Graves' disease is an autoimmune disorder Autoimmune Disorder Septic Arthritis characterized by the presence of circulating thyroid-stimulating hormone Thyroid-stimulating hormone A glycoprotein hormone secreted by the adenohypophysis. Thyrotropin stimulates thyroid gland by increasing the iodide transport, synthesis and release of thyroid hormones (thyroxine and triiodothyronine). Thyroid Hormones (TSH) receptor Receptor Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors antibodies Antibodies Immunoglobulins (Igs), also known as antibodies, are glycoprotein molecules produced by plasma cells that act in immune responses by recognizing and binding particular antigens. The various Ig classes are IgG (the most abundant), IgM, IgE, IgD, and IgA, which differ in their biologic features, structure, target specificity, and distribution. Immunoglobulins: Types and Functions, which cause the thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy gland to hyperfunction. Clinical features include those of hyperthyroidism Hyperthyroidism Hypersecretion of thyroid hormones from the thyroid gland. Elevated levels of thyroid hormones increase basal metabolic rate. Thyrotoxicosis and Hyperthyroidism, as well as orbitopathy, goiter Goiter A goiter is a chronic enlargement of the thyroid gland due to nonneoplastic growth occurring in the setting of hypothyroidism, hyperthyroidism, or euthyroidism. Morphologically, thyroid enlargement can be diffuse (smooth consistency) or nodular (uninodular or multinodular). Goiter, and dermopathy/ pretibial myxedema Pretibial Myxedema Graves’ Disease. Diagnosis is by thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy laboratory tests showing a low TSH, elevated thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy hormones Hormones Hormones are messenger molecules that are synthesized in one part of the body and move through the bloodstream to exert specific regulatory effects on another part of the body. Hormones play critical roles in coordinating cellular activities throughout the body in response to the constant changes in both the internal and external environments. Hormones: Overview and Types ( thyroxine Thyroxine The major hormone derived from the thyroid gland. Thyroxine is synthesized via the iodination of tyrosines (monoiodotyrosine) and the coupling of iodotyrosines (diiodotyrosine) in the thyroglobulin. Thyroxine is released from thyroglobulin by proteolysis and secreted into the blood. Thyroid Hormones (T4) and triiodothyronine Triiodothyronine A T3 thyroid hormone normally synthesized and secreted by the thyroid gland in much smaller quantities than thyroxine (T4). Most T3 is derived from peripheral monodeiodination of T4 at the 5' position of the outer ring of the iodothyronine nucleus. The hormone finally delivered and used by the tissues is mainly t3. Thyroid Hormones (T3)) and thyrotropin-receptor antibodies Antibodies Immunoglobulins (Igs), also known as antibodies, are glycoprotein molecules produced by plasma cells that act in immune responses by recognizing and binding particular antigens. The various Ig classes are IgG (the most abundant), IgM, IgE, IgD, and IgA, which differ in their biologic features, structure, target specificity, and distribution. Immunoglobulins: Types and Functions (TRAbs; particularly the thyroid-stimulating immunoglobulins Thyroid-stimulating immunoglobulins Autoantibodies that bind to the thyroid-stimulating hormone (TSH) receptor on thyroid epithelial cells. The autoantibodies mimic TSH causing an unregulated production of thyroid hormones characteristic of graves disease. Graves’ Disease subtype). If initial tests are nondiagnostic, radioactive iodine uptake Radioactive Iodine Uptake Thyrotoxicosis and Hyperthyroidism (increased uptake) and thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy ultrasound (diffuse thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy enlargement) provide diagnostic information. Treatment options include antithyroid drugs, radioiodine ablation Radioiodine Ablation Thyrotoxicosis and Hyperthyroidism, and surgery.
Last updated: Dec 15, 2025
Graves’ disease is an autoimmune disorder Autoimmune Disorder Septic Arthritis in which antibodies Antibodies Immunoglobulins (Igs), also known as antibodies, are glycoprotein molecules produced by plasma cells that act in immune responses by recognizing and binding particular antigens. The various Ig classes are IgG (the most abundant), IgM, IgE, IgD, and IgA, which differ in their biologic features, structure, target specificity, and distribution. Immunoglobulins: Types and Functions against the thyroid-stimulating hormone Thyroid-stimulating hormone A glycoprotein hormone secreted by the adenohypophysis. Thyrotropin stimulates thyroid gland by increasing the iodide transport, synthesis and release of thyroid hormones (thyroxine and triiodothyronine). Thyroid Hormones (TSH) receptors Receptors Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors cause the thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy gland to hyperfunction. The syndrome may have the following features:
Susceptibility to Graves’ disease is considered to be a combination of multiple factors.
