Hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension, or high blood pressure, is a common medical condition manifesting as elevated systemic arterial pressure. Hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension is most often asymptomatic and discovered as part of a routine physical examination, or during triage for an unrelated medical encounter. Age, gender Gender Gender Dysphoria, smoking Smoking Willful or deliberate act of inhaling and exhaling smoke from burning substances or agents held by hand. Interstitial Lung Diseases, obesity Obesity Obesity is a condition associated with excess body weight, specifically with the deposition of excessive adipose tissue. Obesity is considered a global epidemic. Major influences come from the western diet and sedentary lifestyles, but the exact mechanisms likely include a mixture of genetic and environmental factors. Obesity, and diet are all contributing factors to hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension and can lead to heart attack Heart attack Mi is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction, stroke, heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR), and CKD CKD Chronic kidney disease (CKD) is kidney impairment that lasts for ≥ 3 months, implying that it is irreversible. Hypertension and diabetes are the most common causes; however, there are a multitude of other etiologies. In the early to moderate stages, CKD is usually asymptomatic and is primarily diagnosed by laboratory abnormalities. Chronic Kidney Disease if not managed properly. If blood pressure cannot be controlled with lifestyle modifications, medications are employed for the management of hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension. The 1st-line medication classes include thiazide-like diuretics Diuretics Agents that promote the excretion of urine through their effects on kidney function. Heart Failure and Chronic Coronary Syndrome Medication, angiotensin-converting enzyme inhibitors Angiotensin-converting enzyme inhibitors A class of drugs whose main indications are the treatment of hypertension and heart failure. They exert their hemodynamic effect mainly by inhibiting the renin-angiotensin system. They also modulate sympathetic nervous system activity and increase prostaglandin synthesis. They cause mainly vasodilation and mild natriuresis without affecting heart rate and contractility. Renin-Angiotensin-Aldosterone System Inhibitors ( ACEis ACEIs A class of drugs whose main indications are the treatment of hypertension and heart failure. They exert their hemodynamic effect mainly by inhibiting the renin-angiotensin system. They also modulate sympathetic nervous system activity and increase prostaglandin synthesis. They cause mainly vasodilation and mild natriuresis without affecting heart rate and contractility. Heart Failure and Chronic Coronary Syndrome Medication), angiotensin II Angiotensin II An octapeptide that is a potent but labile vasoconstrictor. It is produced from angiotensin I after the removal of two amino acids at the c-terminal by angiotensin converting enzyme. The amino acid in position 5 varies in different species. To block vasoconstriction and hypertension effect of angiotensin II, patients are often treated with ace inhibitors or with angiotensin II type 1 receptor blockers. Renal Sodium and Water Regulation receptor Receptor Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors blockers ( ARBs ARBs Agents that antagonize angiotensin receptors. Many drugs in this class specifically target the angiotensin type 1 receptor. Heart Failure and Chronic Coronary Syndrome Medication), and calcium Calcium A basic element found in nearly all tissues. It is a member of the alkaline earth family of metals with the atomic symbol ca, atomic number 20, and atomic weight 40. Calcium is the most abundant mineral in the body and combines with phosphorus to form calcium phosphate in the bones and teeth. It is essential for the normal functioning of nerves and muscles and plays a role in blood coagulation (as factor IV) and in many enzymatic processes. Electrolytes channel blockers ( CCBs CCBs Calcium channel blockers (CCBS) are a class of medications that inhibit voltage-dependent L-type calcium channels of cardiac and vascular smooth muscle cells. The inhibition of these channels produces vasodilation and myocardial depression. There are 2 major classes of CCBS: dihydropyridines and non-dihydropyridines. Class 4 Antiarrhythmic Drugs (Calcium Channel Blockers)). Contraindications Contraindications A condition or factor associated with a recipient that makes the use of a drug, procedure, or physical agent improper or inadvisable. Contraindications may be absolute (life threatening) or relative (higher risk of complications in which benefits may outweigh risks). Noninvasive Ventilation, adverse effects, and drug-to-drug interactions are agent specific.
