Hepatorenal syndrome Hepatorenal Syndrome Hepatorenal syndrome (HRS) is a potentially reversible cause of acute kidney injury that develops secondary to liver disease. The main cause of HRS is hypovolemia, often as a result of forced diuresis or drainage of ascites. This leads to renal vasoconstriction resulting in hypoperfusion of the kidneys. Hepatorenal Syndrome ( HRS HRS Hepatorenal syndrome (HRS) is a potentially reversible cause of acute kidney injury that develops secondary to liver disease. The main cause of hrs is hypovolemia, often as a result of forced diuresis or drainage of ascites. This leads to renal vasoconstriction resulting in hypoperfusion of the kidneys. Hepatorenal Syndrome) is a “functional” type of acute kidney injury Acute Kidney Injury Acute kidney injury refers to sudden and often reversible loss of renal function, which develops over days or weeks. Azotemia refers to elevated levels of nitrogen-containing substances in the blood that accompany AKI, which include BUN and creatinine. Acute Kidney Injury ( AKI AKI Acute kidney injury refers to sudden and often reversible loss of renal function, which develops over days or weeks. Azotemia refers to elevated levels of nitrogen-containing substances in the blood that accompany AKI, which include BUN and creatinine. Acute Kidney Injury) in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship who have portal hypertension Portal hypertension Portal hypertension is increased pressure in the portal venous system. This increased pressure can lead to splanchnic vasodilation, collateral blood flow through portosystemic anastomoses, and increased hydrostatic pressure. There are a number of etiologies, including cirrhosis, right-sided congestive heart failure, schistosomiasis, portal vein thrombosis, hepatitis, and Budd-Chiari syndrome. Portal Hypertension, usually due to cirrhosis Cirrhosis Cirrhosis is a late stage of hepatic parenchymal necrosis and scarring (fibrosis) most commonly due to hepatitis C infection and alcoholic liver disease. Patients may present with jaundice, ascites, and hepatosplenomegaly. Cirrhosis can also cause complications such as hepatic encephalopathy, portal hypertension, portal vein thrombosis, and hepatorenal syndrome. Cirrhosis. HRS HRS Hepatorenal syndrome (HRS) is a potentially reversible cause of acute kidney injury that develops secondary to liver disease. The main cause of hrs is hypovolemia, often as a result of forced diuresis or drainage of ascites. This leads to renal vasoconstriction resulting in hypoperfusion of the kidneys. Hepatorenal Syndrome may also be caused by other liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy diseases which are associated with portal hypertension Portal hypertension Portal hypertension is increased pressure in the portal venous system. This increased pressure can lead to splanchnic vasodilation, collateral blood flow through portosystemic anastomoses, and increased hydrostatic pressure. There are a number of etiologies, including cirrhosis, right-sided congestive heart failure, schistosomiasis, portal vein thrombosis, hepatitis, and Budd-Chiari syndrome. Portal Hypertension, which causes decreased systemic arterial blood volume and activation of neurohormonal mechanisms, including the renin-angiotensin-aldosterone system Renin-angiotensin-aldosterone system A blood pressure regulating system of interacting components that include renin; angiotensinogen; angiotensin converting enzyme; angiotensin i; angiotensin ii; and angiotensinase. Renin, an enzyme produced in the kidney, acts on angiotensinogen, an alpha-2 globulin produced by the liver, forming angiotensin I. Angiotensin-converting enzyme, contained in the lung, acts on angiotensin I in the plasma converting it to angiotensin II, an extremely powerful vasoconstrictor. Angiotensin II causes contraction of the arteriolar and renal vascular smooth muscle, leading to retention of salt and water in the kidney and increased arterial blood pressure. In addition, angiotensin II stimulates the release of aldosterone from the adrenal cortex, which in turn also increases salt and water retention in the kidney. Angiotensin-converting enzyme also breaks down bradykinin, a powerful vasodilator and component of the kallikrein-kinin system. Adrenal Hormones. The resulting vasoconstriction Vasoconstriction The physiological narrowing of blood vessels by contraction of the vascular smooth muscle. Vascular Resistance, Flow, and Mean Arterial Pressure and reduced renal perfusion trigger Trigger The type of signal that initiates the inspiratory phase by the ventilator Invasive Mechanical Ventilation the release of vasodilatory substances like nitric oxide Nitric Oxide A free radical gas produced endogenously by a variety of mammalian cells, synthesized from arginine by nitric oxide synthase. Nitric oxide is one of the endothelium-dependent relaxing factors released by the vascular endothelium and mediates vasodilation. It also inhibits platelet aggregation, induces disaggregation of aggregated platelets, and inhibits platelet adhesion to the vascular endothelium. Nitric oxide activates cytosolic guanylate cyclase and thus elevates intracellular levels of cyclic gmp. Pulmonary Hypertension Drugs, which induces splanchnic arterial vasodilatation, leading to a decrease in systemic vascular resistance Resistance Physiologically, the opposition to flow of air caused by the forces of friction. As a