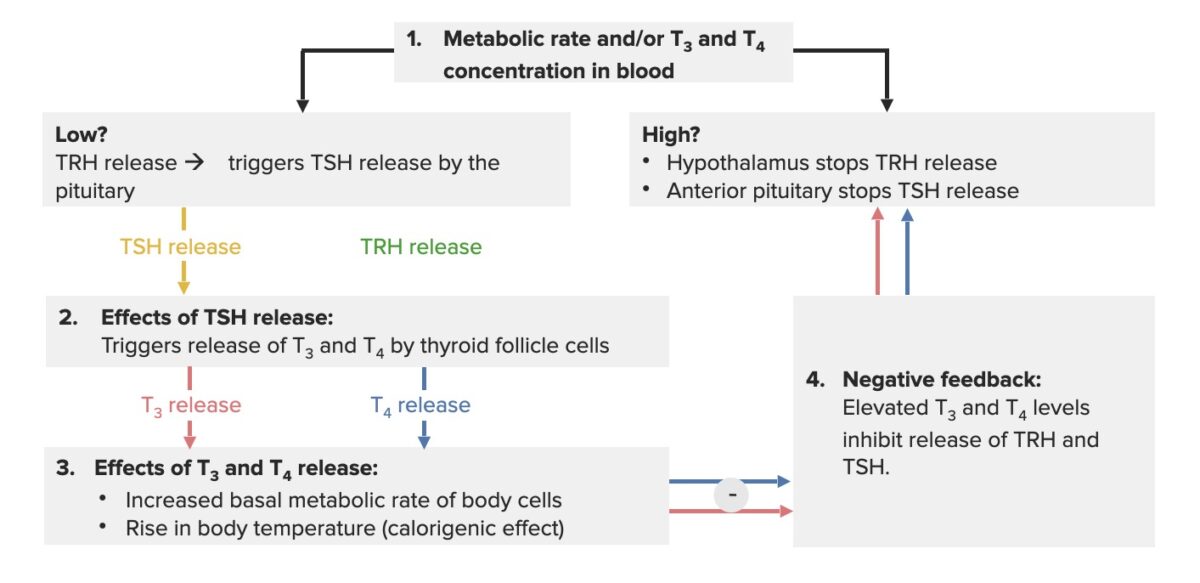
Hypothalamus-pituitary-thyroid axis feedback loop:
When the thyroid hormones are low, the hypothalamus releases thyrotropin-releasing hormone (TRH), which triggers the pituitary gland to secrete TSH. The effect of this process is that the thyroid gland produces thyroxine (T4) and triiodothyronine (T3) (more T4 is produced, as it gets converted to T3). The increase in thyroid hormones (free or unbound T3/T4) creates a negative feedback, inhibiting TRH and TSH release.
Elevated thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy hormone levels have effects throughout the body, including:
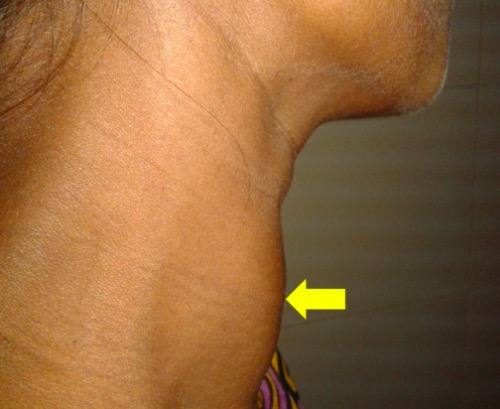
Goiter: diffusely enlarged thyroid gland (arrow) in a 30-year-old pregnant woman
Image: “Diffusely enlarged thyroid gland” by Department of Cardiology, Dhaka Medical College Hospital, Dhaka, Bangladesh. License: CC BY 4.0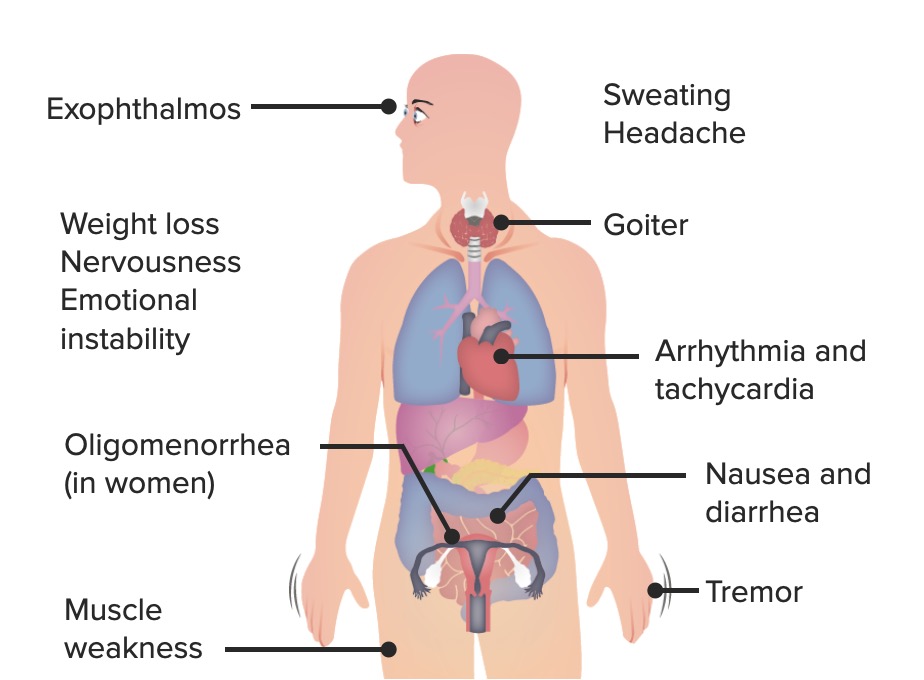
The most common signs and symptoms of Graves’ disease
Image by Lecturio.
Ophthalmologic effect of Graves’ disease: bilateral infiltrative thyroid-associated ophthalmopathy in a 33-year-old woman
