The complexity of health systems and the delivery of healthcare has resulted in the growing field of health systems science, which has now joined basic and clinical sciences as the 3rd pillar of medical education. Health systems science allows for an understanding of the framework in which care providers practice, and comprehension of the interconnected components of care delivery. Effective communication and collaboration within this context are essential for providing quality healthcare. The patient is at the center of a nested model of healthcare surrounded by the care team, the supporting organizational infrastructure, and the political environment. Models of health systems are defined by the ways in which healthcare is paid for, financed, and delivered. Healthcare delivery systems are further defined by a network of providers, affiliated organizations, and financial structures.
Last updated: Dec 15, 2025
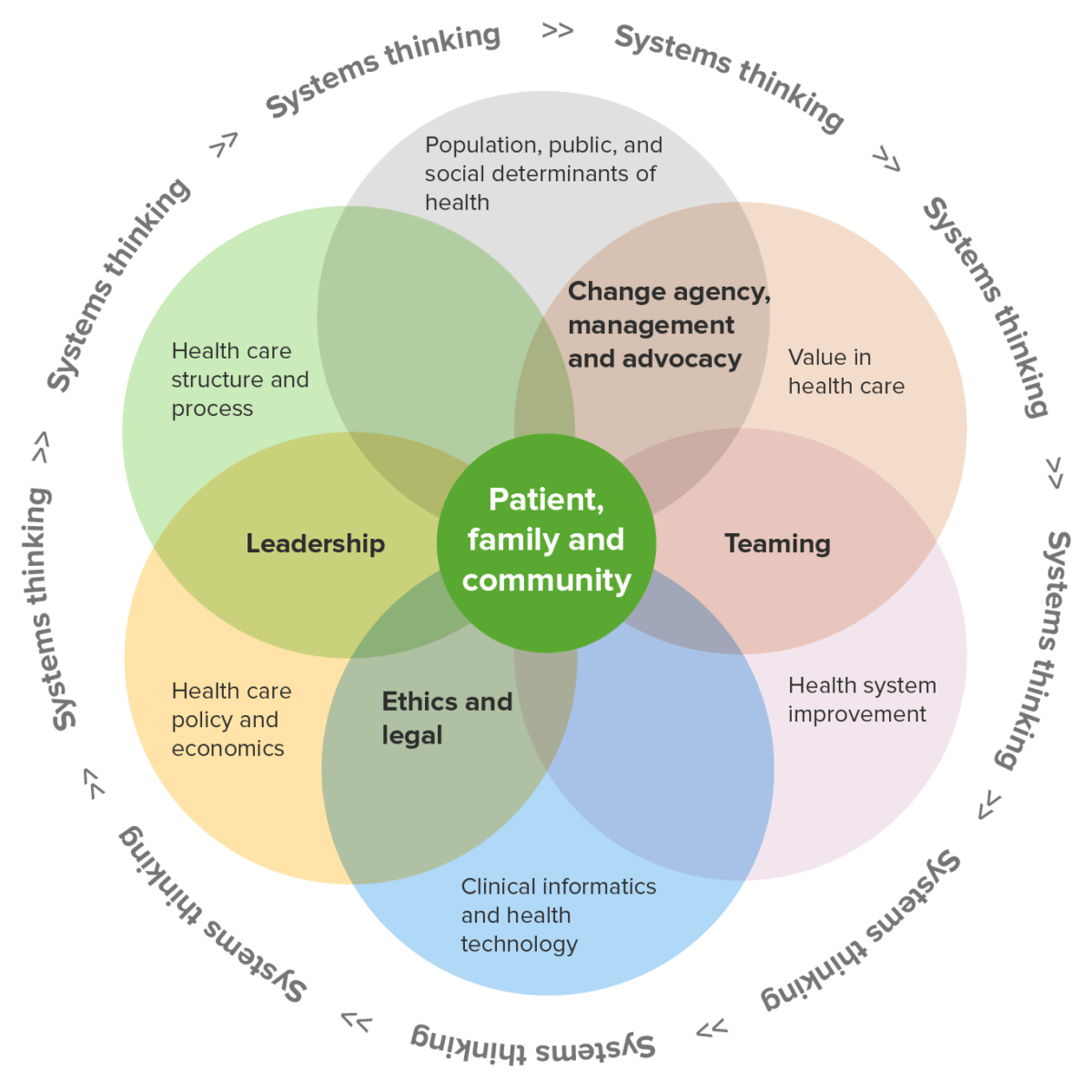
Health systems science domains
Image by Lecturio.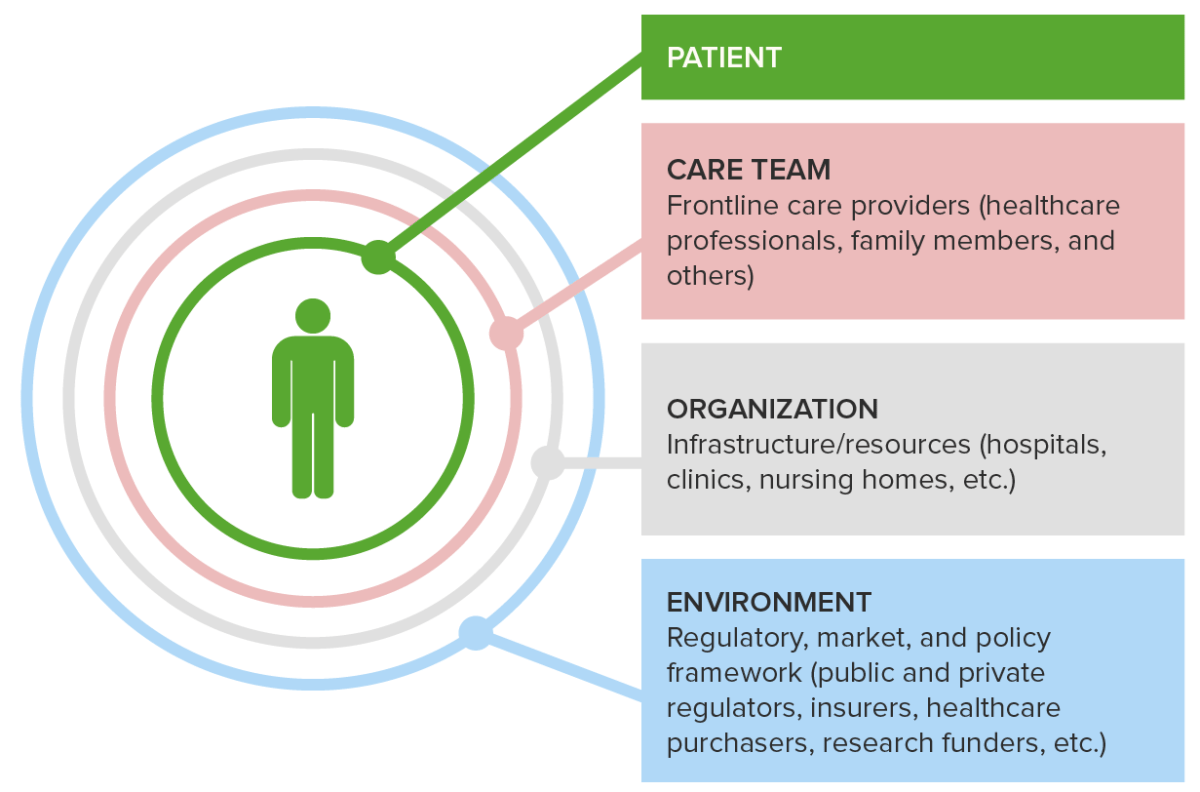
A 4-level conceptual health model
Image by Lecturio.