Hyperaldosteronism is defined as the increased secretion Secretion Coagulation Studies of aldosterone Aldosterone A hormone secreted by the adrenal cortex that regulates electrolyte and water balance by increasing the renal retention of sodium and the excretion of potassium. Hyperkalemia from the zona glomerulosa Zona Glomerulosa The narrow subcapsular outer zone of the adrenal cortex. This zone produces a series of enzymes that convert pregnenolone to aldosterone. The final steps involve three successive oxidations by cytochrome p-450 cyp11b2. Adrenal Glands: Anatomy of the adrenal cortex Adrenal Cortex The outer layer of the adrenal gland. It is derived from mesoderm and comprised of three zones (outer zona glomerulosa, middle zona fasciculata, and inner zona reticularis) with each producing various steroids preferentially, such as aldosterone; hydrocortisone; dehydroepiandrosterone; and androstenedione. Adrenal cortex function is regulated by pituitary adrenocorticotropin. Adrenal Glands: Anatomy. Hyperaldosteronism may be primary (resulting from autonomous secretion Secretion Coagulation Studies), or secondary (resulting from physiological secretion Secretion Coagulation Studies due to stimulation of the RAAS RAAS A blood pressure regulating system of interacting components that include renin; angiotensinogen; angiotensin converting enzyme; angiotensin i; angiotensin ii; and angiotensinase. Renin, an enzyme produced in the kidney, acts on angiotensinogen, an alpha-2 globulin produced by the liver, forming angiotensin I. Angiotensin-converting enzyme, contained in the lung, acts on angiotensin I in the plasma converting it to angiotensin II, an extremely powerful vasoconstrictor. Angiotensin II causes contraction of the arteriolar and renal vascular smooth muscle, leading to retention of salt and water in the kidney and increased arterial blood pressure. In addition, angiotensin II stimulates the release of aldosterone from the adrenal cortex, which in turn also increases salt and water retention in the kidney. Angiotensin-converting enzyme also breaks down bradykinin, a powerful vasodilator and component of the kallikrein-kinin system. Adrenal Hormones). Classically, hyperaldosteronism presents with hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension, hypokalemia Hypokalemia Hypokalemia is defined as plasma potassium (K+) concentration < 3.5 mEq/L. Homeostatic mechanisms maintain plasma concentration between 3.5-5.2 mEq/L despite marked variation in dietary intake. Hypokalemia can be due to renal losses, GI losses, transcellular shifts, or poor dietary intake. Hypokalemia, and metabolic alkalosis Alkalosis A pathological condition that removes acid or adds base to the body fluids. Respiratory Alkalosis, although recent studies have suggested that hypokalemia Hypokalemia Hypokalemia is defined as plasma potassium (K+) concentration < 3.5 mEq/L. Homeostatic mechanisms maintain plasma concentration between 3.5-5.2 mEq/L despite marked variation in dietary intake. Hypokalemia can be due to renal losses, GI losses, transcellular shifts, or poor dietary intake. Hypokalemia is less common than originally thought in primary hyperaldosteronism. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension who are treatment resistant and/or associated with hypokalemia Hypokalemia Hypokalemia is defined as plasma potassium (K+) concentration < 3.5 mEq/L. Homeostatic mechanisms maintain plasma concentration between 3.5-5.2 mEq/L despite marked variation in dietary intake. Hypokalemia can be due to renal losses, GI losses, transcellular shifts, or poor dietary intake. Hypokalemia should be screened for hyperaldosteronism by determining their plasma Plasma The residual portion of blood that is left after removal of blood cells by centrifugation without prior blood coagulation. Transfusion Products aldosterone Aldosterone A hormone secreted by the adrenal cortex that regulates electrolyte and water balance by increasing the renal retention of sodium and the excretion of potassium. Hyperkalemia concentration and plasma renin activity Plasma renin activity Renal Artery Stenosis. Confirmatory tests and an abdominal CT scan are required to conclusively diagnose primary hyperaldosteronism. Management involves the use of aldosterone Aldosterone A hormone secreted by the adrenal cortex that regulates electrolyte and water balance by increasing the renal retention of sodium and the excretion of potassium. Hyperkalemia receptor Receptor Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors antagonists and surgical excision of any aldosterone-secreting tumors.
