The primary functions of the GI tract are digestion Digestion Digestion refers to the process of the mechanical and chemical breakdown of food into smaller particles, which can then be absorbed and utilized by the body. Digestion and Absorption and absorption Absorption Absorption involves the uptake of nutrient molecules and their transfer from the lumen of the GI tract across the enterocytes and into the interstitial space, where they can be taken up in the venous or lymphatic circulation. Digestion and Absorption, which require coordinated contractions of the smooth muscles Smooth muscles Unstriated and unstriped muscle, one of the muscles of the internal organs, blood vessels, hair follicles, etc. Contractile elements are elongated, usually spindle-shaped cells with centrally located nuclei. Smooth muscle fibers are bound together into sheets or bundles by reticular fibers and frequently elastic nets are also abundant. Muscle Tissue: Histology present in the GI tract. Peristaltic waves, segmentation contractions, and the migrating motor Motor Neurons which send impulses peripherally to activate muscles or secretory cells. Nervous System: Histology complex are all important contraction patterns that help to mix contents, get them in contact with the intestinal walls (where they are further digested by brush-border enzymes Enzymes Enzymes are complex protein biocatalysts that accelerate chemical reactions without being consumed by them. Due to the body's constant metabolic needs, the absence of enzymes would make life unsustainable, as reactions would occur too slowly without these molecules. Basics of Enzymes and absorbed into the enterocytes), and propel material down the tract at appropriate times and in appropriate amounts.
Last updated: Dec 15, 2025
GI motility refers to the contraction of smooth muscle within the walls of the GI tract, which:
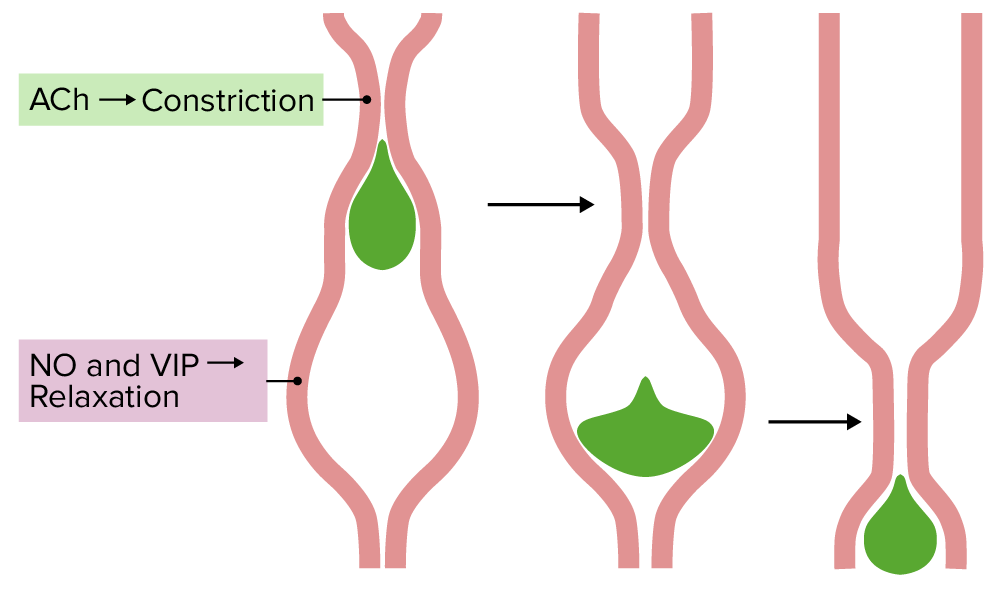
Coordination of smooth muscle in peristalsis:
Acetylcholine (ACh) causes constriction of the muscle just behind the foodstuff, while NO and vasoactive intestinal peptide (VIP) cause relaxation ahead of it. This creates a pressure gradient, forcing the food downward. Nerves from the enteric nervous system (with input from the autonomic nervous system), coordinate the wave of constriction and relaxation.