part of pulmonary function testing, it is the ratio of driving pressure to the rate of air flow. Ventilation: Mechanics of Breathing and effective circulating volume Effective circulating volume Renal Sodium and Water Regulation, thereby exacerbating renal hypoperfusion. HRS HRS Hepatorenal syndrome (HRS) is a potentially reversible cause of acute kidney injury that develops secondary to liver disease. The main cause of hrs is hypovolemia, often as a result of forced diuresis or drainage of ascites. This leads to renal vasoconstriction resulting in hypoperfusion of the kidneys. Hepatorenal Syndrome is a diagnosis of exclusion, and is associated with a poor prognosis Prognosis A prediction of the probable outcome of a disease based on a individual's condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas. Without treatment, most patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship die within weeks of the onset of AKI AKI Acute kidney injury refers to sudden and often reversible loss of renal function, which develops over days or weeks. Azotemia refers to elevated levels of nitrogen-containing substances in the blood that accompany AKI, which include BUN and creatinine. Acute Kidney Injury. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship typically present with a progressive rise in serum creatinine, a benign Benign Fibroadenoma urine sediment, no (or minimal) proteinuria Proteinuria The presence of proteins in the urine, an indicator of kidney diseases. Nephrotic Syndrome in Children, and a low urine sodium Sodium A member of the alkali group of metals. It has the atomic symbol na, atomic number 11, and atomic weight 23. Hyponatremia concentration. Ascites Ascites Ascites is the pathologic accumulation of fluid within the peritoneal cavity that occurs due to an osmotic and/or hydrostatic pressure imbalance secondary to portal hypertension (cirrhosis, heart failure) or non-portal hypertension (hypoalbuminemia, malignancy, infection). Ascites is often present, and severe cases are associated with oliguria Oliguria Decreased urine output that is below the normal range. Oliguria can be defined as urine output of less than or equal to 0. 5 or 1 ml/kg/hr depending on the age. Renal Potassium Regulation. Treatment is aimed at improving liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy function, if possible. Medical therapy includes increasing the systemic blood pressure with norepinephrine Norepinephrine Precursor of epinephrine that is secreted by the adrenal medulla and is a widespread central and autonomic neurotransmitter. Norepinephrine is the principal transmitter of most postganglionic sympathetic fibers, and of the diffuse projection system in the brain that arises from the locus ceruleus. Receptors and Neurotransmitters of the CNS and albumin Albumin Serum albumin from humans. It is an essential carrier of both endogenous substances, such as fatty acids and bilirubin, and of xenobiotics in the blood. Liver Function Tests infusions, and administering agents that cause splanchnic vasoconstriction Vasoconstriction The physiological narrowing of blood vessels by contraction of the vascular smooth muscle. Vascular Resistance, Flow, and Mean Arterial Pressure (e.g., terlipressin). Transjugular intrahepatic portosystemic shunt Transjugular intrahepatic portosystemic shunt A type of surgical portosystemic shunt to reduce portal hypertension with associated complications of esophageal varices and ascites. It is performed percutaneously through the jugular vein and involves the creation of an intrahepatic shunt between the hepatic vein and portal vein. The channel is maintained by a metallic stent. The procedure can be performed in patients who have failed sclerotherapy and is an additional option to the surgical techniques of portocaval, mesocaval, and splenorenal shunts. It takes one to three hours to perform. Ascites (TIPS) may be successful, and dialysis Dialysis Renal replacement therapy refers to dialysis and/or kidney transplantation. Dialysis is a procedure by which toxins and excess water are removed from the circulation. Hemodialysis and peritoneal dialysis (PD) are the two types of dialysis, and their primary difference is the location of the filtration process (external to the body in hemodialysis versus inside the body for PD). Peritoneal Dialysis and Hemodialysis is a temporizing solution while waiting for liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy transplant. The prognosis Prognosis A prediction of the probable outcome of a disease based on a individual's condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas of patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with HRS HRS Hepatorenal syndrome (HRS) is a potentially reversible cause of acute kidney injury that develops secondary to liver disease. The main cause of hrs is hypovolemia, often as a result of forced diuresis or drainage of ascites. This leads to renal vasoconstriction resulting in hypoperfusion of the kidneys. Hepatorenal Syndrome is highly dependent upon reversal of the hepatic failure Hepatic failure Severe inability of the liver to perform its normal metabolic functions, as evidenced by severe jaundice and abnormal serum levels of ammonia; bilirubin; alkaline phosphatase; aspartate aminotransferase; lactate dehydrogenases; and albumin/globulin ratio. Autoimmune Hepatitis, whether spontaneous, following medical therapy, or following transplantation.
