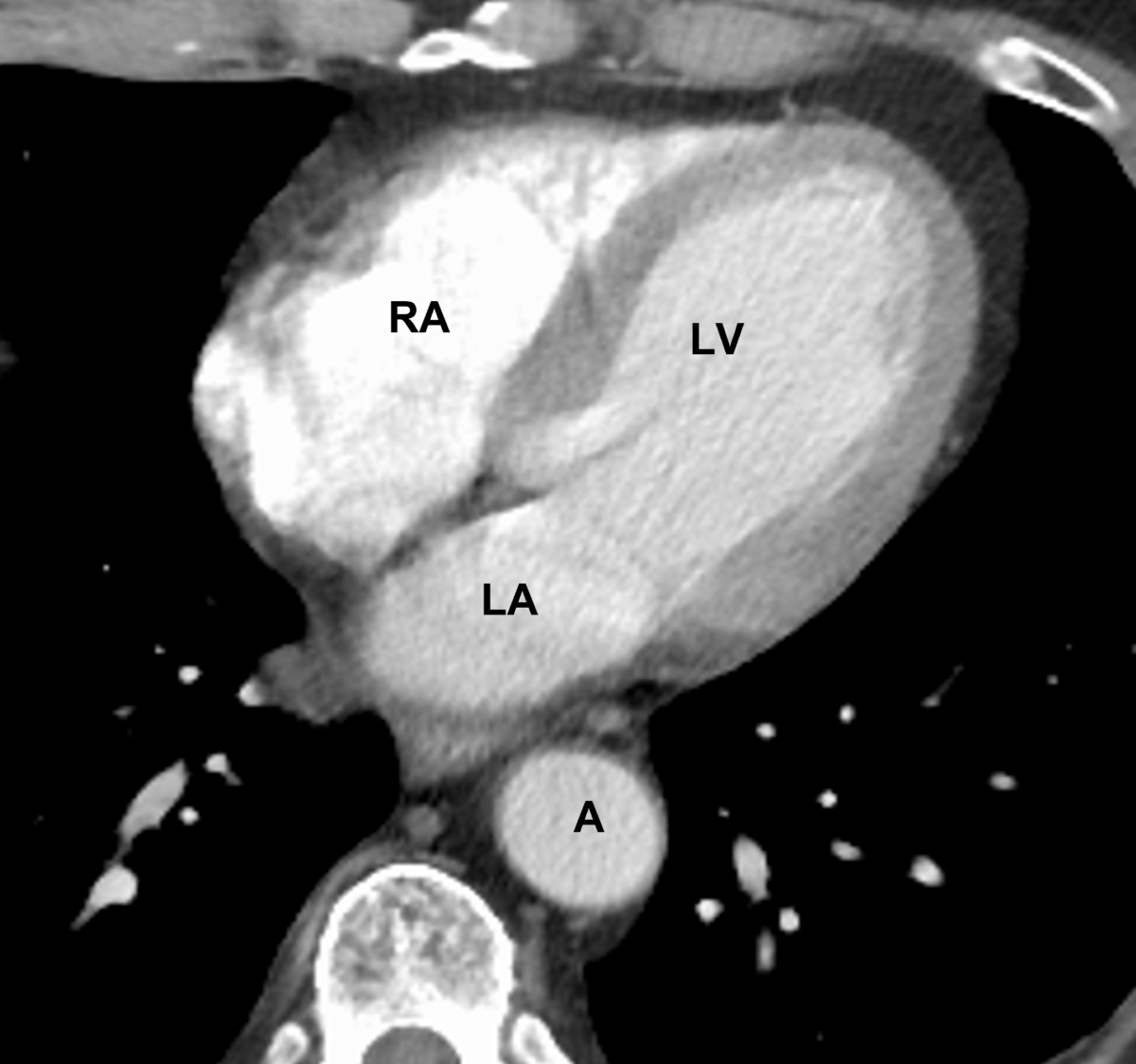
An axial cut of a chest CT scan visualizing the heart chambers:
Note the thickness of the left ventricular wall. Also, notice the descending aorta behind the left atrium (LA).