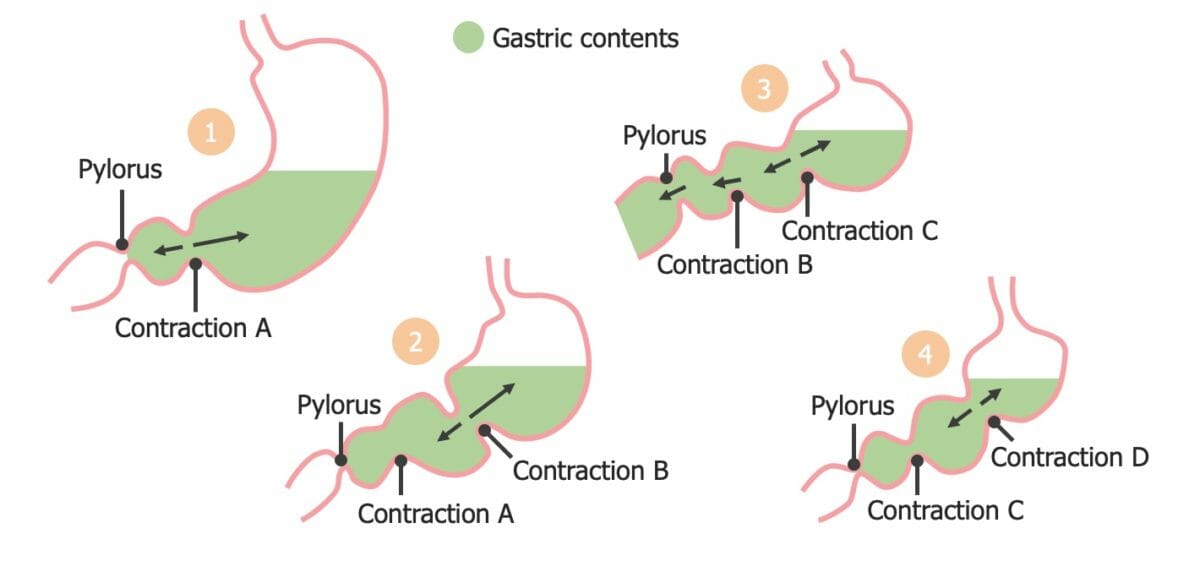
Segmentation contractions in the stomach:
Note how the subsequent contraction achieves mixing of contents and enough increase in pressure to overcome the relaxed pyloric sphincter.
GI motility is controlled primarily via the parasympathetic nervous system Nervous system The nervous system is a small and complex system that consists of an intricate network of neural cells (or neurons) and even more glial cells (for support and insulation). It is divided according to its anatomical components as well as its functional characteristics. The brain and spinal cord are referred to as the central nervous system, and the branches of nerves from these structures are referred to as the peripheral nervous system. Nervous System: Anatomy, Structure, and Classification (PNS) and the ENS.