Last updated: Dec 15, 2025
American Heart Association American Heart Association A voluntary organization concerned with the prevention and treatment of heart and vascular diseases. Heart Failure and American College of Cardiology guidelines (2017, 2021):
Eighth Joint National Committee (JNC 8, 2014) guidelines:
Selection Selection Lymphocyte activation by a specific antigen thus triggering clonal expansion of lymphocytes already capable of mounting an immune response to the antigen. B cells: Types and Functions of antihypertensive agent should be based on:
| BP category | Systolic BP (mm Hg) | Diastolic BP (mm Hg) | |
|---|---|---|---|
| Normal BP | < 120 mm Hg | AND | < 80 mm Hg |
| Elevated BP | 120–129 mm Hg | AND | < 80 mm Hg |
| Stage 1 Stage 1 Trypanosoma brucei/African trypanosomiasis hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension | 130–139 mm Hg | OR | 80–89 mm Hg |
| Stage 2 hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension | ≥ 140 mm Hg | OR | ≥ 90 mm Hg |
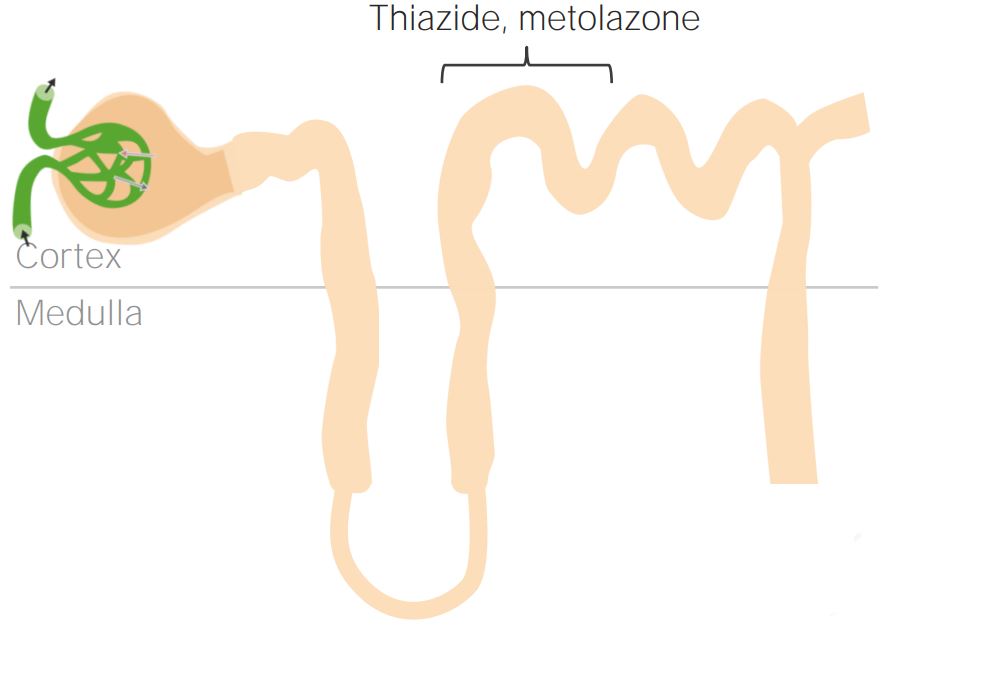
Thiazide and thiazide-like diuretics and where they act on the renal tubule
Image by Lecturio.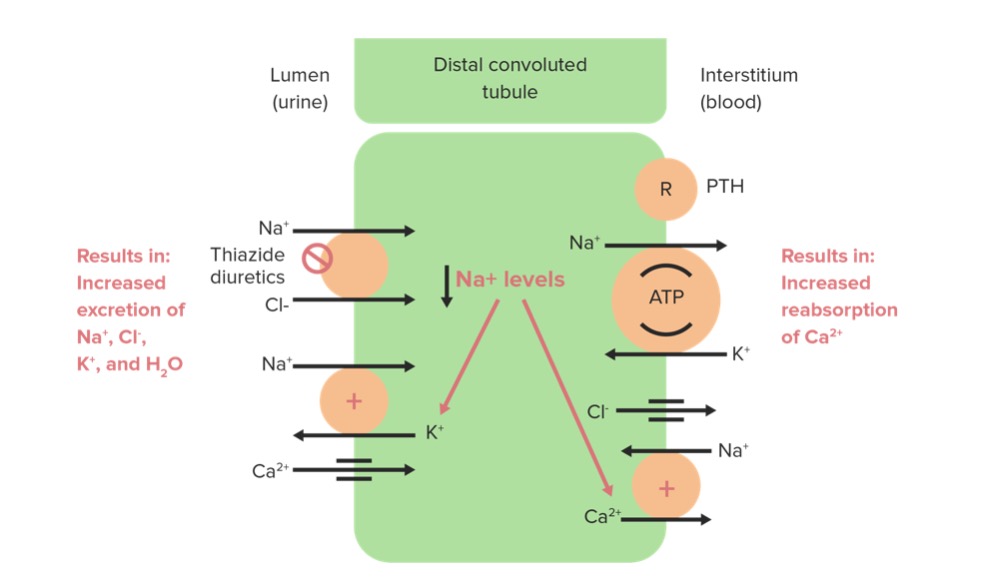
Thiazide diuretics acting on the Na/Cl cotransporter