LV: left ventricle
RA: right atrium
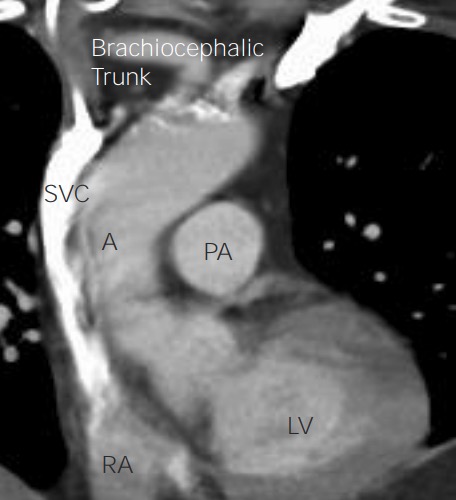
Anatomy of the heart on chest CT on coronal view:
Coronal view of the heart on chest CT provides more readily recognizable anatomic landmarks, with the aorta (A) arising from the left ventricle (LV) and the superior vena cava (SVC) feeding into the right atrium (RA). The left pulmonary artery (PA) can be seen head on, but its source (the right ventricle) is hidden in this image.
Aortic CTA CTA A non-invasive method that uses a ct scanner for capturing images of blood vessels and tissues. A contrast material is injected, which helps produce detailed images that aid in diagnosing vascular diseases. Pulmonary Function Tests:
CT pulmonary angiography Angiography Radiography of blood vessels after injection of a contrast medium. Cardiac Surgery ( CTPA CTPA Pulmonary Function Tests):

An axial cut of a chest CT scan visualizing the great vessels
A: aorta
PA: pulmonary artery
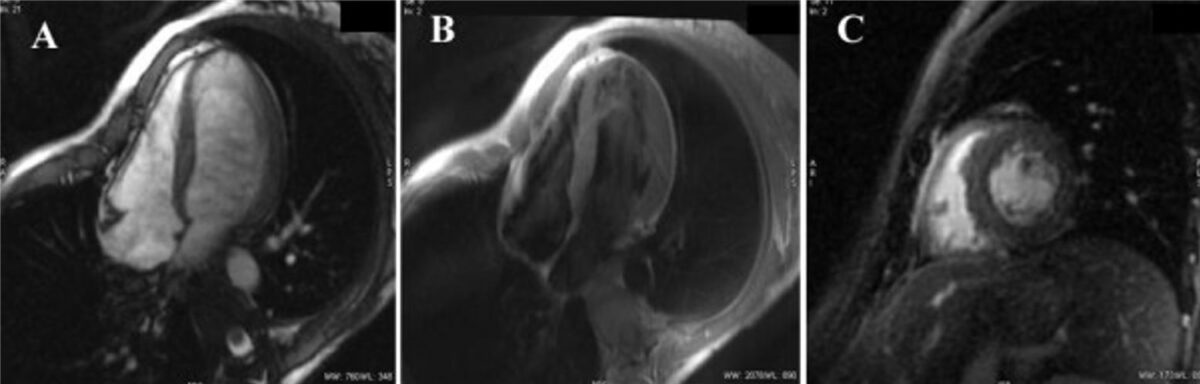
Cardiac MRI images:
A: Cardiac MRI gradient echo sequence of the normal dimensions and function of the left ventricle
B: T2-weighted short τ inversion recovery sequence
C: Late gadolinium hyperenhancement sequence
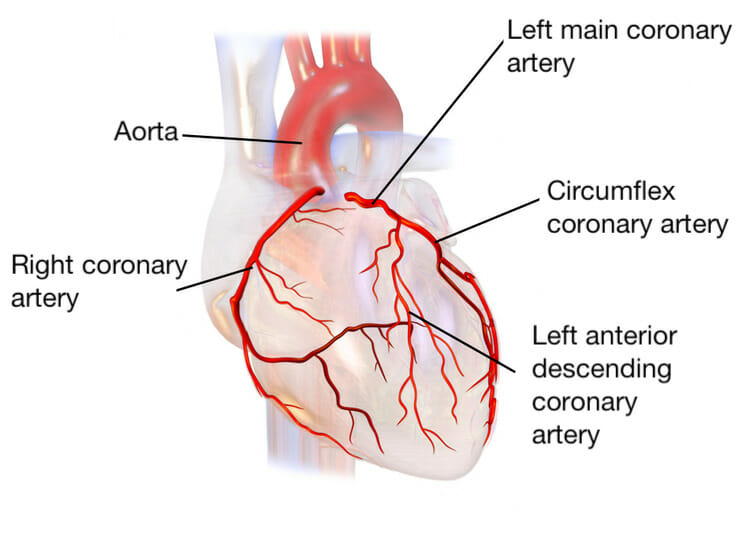
Main coronary arteries:
The left main coronary artery provides blood supply to the left side of the heart. The two branches are the left anterior descending artery and circumflex artery. The right coronary artery supplies the right side of the heart.