Last updated: Dec 30, 2024
Hyperaldosteronism is defined as an increased secretion Secretion Coagulation Studies of aldosterone Aldosterone A hormone secreted by the adrenal cortex that regulates electrolyte and water balance by increasing the renal retention of sodium and the excretion of potassium. Hyperkalemia from the zona glomerulosa Zona Glomerulosa The narrow subcapsular outer zone of the adrenal cortex. This zone produces a series of enzymes that convert pregnenolone to aldosterone. The final steps involve three successive oxidations by cytochrome p-450 cyp11b2. Adrenal Glands: Anatomy of the adrenal cortex Adrenal Cortex The outer layer of the adrenal gland. It is derived from mesoderm and comprised of three zones (outer zona glomerulosa, middle zona fasciculata, and inner zona reticularis) with each producing various steroids preferentially, such as aldosterone; hydrocortisone; dehydroepiandrosterone; and androstenedione. Adrenal cortex function is regulated by pituitary adrenocorticotropin. Adrenal Glands: Anatomy.
| Type of hyperaldosteronism | Etiology |
|---|---|
| Primary hyperaldosteronism |
|
| Secondary hyperaldosteronism |
|
The primary role of aldosterone Aldosterone A hormone secreted by the adrenal cortex that regulates electrolyte and water balance by increasing the renal retention of sodium and the excretion of potassium. Hyperkalemia is to increase BP, which occurs by an increase in sodium Sodium A member of the alkali group of metals. It has the atomic symbol na, atomic number 11, and atomic weight 23. Hyponatremia and, thus, increased water reabsorption from the kidneys Kidneys The kidneys are a pair of bean-shaped organs located retroperitoneally against the posterior wall of the abdomen on either side of the spine. As part of the urinary tract, the kidneys are responsible for blood filtration and excretion of water-soluble waste in the urine. Kidneys: Anatomy, while excreting potassium Potassium An element in the alkali group of metals with an atomic symbol k, atomic number 19, and atomic weight 39. 10. It is the chief cation in the intracellular fluid of muscle and other cells. Potassium ion is a strong electrolyte that plays a significant role in the regulation of fluid volume and maintenance of the water-electrolyte balance. Hyperkalemia and hydrogen ions.
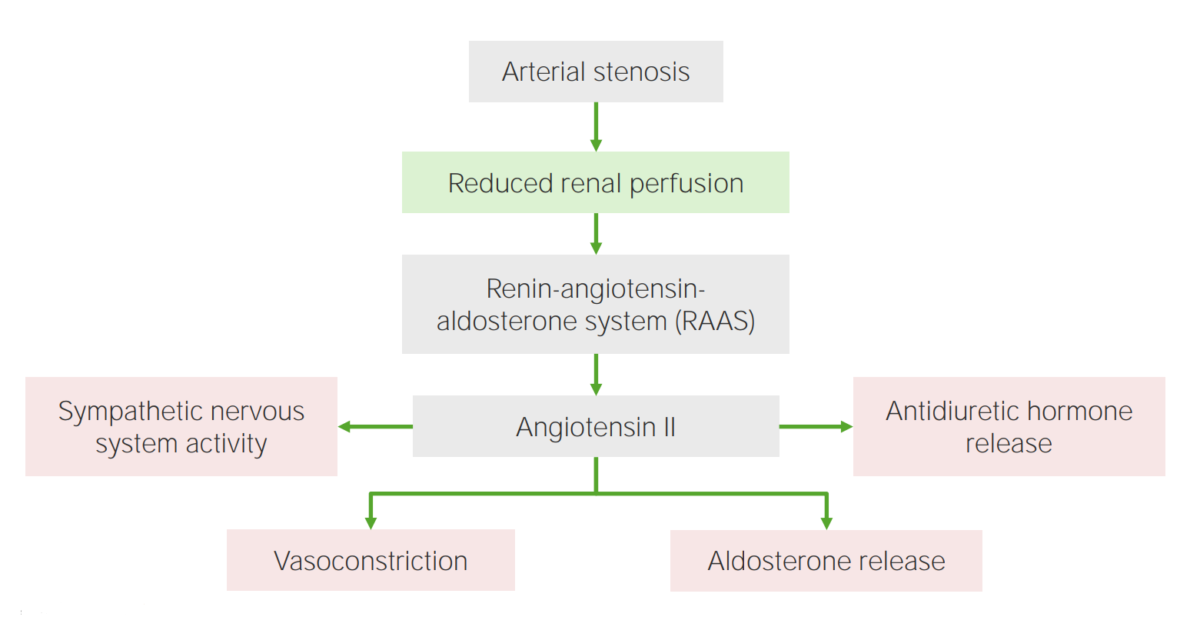
Effects of angiotensin II, which plays a key role in the renin-angiotensin-aldosterone system.