Image: “Thyroid-associated ophthalmopathy” by Esra Şahlı and Kaan Gündüz. License: CC BY 2.5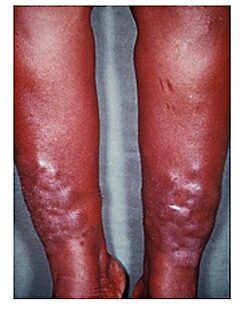
Myxedema
Image: “Myxedema” by Herbert L. Fred, MD and Hendrik A. van Dijk. License: CCC BY 2.0The diagnosis of Graves’ disease Graves’ disease A common form of hyperthyroidism with a diffuse hyperplastic goiter. It is an autoimmune disorder that produces antibodies against the thyroid stimulating hormone receptor. These autoantibodies activate the TSH receptor, thereby stimulating the thyroid gland and hypersecretion of thyroid hormones. These autoantibodies can also affect the eyes (Graves ophthalmopathy) and the skin (Graves dermopathy). Thyrotoxicosis and Hyperthyroidism is primarily made with lab testing combined with characteristic features on clinical presentation, though a radioactive iodine uptake Radioactive Iodine Uptake Thyrotoxicosis and Hyperthyroidism scan may be helpful in cases of diagnostic uncertainty.
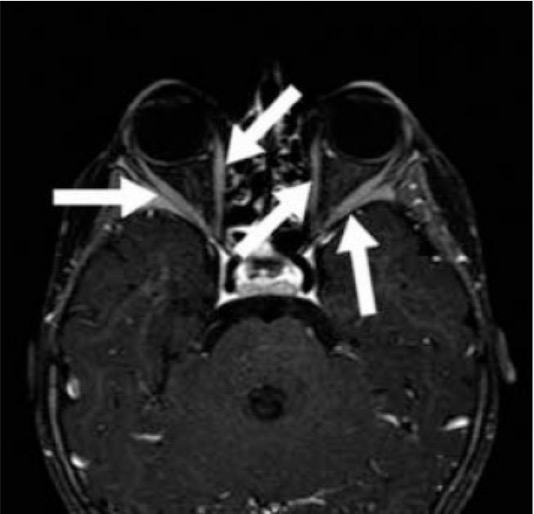
Graves’ orbitopathy: Contrast-enhanced axial MRI of a 2-year-old patient with Graves’ disease shows marked enhancement of extraocular muscles (arrows) of bilateral orbits.