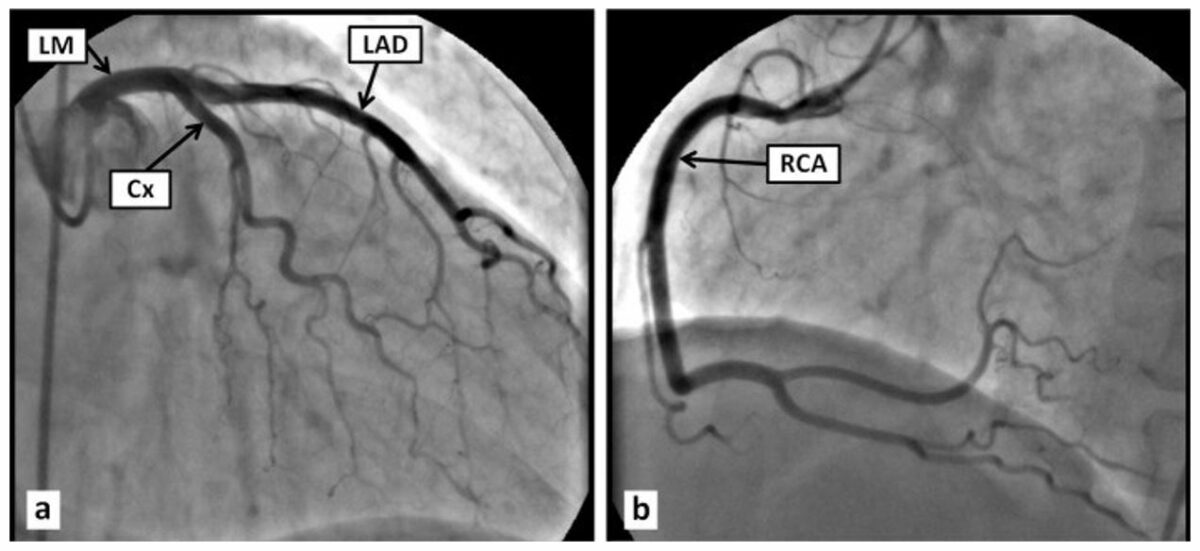
Normal coronary angiogram:
a: Normal left main coronary artery (LM), left anterior descending artery (LAD), circumflex artery (Cx)
b: Normal right main coronary artery (RCA)
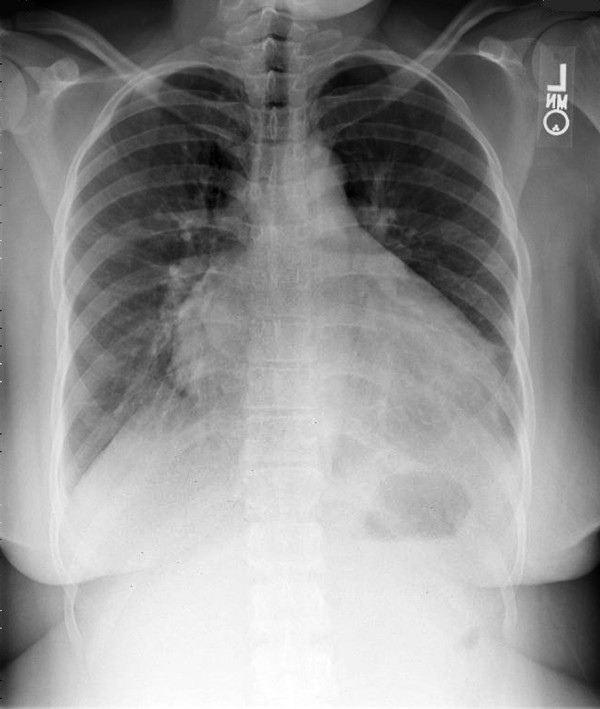
Chest X-ray showing prominent cardiomegaly and bibasilar interstitial markings in a patient with cardiomyopathy
Image: “Chest x-ray showing moderate cardiomegaly and prominent bibasilar interstitial markings” by Ibebuogu UN, Thornton JW, Reed GL. License: CC BY 2.0
Echocardiogram showing left ventricular dilatation during acute heart failure
Image: “Echocardiograph showing dilatation of the left ventricle in the acute phase” by Gangadhar TC, Von der Lohe E, Sawada SG, Helft PR. License: CC BY 2.0
Transthoracic echocardiogram:
A: Parasternal long-axis view showing asymmetric septal hypertrophic cardiomyopathy in end diastole
B: 4-chamber view showing a combination of basal and midventricular hypertrophic cardiomyopathy and an apical aneurysm (*)
Ao: aorta
LA = left atrium
RA = right atrium
RV = right ventricle
Image: “Transthoracic echocardiogram” by Cianciulli TF, Saccheri MC, Konopka IV, Serans DF, Acunzo RS, Escudero AM, Masoli OH, Prezioso HA. License: CC BY 2.0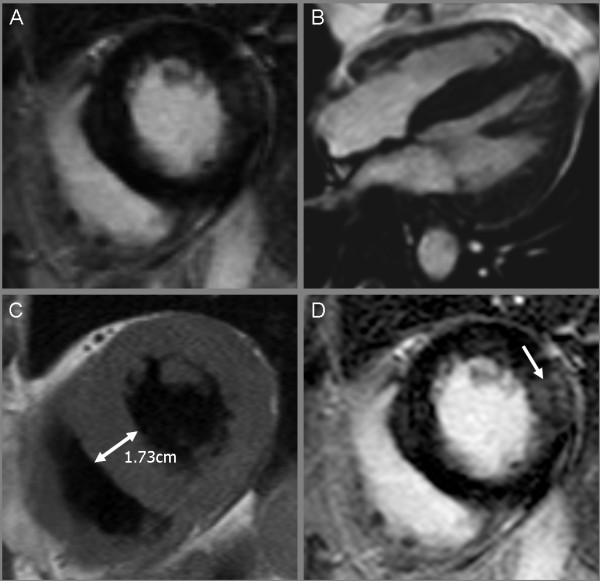