Last updated: Dec 15, 2025
Hepatorenal syndrome Hepatorenal Syndrome Hepatorenal syndrome (HRS) is a potentially reversible cause of acute kidney injury that develops secondary to liver disease. The main cause of HRS is hypovolemia, often as a result of forced diuresis or drainage of ascites. This leads to renal vasoconstriction resulting in hypoperfusion of the kidneys. Hepatorenal Syndrome ( HRS HRS Hepatorenal syndrome (HRS) is a potentially reversible cause of acute kidney injury that develops secondary to liver disease. The main cause of hrs is hypovolemia, often as a result of forced diuresis or drainage of ascites. This leads to renal vasoconstriction resulting in hypoperfusion of the kidneys. Hepatorenal Syndrome) is associated with portal hypertension Portal hypertension Portal hypertension is increased pressure in the portal venous system. This increased pressure can lead to splanchnic vasodilation, collateral blood flow through portosystemic anastomoses, and increased hydrostatic pressure. There are a number of etiologies, including cirrhosis, right-sided congestive heart failure, schistosomiasis, portal vein thrombosis, hepatitis, and Budd-Chiari syndrome. Portal Hypertension due to:[1]
Trigger Trigger The type of signal that initiates the inspiratory phase by the ventilator Invasive Mechanical Ventilation factors are any interventions or conditions that cause arterial hypovolemia Hypovolemia Sepsis in Children:
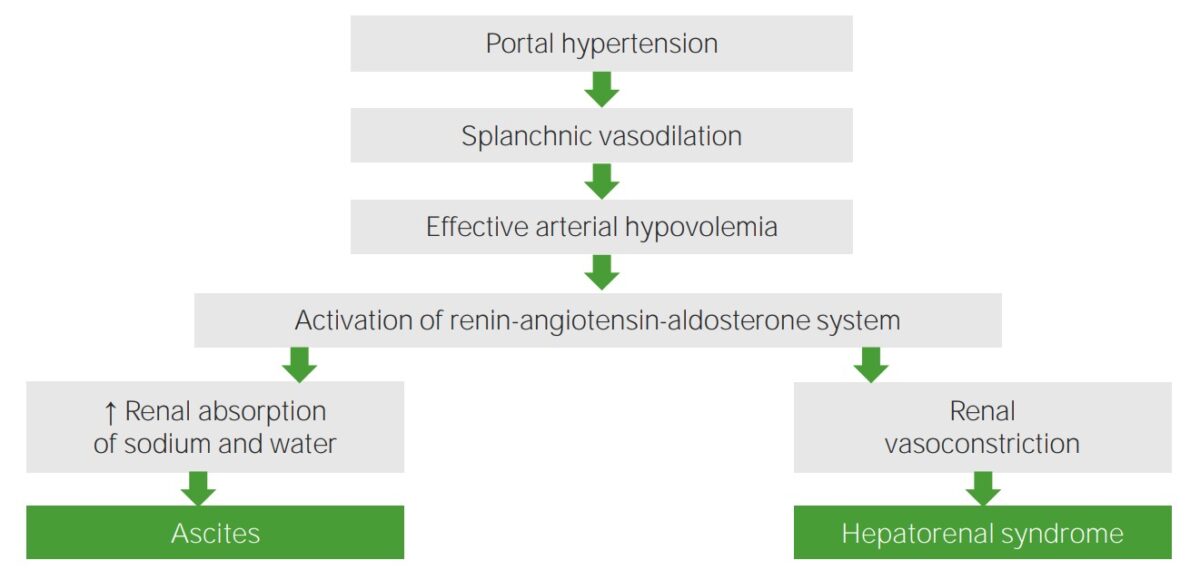
Pathophysiology of hepatorenal syndrome
Image by Lecturio.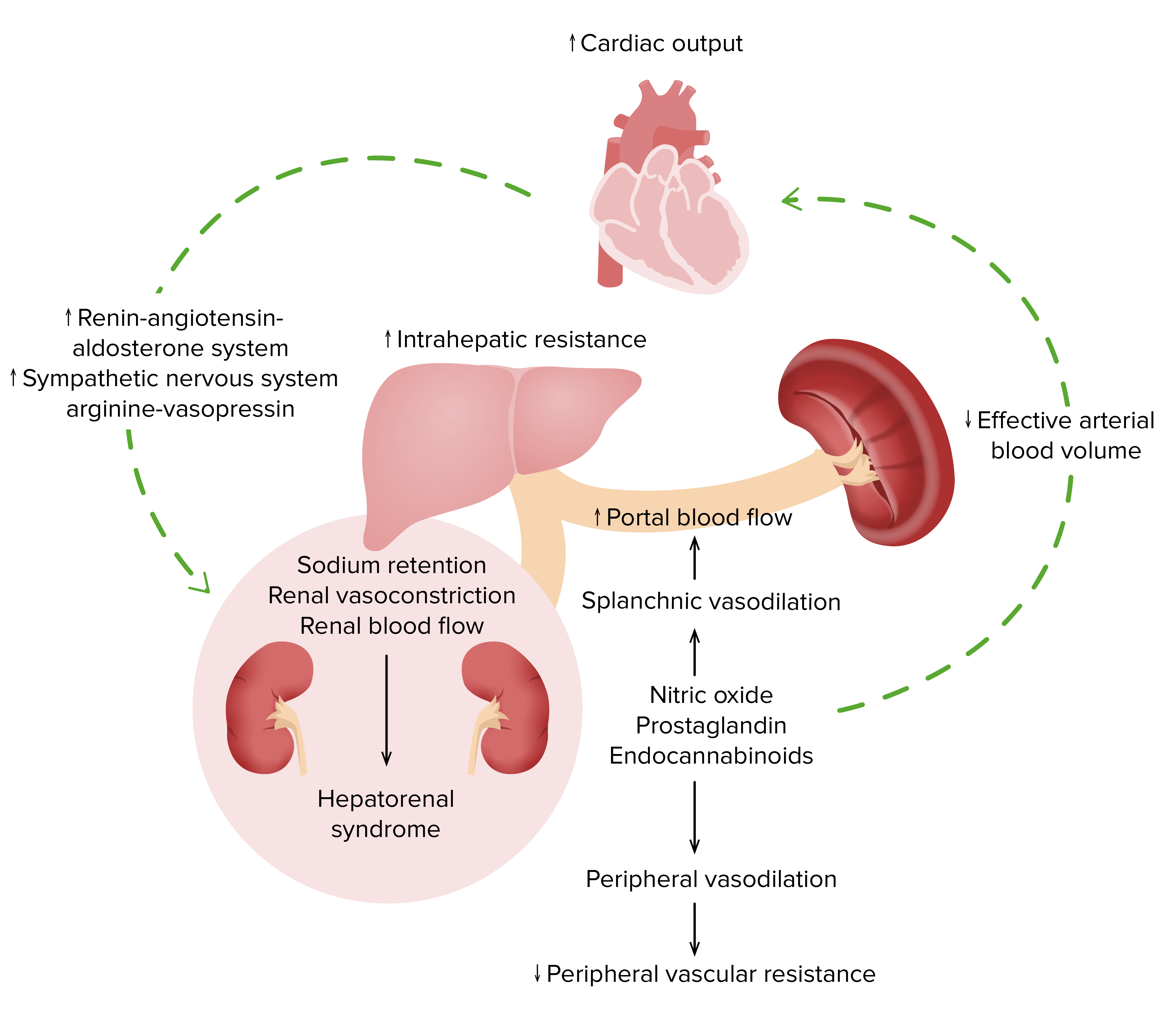
Pathophysiology of hepatorenal syndrome
Image by Lecturio.Diagnostic criteria may vary depending on practice location. The following information is based on US, UK, and European recommendations.

Lower extremity edema due to fluid retention, which is similar to the peripheral edema which can occur in a patient with hepatorenal syndrome
Image: “Itraconazole associated quadriparesis and edema” by National Aspergillosis Centre, Education and Research Centre, University Hospital of South Manchester (Wythenshawe Hospital), Southmoor Road, Manchester M23 9LT, UK. License: CC BY 2.0HRS HRS Hepatorenal syndrome (HRS) is a potentially reversible cause of acute kidney injury that develops secondary to liver disease. The main cause of hrs is hypovolemia, often as a result of forced diuresis or drainage of ascites. This leads to renal vasoconstriction resulting in hypoperfusion of the kidneys. Hepatorenal Syndrome is a diagnosis of exclusion. There has been a recent shift in the classification of HRS HRS Hepatorenal syndrome (HRS) is a potentially reversible cause of acute kidney injury that develops secondary to liver disease. The main cause of hrs is hypovolemia, often as a result of forced diuresis or drainage of ascites. This leads to renal vasoconstriction resulting in hypoperfusion of the kidneys. Hepatorenal Syndrome. Because AKI AKI Acute kidney injury refers to sudden and often reversible loss of renal function, which develops over days or weeks. Azotemia refers to elevated levels of nitrogen-containing substances in the blood that accompany AKI, which include BUN and creatinine. Acute Kidney Injury is common in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with cirrhosis Cirrhosis Cirrhosis is a late stage of hepatic parenchymal necrosis