A specialized portion of the ANS ANS The ans is a component of the peripheral nervous system that uses both afferent (sensory) and efferent (effector) neurons, which control the functioning of the internal organs and involuntary processes via connections with the CNS. The ans consists of the sympathetic and parasympathetic nervous systems. Autonomic Nervous System: Anatomy located within the walls of the GI tract
Consists of:
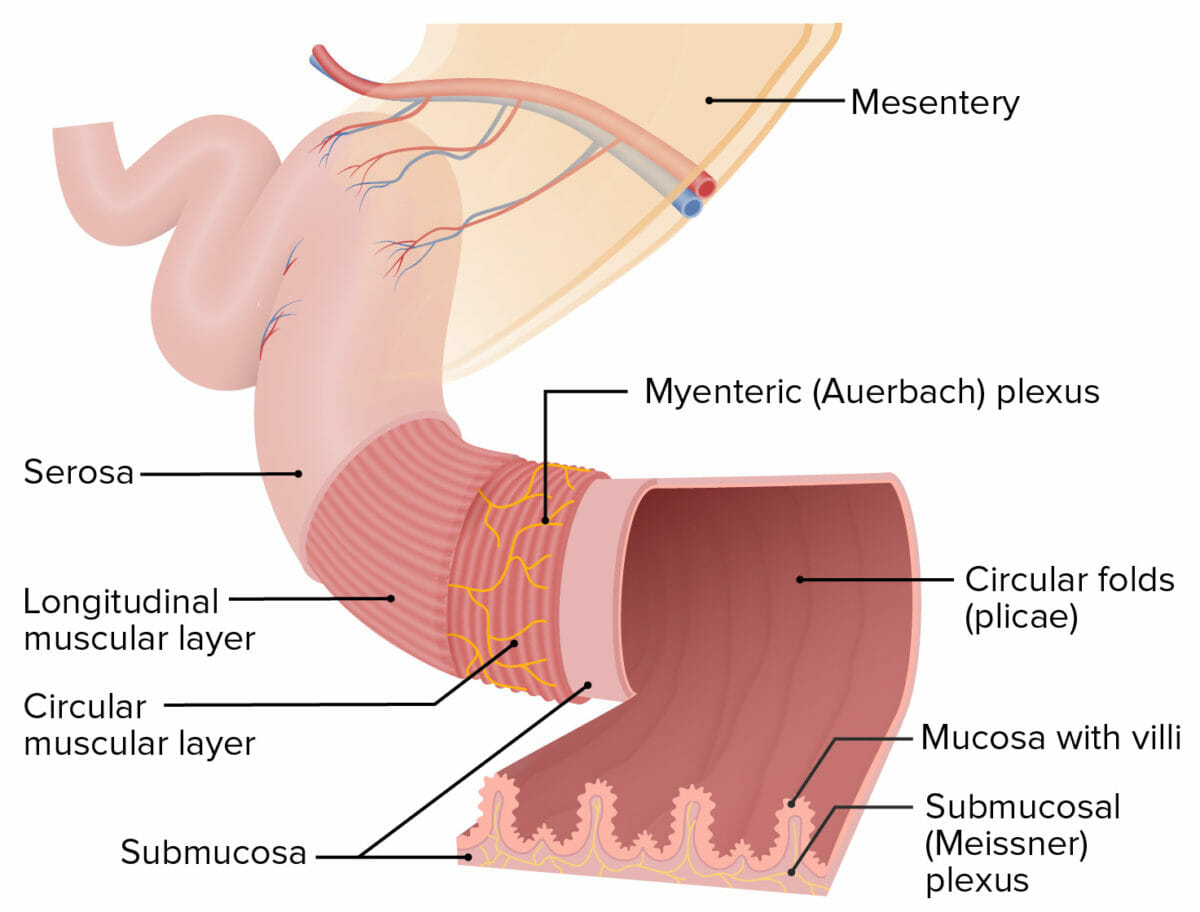
Structure of the intestinal walls:
The Meissner plexus is located within the submucosa, and the Auerbach plexus (also known as the myenteric plexus) is located between the circular and longitudinal muscular layers.