Cardiac MRI showing a marked hypertrophic cardiomyopathy:
Balanced fast-field echocardiogram (bFFE) cine sequence, short-axis view (A); 4-chamber view (B); a left ventricular hypertrophy with normal contractility was recognized.
T1-weighted black blood turbo spin echo sequence, short-axis view (C); left ventricular hypertrophy is evident, specifically in the septal region. Corresponding view with transmural late gadolinium enhancement (arrow) in the lateral wall using a T1-weighted inversion recovery 3D fast gradient echo sequence (D).

Pulmonary embolism:
Chest CT showing multiple filling defects of the principal branches (arrows) due to pulmonary embolism
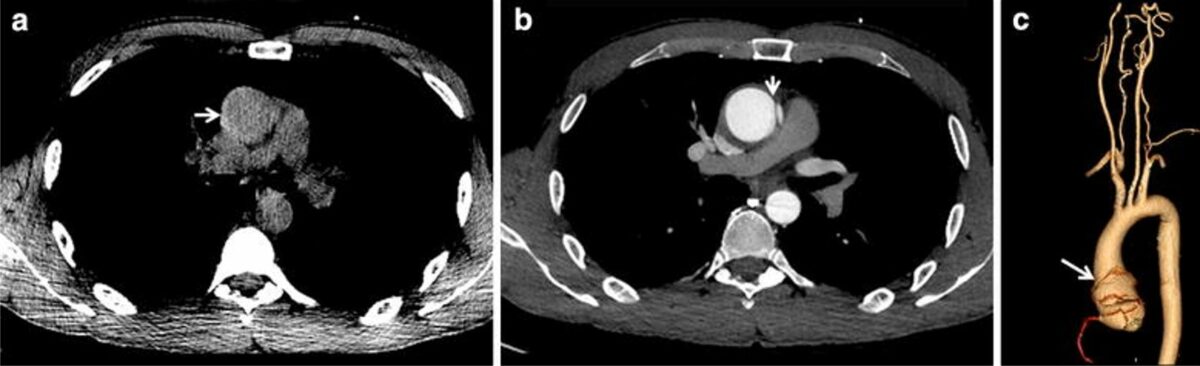
CT scan of aortic dissection:
a: Plain axial slices demonstrating a hyperintense crescent on the right margin of the aortic lumen indicating intramural hematoma (arrow)
b: Contrast-enhanced axial slices demonstrating the intimal flap (arrow) that underlies the pathognomonic double-lumen sign
c: Volume-rendered reconstructed image showing the margins of the Stanford type A aortic dissection (arrow)
The right coronary artery and the major thoracic and cervical arteries are not involved.