Image by Lecturio. License: CC BY-NC-SA 4.0| Drug | Absorption Absorption Absorption involves the uptake of nutrient molecules and their transfer from the lumen of the GI tract across the enterocytes and into the interstitial space, where they can be taken up in the venous or lymphatic circulation. Digestion and Absorption | Metabolism | Excretion |
|---|---|---|---|
| HCTZ HCTZ A thiazide diuretic often considered the prototypical member of this class. It reduces the reabsorption of electrolytes from the renal tubules. This results in increased excretion of water and electrolytes, including sodium, potassium, chloride, and magnesium. It is used in the treatment of several disorders including edema, hypertension, diabetes insipidus, and hypoparathyroidism. Thiazide Diuretics |
|
Not metabolized |
|
| Chlorothiazide |
|
Not metabolized |
|
| Chlorthalidone Chlorthalidone A benzenesulfonamide-phthalimidine that tautomerizes to a benzophenones form. It is considered a thiazide-like diuretic. Thiazide Diuretics | Peak effect 2–6 hours | Hepatic |
|
| Indapamide |
|
Extensive hepatic metabolism |
|
| Metolazone | Onset of action: 1 hour | Not metabolized | Urine |
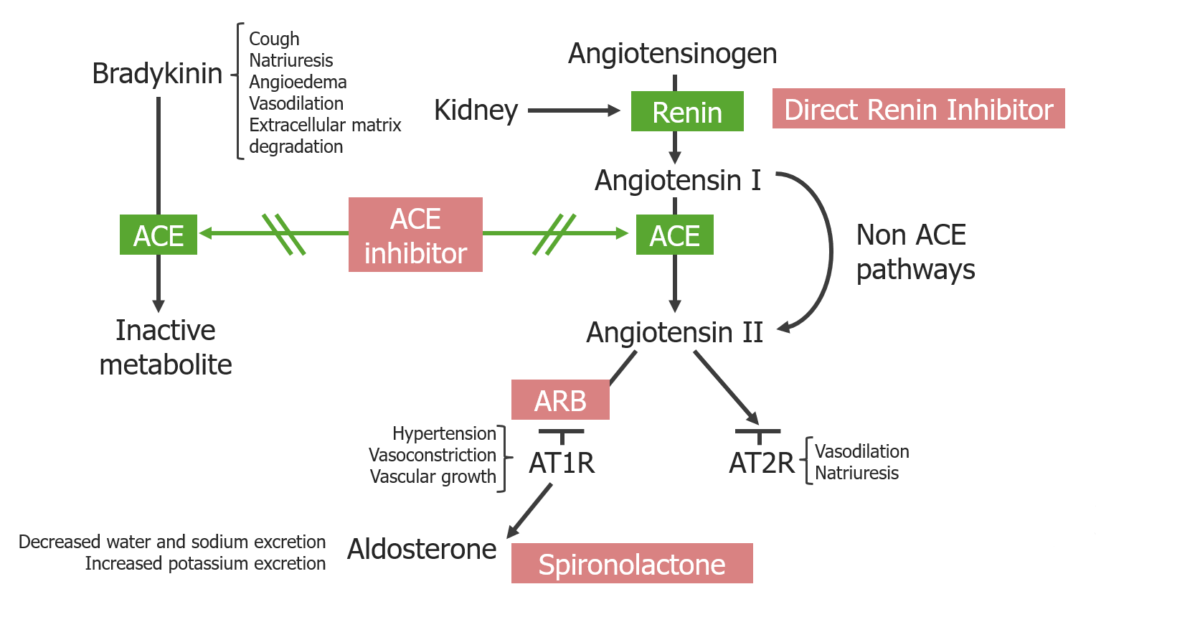
Overview of RAAS inhibitors and their location of action:
ACE inhibitors block both the degradation of bradykinin and the generation of angiotensin II.
