Hyperbilirubinemia Hyperbilirubinemia A condition characterized by an abnormal increase of bilirubin in the blood, which may result in jaundice. Bilirubin, a breakdown product of heme, is normally excreted in the bile or further catabolized before excretion in the urine. Jaundice of the newborn Newborn An infant during the first 28 days after birth. Physical Examination of the Newborn is a broad term that refers to various conditions that can cause accumulation of bilirubin Bilirubin A bile pigment that is a degradation product of heme. Heme Metabolism during the first few days after birth. The condition is often noted because of visible yellowing of the skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions and sclera Sclera The white, opaque, fibrous, outer tunic of the eyeball, covering it entirely excepting the segment covered anteriorly by the cornea. It is essentially avascular but contains apertures for vessels, lymphatics, and nerves. Eye: Anatomy secondary to bilirubin Bilirubin A bile pigment that is a degradation product of heme. Heme Metabolism deposition. Because hyperbilirubinemia Hyperbilirubinemia A condition characterized by an abnormal increase of bilirubin in the blood, which may result in jaundice. Bilirubin, a breakdown product of heme, is normally excreted in the bile or further catabolized before excretion in the urine. Jaundice arises from physiological processes that accompany birth, it is usually an expected finding. However, hyperbilirubinemia Hyperbilirubinemia A condition characterized by an abnormal increase of bilirubin in the blood, which may result in jaundice. Bilirubin, a breakdown product of heme, is normally excreted in the bile or further catabolized before excretion in the urine. Jaundice in the neonate Neonate An infant during the first 28 days after birth. Physical Examination of the Newborn can also have pathological etiologies, including breastfeeding-related, blood group isoimmunization, metabolic disorders, and infection. Regardless of etiology, the primary goal of therapy in neonatal jaundice Neonatal jaundice Yellow discoloration of the skin; mucous membrane; and sclera in the newborn. It is a sign of neonatal hyperbilirubinemia. Most cases are transient self-limiting (physiological neonatal jaundice) occurring in the first week of life, but some can be a sign of pathological disorders, particularly liver diseases. Jaundice is to prevent the neurotoxic effect of indirect bilirubin Indirect Bilirubin Liver Function Tests, mainly kernicterus. When indicated, treatment mainly includes phototherapy and exchange transfusion.
Last updated: Dec 15, 2025
Hyperbilirubinemia Hyperbilirubinemia A condition characterized by an abnormal increase of bilirubin in the blood, which may result in jaundice. Bilirubin, a breakdown product of heme, is normally excreted in the bile or further catabolized before excretion in the urine. Jaundice of the newborn Newborn An infant during the first 28 days after birth. Physical Examination of the Newborn is defined as a yellow discoloration of the skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions and sclera Sclera The white, opaque, fibrous, outer tunic of the eyeball, covering it entirely excepting the segment covered anteriorly by the cornea. It is essentially avascular but contains apertures for vessels, lymphatics, and nerves. Eye: Anatomy of the newborn Newborn An infant during the first 28 days after birth. Physical Examination of the Newborn usually due to the tissue deposition of unconjugated bilirubin Bilirubin A bile pigment that is a degradation product of heme. Heme Metabolism, the end product of heme-protein catabolism.