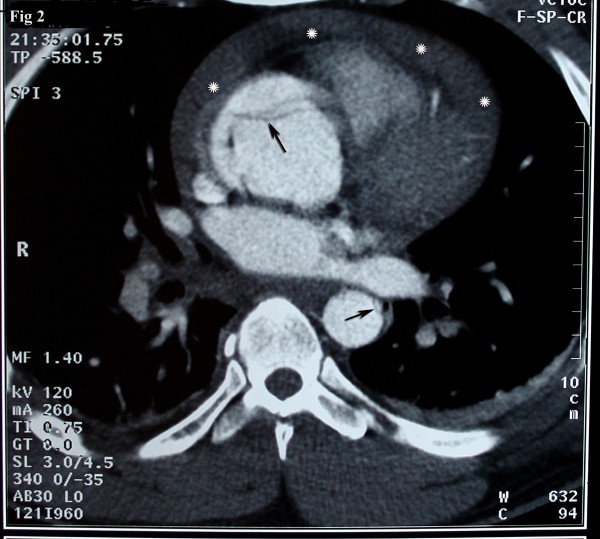
Axial source image of CTA reveals the flap in the ascending aorta compatible with type A Stanford dissection:
Arrows: flap in ascending aorta
Asterisks: hemopericardium.
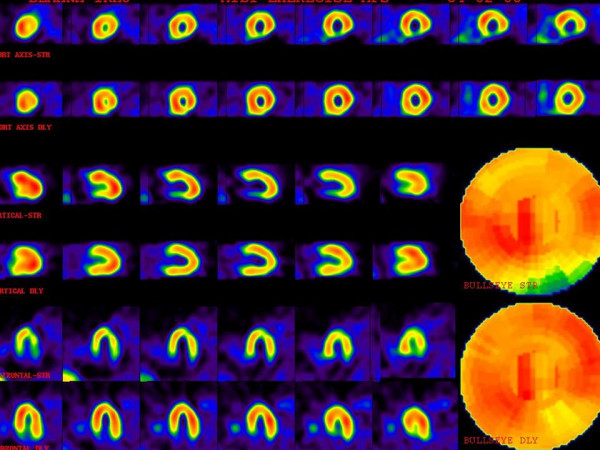
Multiple perfusion defects with different degrees of severity.
The upper images are stress phase and lower images are rest or delayed images. There is moderate ischemia in the midanterolateral and midinferolateral walls.
There also is severe ischemia in the basal inferior wall. Mild ischemia in the apex, apical septal, and basal anterolateral regions are also noted.

Calcified plaques in the anterior descending artery, in addition to others (not shown) in the other coronary arteries
CAC score = 285 (Agatston method), consistent with moderate coronary calcification, indicating moderate cardiovascular risk
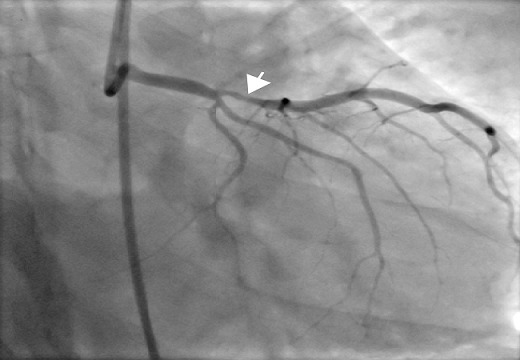
Coronary angiogram:
Stenosis of the left anterior descending artery (arrow)
Image: “Coronary angiogram with a stenosis of the LAD (arrow)” by Adeoye AM, Adekunle AN, Adebiyi AA, Mullassari A, Vijayakumar S, Nwafor CE. License: CC BY 2.0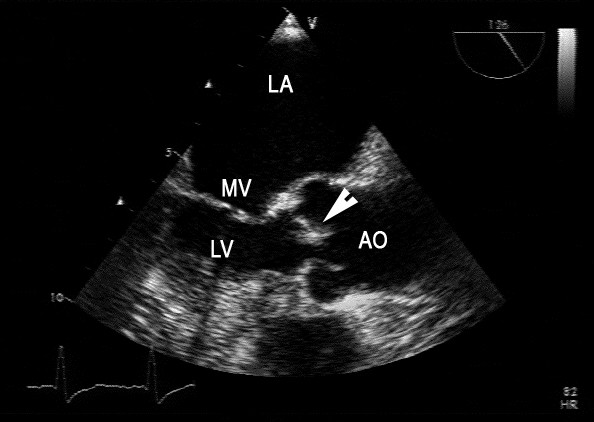
Endocarditis:
A transesophageal echocardiogram shows the left atrium (LA), parts of the mitral valve (MV), the left ventricle (LV), the ascending aorta (AO), and a thickened aortic cusp (arrow), the last of which is highly suggestive of endocarditis.