and scarring (fibrosis) most commonly due to hepatitis C infection and alcoholic liver disease. Patients may present with jaundice, ascites, and hepatosplenomegaly. Cirrhosis can also cause complications such as hepatic encephalopathy, portal hypertension, portal vein thrombosis, and hepatorenal syndrome. Cirrhosis for a multitude of reasons, the International Club of Ascites Ascites Ascites is the pathologic accumulation of fluid within the peritoneal cavity that occurs due to an osmotic and/or hydrostatic pressure imbalance secondary to portal hypertension (cirrhosis, heart failure) or non-portal hypertension (hypoalbuminemia, malignancy, infection). Ascites proposed the following staging Staging Methods which attempt to express in replicable terms the extent of the neoplasm in the patient. Grading, Staging, and Metastasis and classification:
AKI AKI Acute kidney injury refers to sudden and often reversible loss of renal function, which develops over days or weeks. Azotemia refers to elevated levels of nitrogen-containing substances in the blood that accompany AKI, which include BUN and creatinine. Acute Kidney Injury definition and staging Staging Methods which attempt to express in replicable terms the extent of the neoplasm in the patient. Grading, Staging, and Metastasis for patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with cirrhosis Cirrhosis Cirrhosis is a late stage of hepatic parenchymal necrosis and scarring (fibrosis) most commonly due to hepatitis C infection and alcoholic liver disease. Patients may present with jaundice, ascites, and hepatosplenomegaly. Cirrhosis can also cause complications such as hepatic encephalopathy, portal hypertension, portal vein thrombosis, and hepatorenal syndrome. Cirrhosis:[1,3,7,13]
HRS HRS Hepatorenal syndrome (HRS) is a potentially reversible cause of acute kidney injury that develops secondary to liver disease. The main cause of hrs is hypovolemia, often as a result of forced diuresis or drainage of ascites. This leads to renal vasoconstriction resulting in hypoperfusion of the kidneys. Hepatorenal Syndrome classification with diagnostic criteria:
The history and workup should focus on ruling out other potential causes of renal dysfunction, such as:
Laboratory studies may demonstrate the following findings in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with HRS HRS Hepatorenal syndrome (HRS) is a potentially reversible cause of acute kidney injury that develops secondary to liver disease. The main cause of hrs is hypovolemia, often as a result of forced diuresis or drainage of ascites. This leads to renal vasoconstriction resulting in hypoperfusion of the kidneys. Hepatorenal Syndrome:
Imaging, such as ultrasonography, may be used to exclude obstruction or parenchymal kidney disease.
Management may vary depending on practice location and availability of therapeutics. The following information is based on US, UK, and European recommendations for HRS-AKI. Information on optimal therapy for HRS-NAKI is currently lacking. See your local guidelines for additional recommendations.
The following measures can be implemented to correct potential AKI AKI Acute kidney injury refers to sudden and often reversible loss of renal function, which develops over days or weeks. Azotemia refers to elevated levels of nitrogen-containing substances in the blood that accompany AKI, which include BUN and creatinine. Acute Kidney Injury from hypovolemia Hypovolemia Sepsis in Children:
Once the diagnosis of HRS-AKI is established, vasoconstrictors and albumin Albumin Serum albumin from humans. It is an essential carrier of both endogenous substances, such as fatty acids and bilirubin, and of xenobiotics in the blood. Liver Function Tests are the mainstay of therapy. Vasoconstrictors are generally continued until the patient’s creatinine returns to baseline (or up to 14 days).
If terlipressin is available:[3,4,7,9]
Alternative 1:[3,7,9]
Alternative 2 (all 3 should be given; lower efficacy than the above options):[3,7]
The following options should be considered based on specialty recommendations and clinical scenario:
Avoiding precipitating factors is important in preventing HRS-AKI, including:
Prerenal disease: presents with similar laboratory findings (↑ serum creatinine and ↑ BUN:creatinine ratio BUN:creatinine Ratio Kidney Function Tests) and similar urine findings (low sodium Sodium A member of the alkali group of metals. It has the atomic symbol na, atomic number 11, and atomic weight 23. Hyponatremia excretion in urine). Hepatorenal syndrome Hepatorenal Syndrome Hepatorenal syndrome (HRS) is a potentially reversible cause of acute kidney injury that develops secondary to liver disease. The main cause of HRS is hypovolemia, often as a result of forced diuresis or drainage of ascites. This leads to renal vasoconstriction resulting in hypoperfusion of the kidneys. Hepatorenal Syndrome can be differentiated from prerenal failure through an IV fluid volume expansion challenge with intravenous albumin Albumin Serum albumin from humans. It is an essential carrier of both endogenous substances, such as fatty acids and bilirubin, and of xenobiotics in the blood. Liver Function Tests. Giving fluids improves prerenal disease, but not HRS HRS Hepatorenal syndrome (HRS) is a potentially reversible cause of acute kidney injury that develops secondary to liver disease. The main cause of hrs is hypovolemia, often as a result of forced diuresis or drainage of ascites. This leads to renal vasoconstriction resulting in hypoperfusion of the kidneys. Hepatorenal Syndrome. In patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with cirrhosis Cirrhosis Cirrhosis is a late stage of hepatic parenchymal necrosis and scarring (fibrosis) most commonly due to hepatitis C infection and alcoholic liver disease. Patients may present with jaundice, ascites, and hepatosplenomegaly. Cirrhosis can also cause complications such as hepatic encephalopathy, portal hypertension, portal vein thrombosis, and hepatorenal syndrome. Cirrhosis, prerenal disease can be caused by GI fluid losses ( diarrhea Diarrhea Diarrhea is defined as ≥ 3 watery or loose stools in a 24-hour period. There are a multitude of etiologies, which can be classified based on the underlying mechanism of disease. The duration of symptoms (acute or chronic) and characteristics of the stools (e.g., watery, bloody, steatorrheic, mucoid) can help guide further diagnostic evaluation. Diarrhea), bleeding, diuretics Diuretics Agents that promote the excretion of urine through their effects on kidney function. Heart Failure and Chronic Coronary Syndrome Medication, or NSAIDs NSAIDS Primary vs Secondary Headaches.