Image by Lecturio.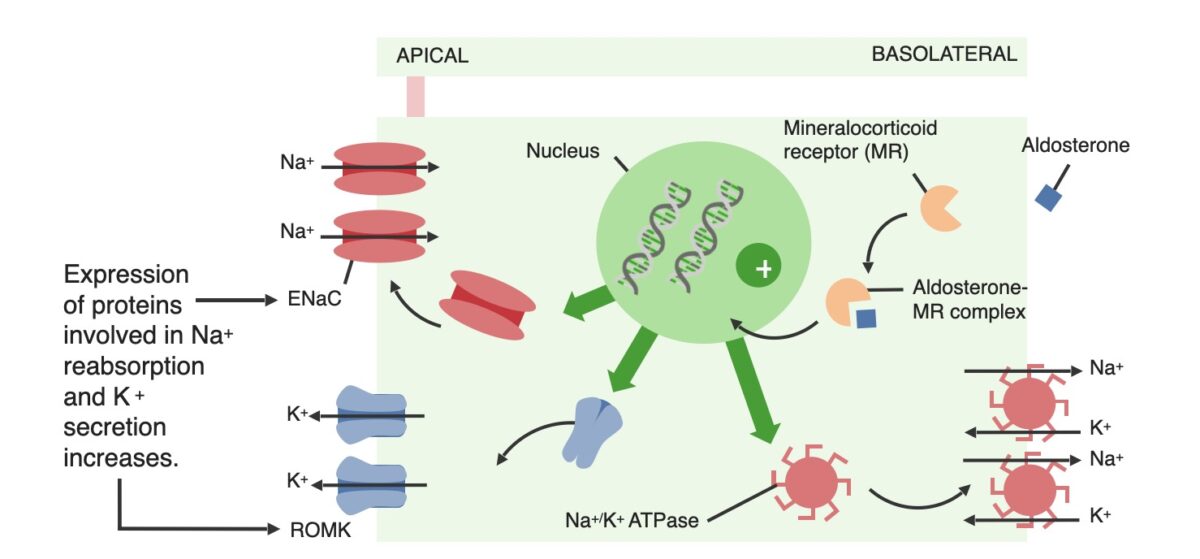
Effects of aldosterone on the principal cells within the distal renal tubules:
ENaC: epithelial sodium channel
ROMK: renal outer medullary potassium
The diagnoses of primary and secondary hyperaldosteronism are made based on biochemical testing. Imaging is required to identify the etiology in cases of primary hyperaldosteronism.
Imaging is used to differentiate a unilateral adrenal adenoma Adrenal Adenoma Cushing Syndrome from bilateral adrenal hyperplasia Hyperplasia An increase in the number of cells in a tissue or organ without tumor formation. It differs from hypertrophy, which is an increase in bulk without an increase in the number of cells. Cellular Adaptation once a biochemical diagnosis of primary hyperaldosteronism is made.