Chest X-ray showing pericardial effusion:
Note global enlargement of both cardiac margins (water bottle heart).
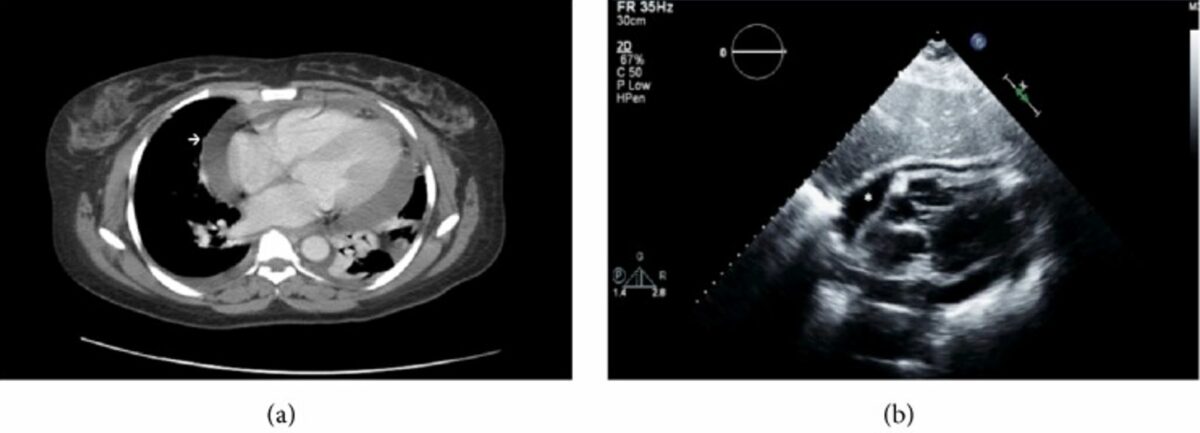
CT shows cardiomegaly with large pericardial effusion:
a: Bilateral pleural effusions with left lower lobe nearly completely collapsed
b: Parasternal long-axis echocardiogram showing pericardial effusion of moderate size with diastolic compression of the right atrium (asterisk)
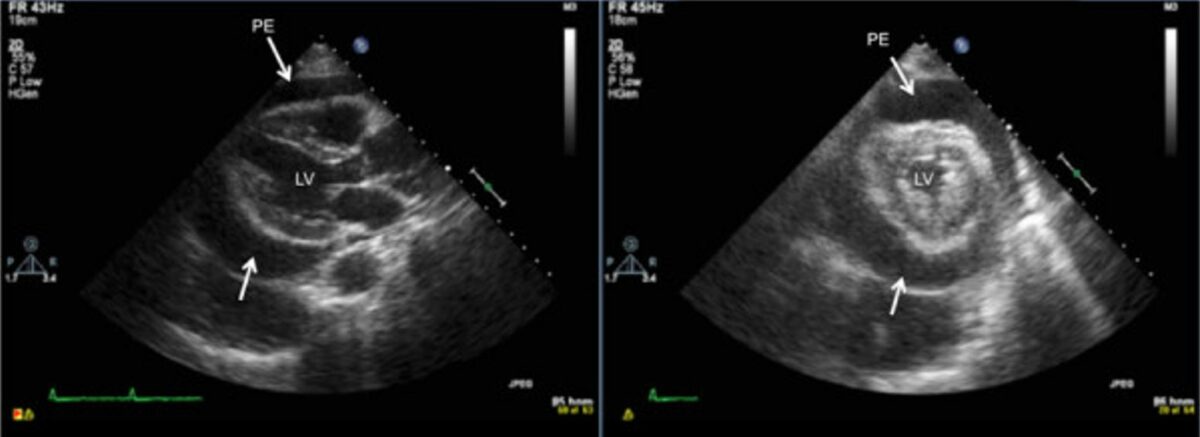
Transthoracic 2-dimensional echocardiogram:
Note the circumferential pericardial effusion on the long- and short-axis parasternal views on this transthoracic echocardiogram, prior to pericardiocentesis.
LV: left ventricle
PE: pericardial effusion