Acute tubular necrosis Necrosis The death of cells in an organ or tissue due to disease, injury or failure of the blood supply. Ischemic Cell Damage (ATN): parenchymal kidney disease, such as membranoproliferative glomerulonephritis Membranoproliferative Glomerulonephritis Membranoproliferative glomerulonephritis (MPGN) is also known as mesangiocapillary glomerulonephritis. Membranoproliferative glomerulonephritis is a pattern of glomerular injury characterized by mesangial hypercellularity, endocapillary proliferation, and thickening of the glomerular basement membrane (double contour formation). Membranoproliferative Glomerulonephritis, IgA IgA Represents 15-20% of the human serum immunoglobulins, mostly as the 4-chain polymer in humans or dimer in other mammals. Secretory iga is the main immunoglobulin in secretions. Immunoglobulins: Types and Functions nephropathy, or diabetic nephropathy Diabetic nephropathy Kidney injuries associated with diabetes mellitus and affecting kidney glomerulus; arterioles; kidney tubules; and the interstitium. Clinical signs include persistent proteinuria, from microalbuminuria progressing to albuminuria of greater than 300 mg/24 h, leading to reduced glomerular filtration rate and end-stage renal disease. Chronic Diabetic Complications, can be associated with AKI AKI Acute kidney injury refers to sudden and often reversible loss of renal function, which develops over days or weeks. Azotemia refers to elevated levels of nitrogen-containing substances in the blood that accompany AKI, which include BUN and creatinine. Acute Kidney Injury but may also coexist with HRS HRS Hepatorenal syndrome (HRS) is a potentially reversible cause of acute kidney injury that develops secondary to liver disease. The main cause of hrs is hypovolemia, often as a result of forced diuresis or drainage of ascites. This leads to renal vasoconstriction resulting in hypoperfusion of the kidneys. Hepatorenal Syndrome. Nephrotoxic agents Nephrotoxic Agents Surgical Complications such as aminoglycosides Aminoglycosides Aminoglycosides are a class of antibiotics including gentamicin, tobramycin, amikacin, neomycin, plazomicin, and streptomycin. The class binds the 30S ribosomal subunit to inhibit bacterial protein synthesis. Unlike other medications with a similar mechanism of action, aminoglycosides are bactericidal. Aminoglycosides or radiocontrast agents can precipitate ATN that is reversible after withdrawing the offending agent. Addressing the underlying cause of AKI AKI Acute kidney injury refers to sudden and often reversible loss of renal function, which develops over days or weeks. Azotemia refers to elevated levels of nitrogen-containing substances in the blood that accompany AKI, which include BUN and creatinine. Acute Kidney Injury is essential because of the marked difference in prognosis Prognosis A prediction of the probable outcome of a disease based on a individual’s condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas than with HRS HRS Hepatorenal syndrome (HRS) is a potentially reversible cause of acute kidney injury that develops secondary to liver disease. The main cause of hrs is hypovolemia, often as a result of forced diuresis or drainage of ascites. This leads to renal vasoconstriction resulting in hypoperfusion of the kidneys. Hepatorenal Syndrome alone. Most causes of prerenal disease and ATN are reversible.