Function: local control of GI function
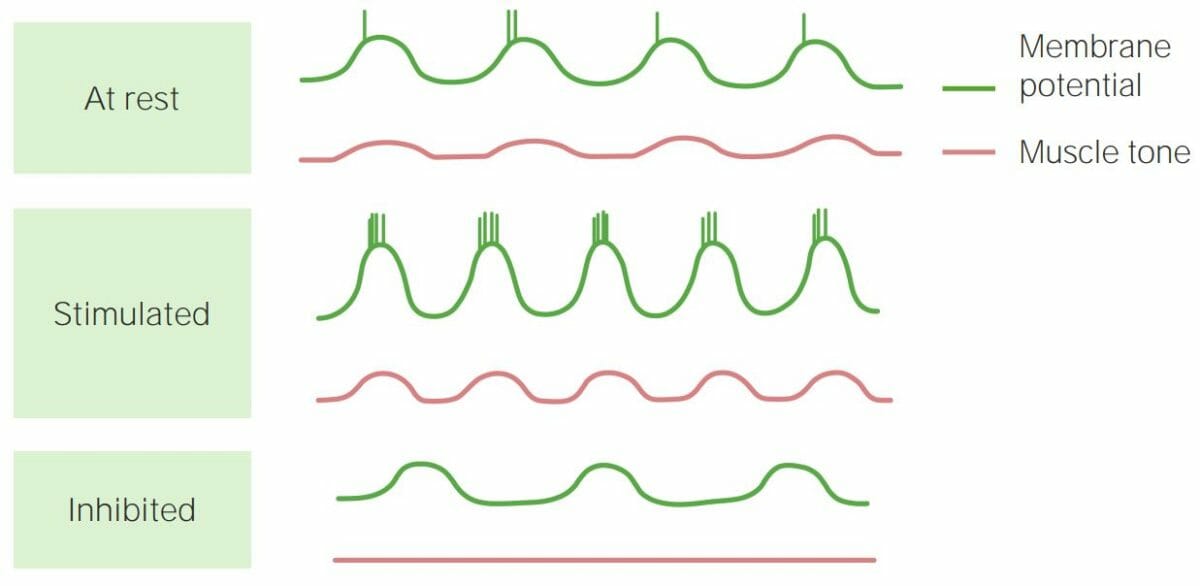
Schematic depiction of slow electrical waves and how they affect smooth muscle tone:
If the peak of the wave reaches the threshold required for an action potential (seen as a vertical spike in the membrane potential), muscle contraction occurs. When action potentials occur back to back in smooth muscle (Stimulated panel), contractions are stronger. If threshold is not reached (Inhibited panel), contractions do not occur.
Swallowing (also called deglutition) is a complex process involving > 22 muscles in the mouth, pharynx Pharynx The pharynx is a component of the digestive system that lies posterior to the nasal cavity, oral cavity, and larynx. The pharynx can be divided into the oropharynx, nasopharynx, and laryngopharynx. Pharyngeal muscles play an integral role in vital processes such as breathing, swallowing, and speaking. Pharynx: Anatomy, and esophagus Esophagus The esophagus is a muscular tube-shaped organ of around 25 centimeters in length that connects the pharynx to the stomach. The organ extends from approximately the 6th cervical vertebra to the 11th thoracic vertebra and can be divided grossly into 3 parts: the cervical part, the thoracic part, and the abdominal part. Esophagus: Anatomy, which moves food in the mouth through the upper esophageal sphincter Upper esophageal sphincter The structure at the pharyngoesophageal junction consisting chiefly of the cricopharyngeus muscle. It normally occludes the lumen of the esophagus, except during swallowing. Esophagus: Anatomy and into the esophagus Esophagus The esophagus is a muscular tube-shaped organ of around 25 centimeters in length that connects the pharynx to the stomach. The organ extends from approximately the 6th cervical vertebra to the 11th thoracic vertebra and can be divided grossly into 3 parts: the cervical part, the thoracic part, and the abdominal part. Esophagus: Anatomy.
