Idiopathic Idiopathic Dermatomyositis intracranial hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension (IIH), also known as pseudotumor cerebri, is a clinical disorder that presents with symptoms due to increased intracranial pressure Increased Intracranial Pressure Normal intracranial pressure (ICP) is defined as < 15 mm Hg, whereas pathologically increased ICP is any pressure ≥ 20 mm Hg. Increased ICP may result from several etiologies, including trauma, intracranial hemorrhage, mass lesions, cerebral edema, increased CSF production, and decreased CSF absorption. Increased Intracranial Pressure (ICP) ( ICP ICP Normal intracranial pressure (ICP) is defined as < 15 mm Hg, whereas pathologically increased ICP is any pressure ≥ 20 mm Hg. Increased ICP may result from several etiologies, including trauma, intracranial hemorrhage, mass lesions, cerebral edema, increased CSF production, and decreased CSF absorption. Increased Intracranial Pressure (ICP); ≥ 20 mm MM Multiple myeloma (MM) is a malignant condition of plasma cells (activated B lymphocytes) primarily seen in the elderly. Monoclonal proliferation of plasma cells results in cytokine-driven osteoclastic activity and excessive secretion of IgG antibodies. Multiple Myeloma Hg) or CSF pressure (> 250 mm MM Multiple myeloma (MM) is a malignant condition of plasma cells (activated B lymphocytes) primarily seen in the elderly. Monoclonal proliferation of plasma cells results in cytokine-driven osteoclastic activity and excessive secretion of IgG antibodies. Multiple Myeloma H2O), with no structural changes or other attributable causes. The condition is most commonly observed in obese women and after intake of certain drugs, such as growth hormones Hormones Hormones are messenger molecules that are synthesized in one part of the body and move through the bloodstream to exert specific regulatory effects on another part of the body. Hormones play critical roles in coordinating cellular activities throughout the body in response to the constant changes in both the internal and external environments. Hormones: Overview and Types, tetracycline Tetracycline A naphthacene antibiotic that inhibits amino Acyl tRNA binding during protein synthesis. Drug-Induced Liver Injury antibiotics, and high dosages of vitamin A Vitamin A Retinol and derivatives of retinol that play an essential role in metabolic functioning of the retina, the growth of and differentiation of epithelial tissue, the growth of bone, reproduction, and the immune response. Dietary vitamin A is derived from a variety of carotenoids found in plants. It is enriched in the liver, egg yolks, and the fat component of dairy products. Fat-soluble Vitamins and their Deficiencies. Classic manifestations include headache Headache The symptom of pain in the cranial region. It may be an isolated benign occurrence or manifestation of a wide variety of headache disorders. Brain Abscess, vision Vision Ophthalmic Exam loss or visual-field defects, and papilledema. Diagnosis is made by clinical exam, imaging, and lumbar puncture Lumbar Puncture Febrile Infant. Management is aimed at decreasing ICP ICP Normal intracranial pressure (ICP) is defined as < 15 mm Hg, whereas pathologically increased ICP is any pressure ≥ 20 mm Hg. Increased ICP may result from several etiologies, including trauma, intracranial hemorrhage, mass lesions, cerebral edema, increased CSF production, and decreased CSF absorption. Increased Intracranial Pressure (ICP) and includes medication, therapeutic CSF removal, and shunting.