ARBs block the angiotensin II type 1 receptors. Direct renin inhibitors block the generation of angiotensin I.
Spironolactone blocks mineralocorticoid receptors at the principal cells in the distal renal tubules and cortical collecting duct.
| Drug | Absorption Absorption Absorption involves the uptake of nutrient molecules and their transfer from the lumen of the GI tract across the enterocytes and into the interstitial space, where they can be taken up in the venous or lymphatic circulation. Digestion and Absorption | Metabolism | Excretion |
|---|---|---|---|
| ACEis ACEIs A class of drugs whose main indications are the treatment of hypertension and heart failure. They exert their hemodynamic effect mainly by inhibiting the renin-angiotensin system. They also modulate sympathetic nervous system activity and increase prostaglandin synthesis. They cause mainly vasodilation and mild natriuresis without affecting heart rate and contractility. Heart Failure and Chronic Coronary Syndrome Medication |
|
Prodrugs are activated via hydrolysis Hydrolysis The process of cleaving a chemical compound by the addition of a molecule of water. Proteins and Peptides in the liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy; active drugs are unchanged. |
|
| ARBs ARBs Agents that antagonize angiotensin receptors. Many drugs in this class specifically target the angiotensin type 1 receptor. Heart Failure and Chronic Coronary Syndrome Medication |
|
Hepatic metabolism |
|
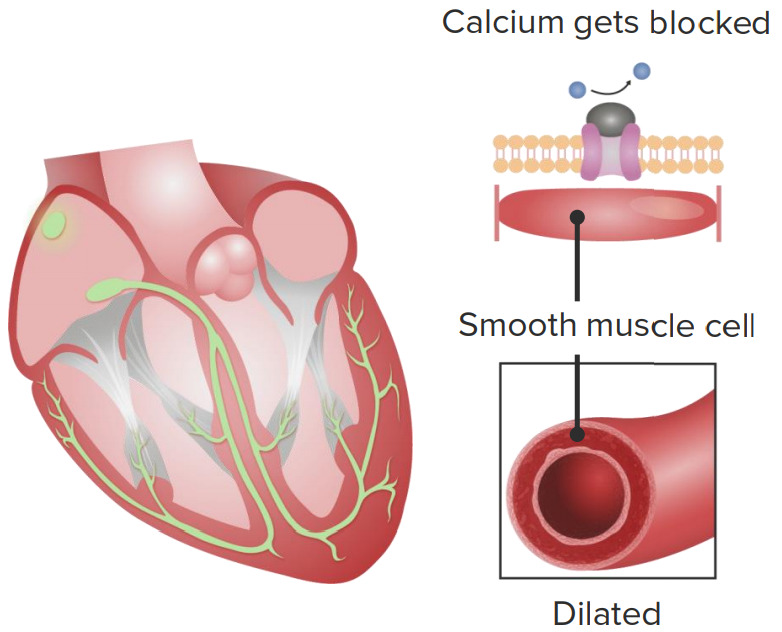
Cardiovascular effects of calcium channel blockers (CCBs)