Image: “T1 weighted fat saturated contrast enhanced axial MR” by Mustafa Kemal University School of Medicine, Department of Nuclear Medicine, Hatay, Turkey. License: CC BY 2.5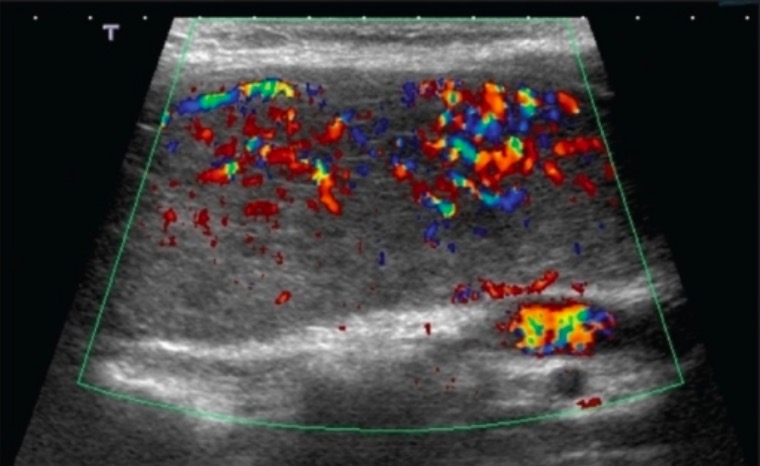
Thyroid ultrasonography with Doppler in Graves’ disease: a 28-year-old woman with Graves’ disease whose ultrasound with Doppler finding shows diffuse colour flow representing intense vascularity (“thyroid inferno”)
Image: “Ultrasound of the thyroid” by Saleh Aldasouqi et al. License: CC BY 2.0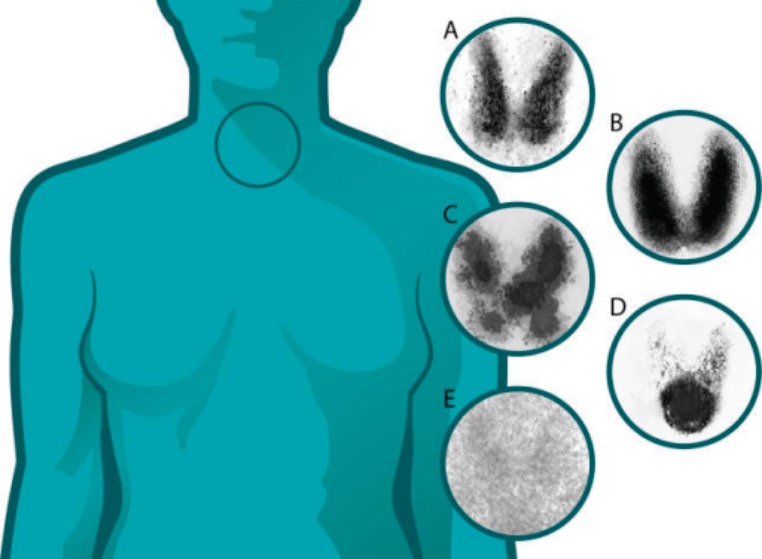
Thyroid uptake scans (thyroiditis versus other thyroid diseases):
A: normal
B: Graves’ disease: diffuse increased uptake in both thyroid lobes
C: toxic multinodular goiter: “hot” and “cold” areas of uneven uptake
D: toxic adenoma: increased uptake in a single nodule with suppression of the surrounding thyroid
E: thyroiditis: decreased or absent uptake
| Clinical situation | Antithyroid drugs | Radioiodine ablation Radioiodine Ablation Thyrotoxicosis and Hyperthyroidism | Surgery |
|---|---|---|---|
| Women planning pregnancy Pregnancy The status during which female mammals carry their developing young (embryos or fetuses) in utero before birth, beginning from fertilization to birth. Pregnancy: Diagnosis, Physiology, and Care in > 6 months | Acceptable | Preferred | Acceptable |
| Women planning pregnancy Pregnancy The status during which female mammals carry their developing young (embryos or fetuses) in utero before birth, beginning from fertilization to birth. Pregnancy: Diagnosis, Physiology, and Care in < 6 months | Preferred | X | Preferred |
| Currently pregnant | Preferred | X | Sometimes acceptable, best in 2nd trimester |
| Comorbidities Comorbidities The presence of co-existing or additional diseases with reference to an initial diagnosis or with reference to the index condition that is the subject of study. Comorbidity may affect the ability of affected individuals to function and also their survival; it may be used as a prognostic indicator for length of hospital stay, cost factors, and outcome or survival. St. Louis Encephalitis Virus increasing surgical risk (e.g., cardiovascular disease) and/or limited life expectancy | Acceptable | Preferred | X |
| Inactive orbitopathy | Acceptable | Acceptable | Acceptable |
| Moderate-to-severe orbitopathy | Preferred | X | Preferred |
| Liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy disease | Use with caution | Preferred | Acceptable |
| Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with a high likelihood of remission Remission A spontaneous diminution or abatement of a disease over time, without formal treatment. Cluster Headaches (e.g., mild disease with low TRAb titers) | Preferred | Acceptable | Acceptable |
| Suspected or confirmed thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy malignancy Malignancy Hemothorax | Sometimes acceptable | X | Preferred |
| ≥ 1 large thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy nodules | Acceptable | Sometimes acceptable | Preferred |
Mechanism and use:
Options:
Remission Remission A spontaneous diminution or abatement of a disease over time, without formal treatment. Cluster Headaches:[10,11]
Adverse effects:
Follow-up:[10]
Patient information:[10]