Last updated: Dec 15, 2025
Idiopathic Idiopathic Dermatomyositis intracranial hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension (IIH), also known as pseudotumor cerebri, is a clinical disorder that presents with symptoms due to increased intracranial pressure Increased Intracranial Pressure Normal intracranial pressure (ICP) is defined as < 15 mm Hg, whereas pathologically increased ICP is any pressure ≥ 20 mm Hg. Increased ICP may result from several etiologies, including trauma, intracranial hemorrhage, mass lesions, cerebral edema, increased CSF production, and decreased CSF absorption. Increased Intracranial Pressure (ICP) ( ICP ICP Normal intracranial pressure (ICP) is defined as < 15 mm Hg, whereas pathologically increased ICP is any pressure ≥ 20 mm Hg. Increased ICP may result from several etiologies, including trauma, intracranial hemorrhage, mass lesions, cerebral edema, increased CSF production, and decreased CSF absorption. Increased Intracranial Pressure (ICP); ≥ 20 mm MM Multiple myeloma (MM) is a malignant condition of plasma cells (activated B lymphocytes) primarily seen in the elderly. Monoclonal proliferation of plasma cells results in cytokine-driven osteoclastic activity and excessive secretion of IgG antibodies. Multiple Myeloma Hg) or CSF pressure (> 250 mm MM Multiple myeloma (MM) is a malignant condition of plasma cells (activated B lymphocytes) primarily seen in the elderly. Monoclonal proliferation of plasma cells results in cytokine-driven osteoclastic activity and excessive secretion of IgG antibodies. Multiple Myeloma H2O), with no structural changes or other attributable cause.
The exact pathogenesis of IIH is unknown, although there are several proposed mechanisms. Cerebral edema Cerebral edema Increased intracellular or extracellular fluid in brain tissue. Cytotoxic brain edema (swelling due to increased intracellular fluid) is indicative of a disturbance in cell metabolism, and is commonly associated with hypoxic or ischemic injuries. An increase in extracellular fluid may be caused by increased brain capillary permeability (vasogenic edema), an osmotic gradient, local blockages in interstitial fluid pathways, or by obstruction of CSF flow (e.g., obstructive hydrocephalus). Increased Intracranial Pressure (ICP) has not been found in IIH, as hypothesized in the past.
Idiopathic Idiopathic Dermatomyositis intracranial hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension should be considered in the differential diagnosis for any individual who presents with headaches and papilledema.

Photo demonstrating papilledema (swollen optic disc with blurred disk margins)
Image: “Papilledema” by Jonathan Trobe, M.D. License: CC BY 3.0The diagnosis of IIH is clinical; urgent neuroimaging Neuroimaging Non-invasive methods of visualizing the central nervous system, especially the brain, by various imaging modalities. Febrile Infant is required to rule out other causes of increased ICP Increased ICP Excessive accumulation of cerebrospinal fluid within the cranium which may be associated with dilation of cerebral ventricles, intracranial. Subarachnoid Hemorrhage.
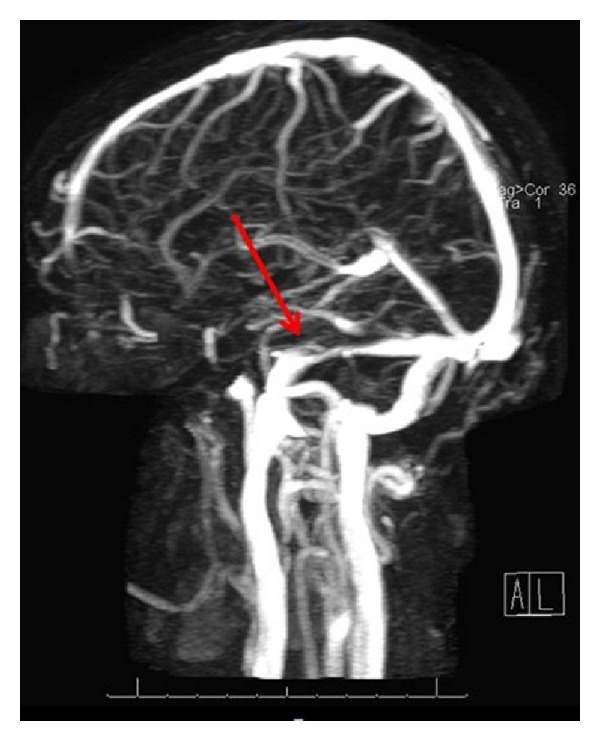
Narrowing of the transverse sinuses:
MRV (magnetic resonance venography) showing narrowing of the transverse venous sinuses, most likely related to idiopathic intracranial hypertension.
Increased ICP Increased ICP Excessive accumulation of cerebrospinal fluid within the cranium which may be associated with dilation of cerebral ventricles, intracranial. Subarachnoid Hemorrhage is a medical emergency. Definitive management depends on the underlying etiology.