1. CCBs slow down the sinoatrial node, causing lowered heart rate.
2. CCB intake leads to vascular smooth muscle relaxation, causing vasodilation.
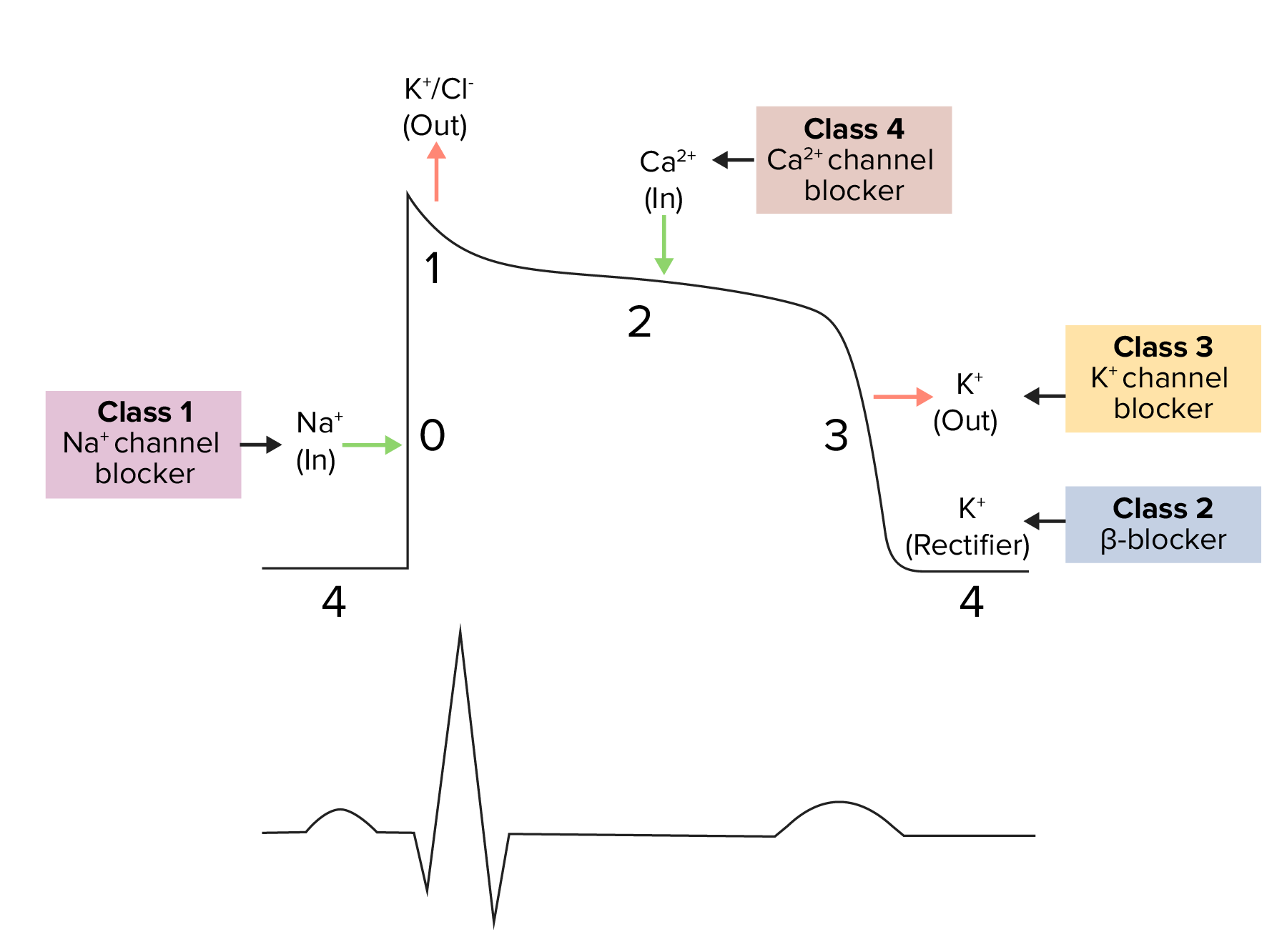
Diagram demonstrating a cardiac action potential and the phases of action for different antiarrhythmic drug classes:
The cycle starts with phase 4, the resting potential. Phase 0 is when rapid depolarization happens due to an influx of sodium ions into the cell. This is where class 1 (sodium channel blockers) antiarrhythmics work.