For hyperthyroidism Hyperthyroidism Hypersecretion of thyroid hormones from the thyroid gland. Elevated levels of thyroid hormones increase basal metabolic rate. Thyrotoxicosis and Hyperthyroidism and goiter Goiter A goiter is a chronic enlargement of the thyroid gland due to nonneoplastic growth occurring in the setting of hypothyroidism, hyperthyroidism, or euthyroidism. Morphologically, thyroid enlargement can be diffuse (smooth consistency) or nodular (uninodular or multinodular). Goiter:
For orbitopathy:
For dermopathy:
Additional recommendations:
Diagnosis Codes:
This code is used to diagnose Graves’ disease, an
autoimmune disorder
Autoimmune Disorder
Septic Arthritis that is the most common cause of
hyperthyroidism
Hyperthyroidism
Hypersecretion of thyroid hormones from the thyroid gland. Elevated levels of thyroid hormones increase basal metabolic rate.
Thyrotoxicosis and Hyperthyroidism, characterized by a diffusely enlarged
thyroid
Thyroid
The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck.
Thyroid Gland: Anatomy gland (
goiter
Goiter
A goiter is a chronic enlargement of the thyroid gland due to nonneoplastic growth occurring in the setting of hypothyroidism, hyperthyroidism, or euthyroidism. Morphologically, thyroid enlargement can be diffuse (smooth consistency) or nodular (uninodular or multinodular).
Goiter).
| Coding System | Code | Description |
|---|---|---|
| ICD-10-CM | E05.00 | Thyrotoxicosis Thyrotoxicosis A hypermetabolic syndrome caused by excess thyroid hormones which may come from endogenous or exogenous sources. The endogenous source of hormone may be thyroid hyperplasia; thyroid neoplasms; or hormone-producing extrathyroidal tissue. Thyrotoxicosis is characterized by nervousness; tachycardia; fatigue; weight loss; heat intolerance; and excessive sweating. Thyrotoxicosis and Hyperthyroidism with diffuse goiter Diffuse goiter Smooth and symmetrically enlarged thyroid gland. Goiter without thyrotoxic crisis or storm |
| SNOMED CT | 35264003 | Graves’ disease (disorder) |
Evaluation & Workup:
This code is for the Thyroid-Stimulating Immunoglobulin (
TSI
TSI
Shigella) or TSH-Receptor Antibody (TRAb) test, which is a specific blood test that confirms the autoimmune basis of the
hyperthyroidism
Hyperthyroidism
Hypersecretion of thyroid hormones from the thyroid gland. Elevated levels of thyroid hormones increase basal metabolic rate.
Thyrotoxicosis and Hyperthyroidism in Graves’ disease.
| Coding System | Code | Description |
|---|---|---|
| CPT | 84445 | Thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy stimulating immune globulins ( TSI TSI Shigella) |
Medications:
This code is for
methimazole
Methimazole
A thioureylene antithyroid agent that inhibits the formation of thyroid hormones by interfering with the incorporation of iodine into tyrosyl residues of thyroglobulin. This is done by interfering with the oxidation of iodide ion and iodotyrosyl groups through inhibition of the peroxidase enzyme.
Antithyroid Drugs, an antithyroid drug that blocks the production of
thyroid
Thyroid
The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck.
Thyroid Gland: Anatomy hormone and is the primary medical treatment for Graves’ disease.
| Coding System | Code | Description |
|---|---|---|
| RxNorm | 6847 | Methimazole Methimazole A thioureylene antithyroid agent that inhibits the formation of thyroid hormones by interfering with the incorporation of iodine into tyrosyl residues of thyroglobulin. This is done by interfering with the oxidation of iodide ion and iodotyrosyl groups through inhibition of the peroxidase enzyme. Antithyroid Drugs (ingredient) |