Infection ( sepsis Sepsis Systemic inflammatory response syndrome with a proven or suspected infectious etiology. When sepsis is associated with organ dysfunction distant from the site of infection, it is called severe sepsis. When sepsis is accompanied by hypotension despite adequate fluid infusion, it is called septic shock. Sepsis and Septic Shock or spontaneous bacterial peritonitis Spontaneous Bacterial Peritonitis Ascites ( SBP SBP Ascites): infection can be associated with AKI AKI Acute kidney injury refers to sudden and often reversible loss of renal function, which develops over days or weeks. Azotemia refers to elevated levels of nitrogen-containing substances in the blood that accompany AKI, which include BUN and creatinine. Acute Kidney Injury in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with chronic liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy disease/ cirrhosis Cirrhosis Cirrhosis is a late stage of hepatic parenchymal necrosis and scarring (fibrosis) most commonly due to hepatitis C infection and alcoholic liver disease. Patients may present with jaundice, ascites, and hepatosplenomegaly. Cirrhosis can also cause complications such as hepatic encephalopathy, portal hypertension, portal vein thrombosis, and hepatorenal syndrome. Cirrhosis. However, the presence of SBP SBP Ascites does not exclude the diagnosis of HRS HRS Hepatorenal syndrome (HRS) is a potentially reversible cause of acute kidney injury that develops secondary to liver disease. The main cause of hrs is hypovolemia, often as a result of forced diuresis or drainage of ascites. This leads to renal vasoconstriction resulting in hypoperfusion of the kidneys. Hepatorenal Syndrome. An episode of sepsis Sepsis Systemic inflammatory response syndrome with a proven or suspected infectious etiology. When sepsis is associated with organ dysfunction distant from the site of infection, it is called severe sepsis. When sepsis is accompanied by hypotension despite adequate fluid infusion, it is called septic shock. Sepsis and Septic Shock with hypotension Hypotension Hypotension is defined as low blood pressure, specifically < 90/60 mm Hg, and is most commonly a physiologic response. Hypotension may be mild, serious, or life threatening, depending on the cause. Hypotension can cause a rapid rise in creatinine, contrasted with the more gradual rise with HRS HRS Hepatorenal syndrome (HRS) is a potentially reversible cause of acute kidney injury that develops secondary to liver disease. The main cause of hrs is hypovolemia, often as a result of forced diuresis or drainage of ascites. This leads to renal vasoconstriction resulting in hypoperfusion of the kidneys. Hepatorenal Syndrome. Treatment of the infection usually results in restoration of renal perfusion and an improvement in kidney function. However, with HRS HRS Hepatorenal syndrome (HRS) is a potentially reversible cause of acute kidney injury that develops secondary to liver disease. The main cause of hrs is hypovolemia, often as a result of forced diuresis or drainage of ascites. This leads to renal vasoconstriction resulting in hypoperfusion of the kidneys. Hepatorenal Syndrome not due to infection, the prognosis Prognosis A prediction of the probable outcome of a disease based on a individual’s condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas is poor.
Beta-blockers Beta-blockers Drugs that bind to but do not activate beta-adrenergic receptors thereby blocking the actions of beta-adrenergic agonists. Adrenergic beta-antagonists are used for treatment of hypertension, cardiac arrhythmias, angina pectoris, glaucoma, migraine headaches, and anxiety. Class 2 Antiarrhythmic Drugs (Beta Blockers): often used in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with cirrhosis Cirrhosis Cirrhosis is a late stage of hepatic parenchymal necrosis and scarring (fibrosis) most commonly due to hepatitis C infection and alcoholic liver disease. Patients may present with jaundice, ascites, and hepatosplenomegaly. Cirrhosis can also cause complications such as hepatic encephalopathy, portal hypertension, portal vein thrombosis, and hepatorenal syndrome. Cirrhosis and ascites Ascites Ascites is the pathologic accumulation of fluid within the peritoneal cavity that occurs due to an osmotic and/or hydrostatic pressure imbalance secondary to portal hypertension (cirrhosis, heart failure) or non-portal hypertension (hypoalbuminemia, malignancy, infection). Ascites but may cause hypotension Hypotension Hypotension is defined as low blood pressure, specifically < 90/60 mm Hg, and is most commonly a physiologic response. Hypotension may be mild, serious, or life threatening, depending on the cause. Hypotension and AKI AKI Acute kidney injury refers to sudden and often reversible loss of renal function, which develops over days or weeks. Azotemia refers to elevated levels of nitrogen-containing substances in the blood that accompany AKI, which include BUN and creatinine. Acute Kidney Injury. Discontinuing beta-blockers Beta-blockers Drugs that bind to but do not activate beta-adrenergic receptors thereby blocking the actions of beta-adrenergic agonists. Adrenergic beta-antagonists are used for treatment of hypertension, cardiac arrhythmias, angina pectoris, glaucoma, migraine headaches, and anxiety. Class 2 Antiarrhythmic Drugs (Beta Blockers) may lead to resolution of the renal function decline and clarify that the diagnosis is not HRS HRS Hepatorenal syndrome (HRS) is a potentially reversible cause of acute kidney injury that develops secondary to liver disease. The main cause of hrs is hypovolemia, often as a result of forced diuresis or drainage of ascites. This leads to renal vasoconstriction resulting in hypoperfusion of the kidneys. Hepatorenal Syndrome.