Repolarization follows, with an efflux of potassium through fast potassium channels in phase 1, calcium influx in phase 2, and efflux of potassium through delayed potassium channels in phase 3.
| Location of action | Class | Subclass |
|---|---|---|
| Renal drugs | Diuretics Diuretics Agents that promote the excretion of urine through their effects on kidney function. Heart Failure and Chronic Coronary Syndrome Medication |
|
| Drugs affecting RAAS RAAS A blood pressure regulating system of interacting components that include renin; angiotensinogen; angiotensin converting enzyme; angiotensin i; angiotensin ii; and angiotensinase. Renin, an enzyme produced in the kidney, acts on angiotensinogen, an alpha-2 globulin produced by the liver, forming angiotensin I. Angiotensin-converting enzyme, contained in the lung, acts on angiotensin I in the plasma converting it to angiotensin II, an extremely powerful vasoconstrictor. Angiotensin II causes contraction of the arteriolar and renal vascular smooth muscle, leading to retention of salt and water in the kidney and increased arterial blood pressure. In addition, angiotensin II stimulates the release of aldosterone from the adrenal cortex, which in turn also increases salt and water retention in the kidney. Angiotensin-converting enzyme also breaks down bradykinin, a powerful vasodilator and component of the kallikrein-kinin system. Adrenal Hormones |
|
|
| Extrarenal drugs | Direct vasodilators Vasodilators Drugs used to cause dilation of the blood vessels. Thromboangiitis Obliterans (Buerger Disease) |
|
| Agents acting via the sympathetic nervous system Nervous system The nervous system is a small and complex system that consists of an intricate network of neural cells (or neurons) and even more glial cells (for support and insulation). It is divided according to its anatomical components as well as its functional characteristics. The brain and spinal cord are referred to as the central nervous system, and the branches of nerves from these structures are referred to as the peripheral nervous system. Nervous System: Anatomy, Structure, and Classification |
|
| Drug class | Mechanism of action | Examples of drugs in the class | Adverse effects | Other |
|---|---|---|---|---|
| Thiazide-like diuretic |
|
|
|
Excellent as 1st-line monotherapy or in combination |
| ACEi ACEi A class of drugs whose main indications are the treatment of hypertension and heart failure. They exert their hemodynamic effect mainly by inhibiting the renin-angiotensin system. They also modulate sympathetic nervous system activity and increase prostaglandin synthesis. They cause mainly vasodilation and mild natriuresis without affecting heart rate and contractility. Renin-Angiotensin-Aldosterone System Inhibitors | Prevents conversion of angiotensin I to angiotensin II Angiotensin II An octapeptide that is a potent but labile vasoconstrictor. It is produced from angiotensin I after the removal of two amino acids at the c-terminal by angiotensin converting enzyme. The amino acid in position 5 varies in different species. To block vasoconstriction and hypertension effect of angiotensin II, patients are often treated with ace inhibitors or with angiotensin II type 1 receptor blockers. Renal Sodium and Water Regulation |
|
|
|
| ARB | Blocks binding of angiotensin II Angiotensin II An octapeptide that is a potent but labile vasoconstrictor. It is produced from angiotensin I after the removal of two amino acids at the c-terminal by angiotensin converting enzyme. The amino acid in position 5 varies in different species. To block vasoconstriction and hypertension effect of angiotensin II, patients are often treated with ace inhibitors or with angiotensin II type 1 receptor blockers. Renal Sodium and Water Regulation to the receptor Receptor Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors |
|
|
|
| CCB | Inhibits the voltage-gated Ca CA Condylomata acuminata are a clinical manifestation of genital HPV infection. Condylomata acuminata are described as raised, pearly, flesh-colored, papular, cauliflower-like lesions seen in the anogenital region that may cause itching, pain, or bleeding. Condylomata Acuminata (Genital Warts)2+ channel → smooth muscle relaxation |
|
|
1st-line therapy in individuals with abnormal renal function |
| Drug class | Mechanism of action | Examples of drugs in the class | Adverse effects | Other |
|---|---|---|---|---|
| Beta-blockers Beta-blockers Drugs that bind to but do not activate beta-adrenergic receptors thereby blocking the actions of beta-adrenergic agonists. Adrenergic beta-antagonists are used for treatment of hypertension, cardiac arrhythmias, angina pectoris, glaucoma, migraine headaches, and anxiety. Class 2 Antiarrhythmic Drugs (Beta Blockers) | ↓ Sympathetic output by blockade of B-adrenergic receptors Receptors Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors |
|
|
2nd-line therapy for chronic hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension (unless another indication for beta-blocker therapy is present) |
| Loop diuretics Diuretics Agents that promote the excretion of urine through their effects on kidney function. Heart Failure and Chronic Coronary Syndrome Medication | Blockade of the Na+/K+-2Cl cotransporter in the loop of Henle Loop of Henle The U-shaped portion of the renal tubule in the kidney medulla, consisting of a descending limb and an ascending limb. It is situated between the proximal kidney tubule and the distal kidney tubule. Tubular System |
|
|
Used in HF-related hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension |
| Aldosterone antagonists Aldosterone antagonists Drugs that bind to and block the activation of mineralocorticoid receptors by mineralocorticoids such as aldosterone. Heart Failure and Chronic Coronary Syndrome Medication |
|
|
|
May have superior benefit in refractory hypertension Refractory hypertension Blood pressure that cannot be controlled even with maximally tolerated doses of ≥ 5 drugs. Uncontrolled Hypertension |
| Alpha-1 blockers | Selective blockade of the alpha-1 adrenergic receptor Receptor Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors |
|
Orthostatic hypotension Orthostatic hypotension A significant drop in blood pressure after assuming a standing position. Orthostatic hypotension is a finding, and defined as a 20-mm hg decrease in systolic pressure or a 10-mm hg decrease in diastolic pressure 3 minutes after the person has risen from supine to standing. Symptoms generally include dizziness, blurred vision, and syncope. Hypotension | Used in benign Benign Fibroadenoma prostatic hypertrophy Hypertrophy General increase in bulk of a part or organ due to cell enlargement and accumulation of fluids and secretions, not due to tumor formation, nor to an increase in the number of cells (hyperplasia). Cellular Adaptation and hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension |
| Nonselective alpha blockers | Blockade of alpha-1 and alpha-2 receptors Receptors Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors |
|
Orthostatic hypotension Orthostatic hypotension A significant drop in blood pressure after assuming a standing position. Orthostatic hypotension is a finding, and defined as a 20-mm hg decrease in systolic pressure or a 10-mm hg decrease in diastolic pressure 3 minutes after the person has risen from supine to standing. Symptoms generally include dizziness, blurred vision, and syncope. Hypotension |
|
| Alpha-2 agonists | ↓ Overall sympathetic activity | Clonidine Clonidine An imidazoline sympatholytic agent that stimulates alpha-2 adrenergic receptors and central imidazoline receptors. It is commonly used in the management of hypertension. Sympathomimetic Drugs |
|
Useful in opioid-withdrawal hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension |
| Vasodilators Vasodilators Drugs used to cause dilation of the blood vessels. Thromboangiitis Obliterans (Buerger Disease) | Direct arteriolar vasodilation Vasodilation The physiological widening of blood vessels by relaxing the underlying vascular smooth muscle. Pulmonary Hypertension Drugs | Hydralazine Hydralazine A direct-acting vasodilator that is used as an antihypertensive agent. Heart Failure and Chronic Coronary Syndrome Medication |
|
Treats hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension in pregnancy Pregnancy The status during which female mammals carry their developing young (embryos or fetuses) in utero before birth, beginning from fertilization to birth. Pregnancy: Diagnosis, Physiology, and Care |
| Nitrates Nitrates Nitrates are a class of medications that cause systemic vasodilation (veins > arteries) by smooth muscle relaxation. Nitrates are primarily indicated for the treatment of angina, where preferential venodilation causes pooling of blood, decreased preload, and ultimately decreased myocardial O2 demand. Nitrates | ↑ cGMP cGMP Guanosine cyclic 3. Phosphodiesterase Inhibitors + vasodilation Vasodilation The physiological widening of blood vessels by relaxing the underlying vascular smooth muscle. Pulmonary Hypertension Drugs of veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology > arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology |
|
|
Na+ nitroprusside Nitroprusside A powerful vasodilator used in emergencies to lower blood pressure or to improve cardiac function. It is also an indicator for free sulfhydryl groups in proteins. Nitrates for hypertensive emergency Hypertensive emergency A condition of markedly elevated blood pressure with diastolic pressure usually greater than 120 mm hg. Malignant hypertension is characterized by widespread vascular damage, papilledema, retinopathy, hypertensive encephalopathy, and renal dysfunction. Uncontrolled Hypertension |