Positive Coombs test: isoimmunization
Negative Coombs test
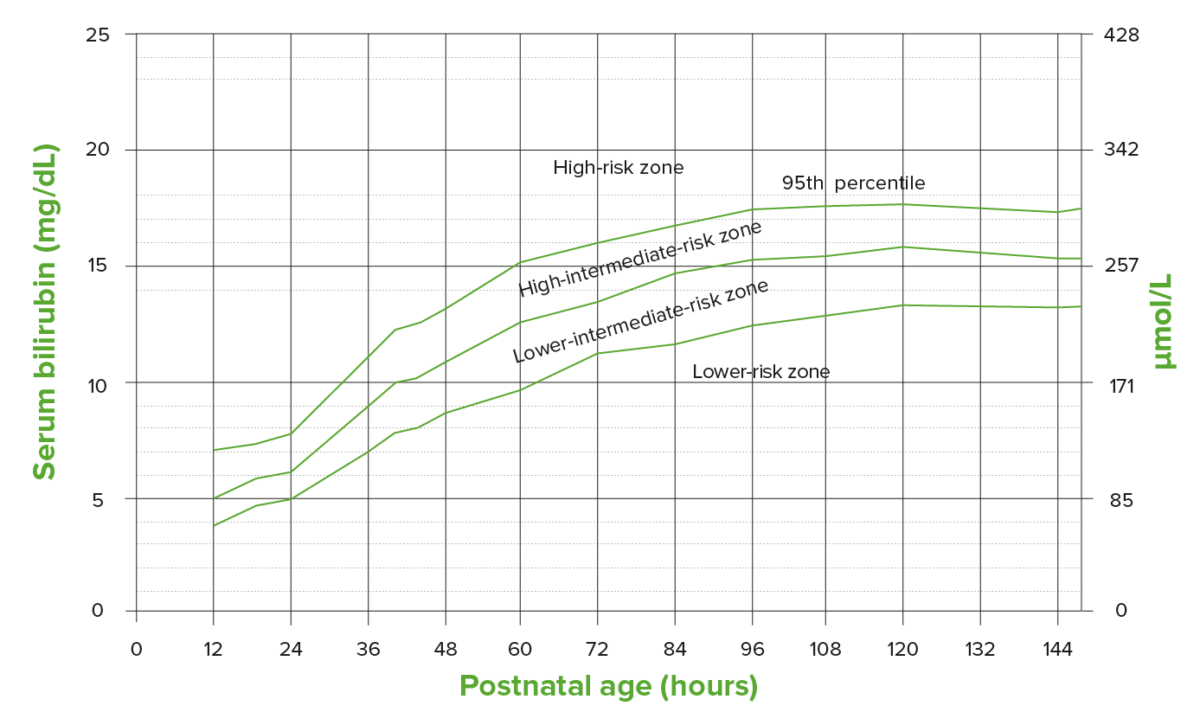
The Buthani nomogram identifying risk of subsequent total serum bilirubin level based on the hour-specific bilirubin level in newborns born at ≥ 35 weeks gestation
Image by Lecturio.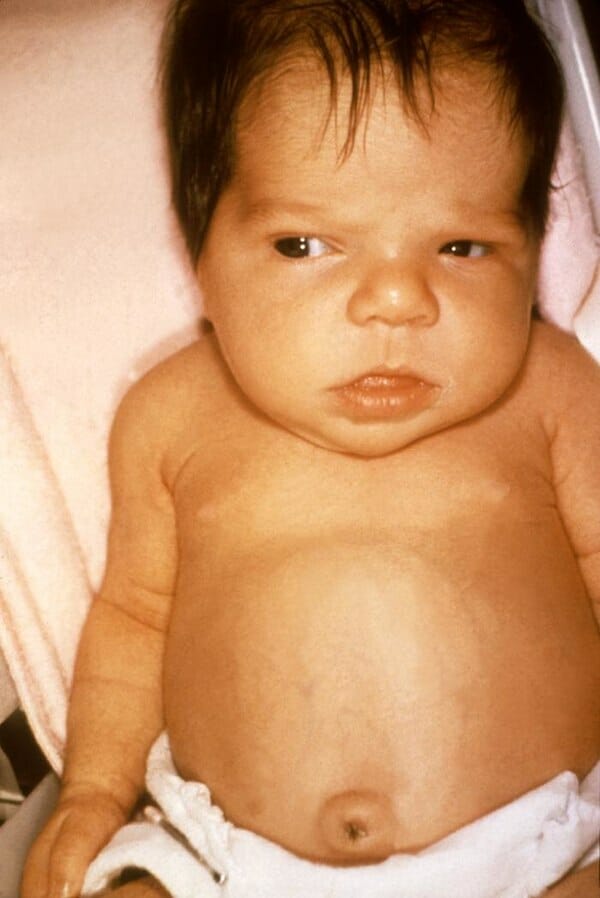
A 6-week-old girl with symptoms of jaundice due to hypothyroidism
Image: “Jaundice in newborn” by Dr. Hudson (CDC). License: Public Domain| Bilirubin Bilirubin A bile pigment that is a degradation product of heme. Heme Metabolism type | Bilirubin Bilirubin A bile pigment that is a degradation product of heme. Heme Metabolism peak (mg/dL) | Bilirubin Bilirubin A bile pigment that is a degradation product of heme. Heme Metabolism increase (mg/dL/day) | Comments/diseases | |
|---|---|---|---|---|
| May appear in 1st 24 hours | ||||
| Hemolytic/ hematoma Hematoma A collection of blood outside the blood vessels. Hematoma can be localized in an organ, space, or tissue. Intussusception (duration: variable Variable Variables represent information about something that can change. The design of the measurement scales, or of the methods for obtaining information, will determine the data gathered and the characteristics of that data. As a result, a variable can be qualitative or quantitative, and may be further classified into subgroups. Types of Variables) | Indirect | Unlimited | < 5 |
|
| Hemolytic + hepatotoxic (duration: variable Variable Variables represent information about something that can change. The design of the measurement scales, or of the methods for obtaining information, will determine the data gathered and the characteristics of that data. As a result, a variable can be qualitative or quantitative, and may be further classified into subgroups. Types of Variables) | Indirect/direct | Unlimited | < 5 |
|
| May appear in 2–4 days | ||||
| Physiologic (disappears in 4–9 days) | Indirect | 10–15 | < 5 | Duration/severity increases with degree of prematurity Prematurity Neonatal Respiratory Distress Syndrome |
| Metabolic (duration: variable Variable Variables represent information about something that can change. The design of the measurement scales, or of the methods for obtaining information, will determine the data gathered and the characteristics of that data. As a result, a variable can be qualitative or quantitative, and may be further classified into subgroups. Types of Variables) | Indirect | > 12–15 | < 5 |
|
| Hepatocellular damage (duration: variable Variable Variables represent information about something that can change. The design of the measurement scales, or of the methods for obtaining information, will determine the data gathered and the characteristics of that data. As a result, a variable can be qualitative or quantitative, and may be further classified into subgroups. Types of Variables) | Indirect/direct | Unlimited | < 5 |
|

A child receiving phototherapy
Image: “Baked Bean” by shannonpatrick17. License: CC BY 2.0Bilirubin-induced neurologic dysfunction (BIND):