Diagnosis Codes:
This code is used to diagnose
hepatorenal syndrome
Hepatorenal Syndrome
Hepatorenal syndrome (HRS) is a potentially reversible cause of acute kidney injury that develops secondary to liver disease. The main cause of HRS is hypovolemia, often as a result of forced diuresis or drainage of ascites. This leads to renal vasoconstriction resulting in hypoperfusion of the kidneys.
Hepatorenal Syndrome (
HRS
HRS
Hepatorenal syndrome (HRS) is a potentially reversible cause of acute kidney injury that develops secondary to liver disease. The main cause of hrs is hypovolemia, often as a result of forced diuresis or drainage of ascites. This leads to renal vasoconstriction resulting in hypoperfusion of the kidneys.
Hepatorenal Syndrome), a life-threatening form of progressive kidney failure that occurs in
patients
Patients
Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures.
Clinician–Patient Relationship with advanced
liver
Liver
The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood.
Liver: Anatomy disease, such as
cirrhosis
Cirrhosis
Cirrhosis is a late stage of hepatic parenchymal necrosis and scarring (fibrosis) most commonly due to hepatitis C infection and alcoholic liver disease. Patients may present with jaundice, ascites, and hepatosplenomegaly. Cirrhosis can also cause complications such as hepatic encephalopathy, portal hypertension, portal vein thrombosis, and hepatorenal syndrome.
Cirrhosis with
ascites
Ascites
Ascites is the pathologic accumulation of fluid within the peritoneal cavity that occurs due to an osmotic and/or hydrostatic pressure imbalance secondary to portal hypertension (cirrhosis, heart failure) or non-portal hypertension (hypoalbuminemia, malignancy, infection).
Ascites.
| Coding System | Code | Description |
|---|---|---|
| ICD-10-CM | K76.7 | Hepatorenal syndrome Hepatorenal Syndrome Hepatorenal syndrome (HRS) is a potentially reversible cause of acute kidney injury that develops secondary to liver disease. The main cause of HRS is hypovolemia, often as a result of forced diuresis or drainage of ascites. This leads to renal vasoconstriction resulting in hypoperfusion of the kidneys. Hepatorenal Syndrome |
| SNOMED CT | 83584006 | Hepatorenal syndrome Hepatorenal Syndrome Hepatorenal syndrome (HRS) is a potentially reversible cause of acute kidney injury that develops secondary to liver disease. The main cause of HRS is hypovolemia, often as a result of forced diuresis or drainage of ascites. This leads to renal vasoconstriction resulting in hypoperfusion of the kidneys. Hepatorenal Syndrome (disorder) |
Medications:
These codes are for the vasoconstrictor medications
midodrine
Midodrine
An ethanolamine derivative that is an adrenergic alpha-1 agonist. It is used as a vasoconstrictor agent in the treatment of hypotension.
Sympathomimetic Drugs and
octreotide
Octreotide
A potent, long-acting synthetic somatostatin octapeptide analog that inhibits secretion of growth hormone and is used to treat hormone-secreting tumors; diabetes mellitus; hypotension, orthostatic; hyperinsulinism; hypergastrinemia; and small bowel fistula.
Antidiarrheal Drugs, which are administered along with
albumin
Albumin
Serum albumin from humans. It is an essential carrier of both endogenous substances, such as fatty acids and bilirubin, and of xenobiotics in the blood.
Liver Function Tests as the primary medical therapy for
HRS
HRS
Hepatorenal syndrome (HRS) is a potentially reversible cause of acute kidney injury that develops secondary to liver disease. The main cause of hrs is hypovolemia, often as a result of forced diuresis or drainage of ascites. This leads to renal vasoconstriction resulting in hypoperfusion of the kidneys.
Hepatorenal Syndrome to improve renal perfusion.
| Coding System | Code | Description |
|---|---|---|
| RxNorm | 19001 | Midodrine Midodrine An ethanolamine derivative that is an adrenergic alpha-1 agonist. It is used as a vasoconstrictor agent in the treatment of hypotension. Sympathomimetic Drugs (ingredient) |
| RxNorm | 7619 | Octreotide Octreotide A potent, long-acting synthetic somatostatin octapeptide analog that inhibits secretion of growth hormone and is used to treat hormone-secreting tumors; diabetes mellitus; hypotension, orthostatic; hyperinsulinism; hypergastrinemia; and small bowel fistula. Antidiarrheal Drugs (ingredient) |
| HCPCS | J0257 | Injection, albumin Albumin Serum albumin from humans. It is an essential carrier of both endogenous substances, such as fatty acids and bilirubin, and of xenobiotics in the blood. Liver Function Tests (human), 5%, 50 ml |