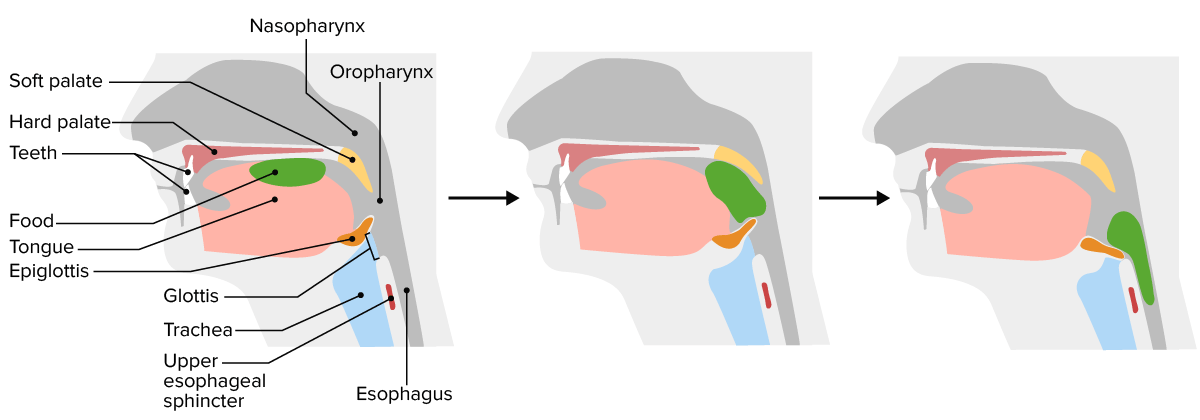
Swallowing:
First, the tongue compresses the food against the hard palate (note the glottis is open). Next, the tongue forces the bolus to the back of the mouth; the soft palate closes off the nasopharynx. Finally, as the foodstuff is forced downwards, the epiglottis is pulled forwards, closing the glottis (airway), and the upper esophageal sphincter relaxes, letting food into the esophagus. Peristaltic waves move the food down towards the stomach.
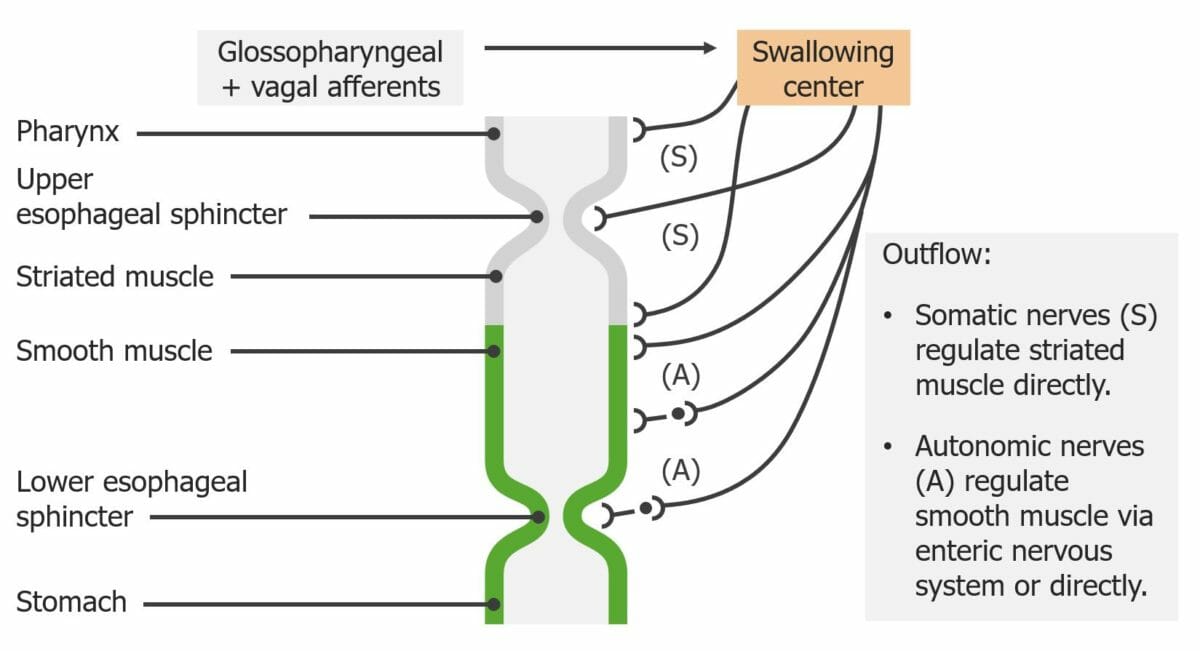
Innervation of the esophagus:
Note how the swallowing center integrates striated and smooth muscle activity.
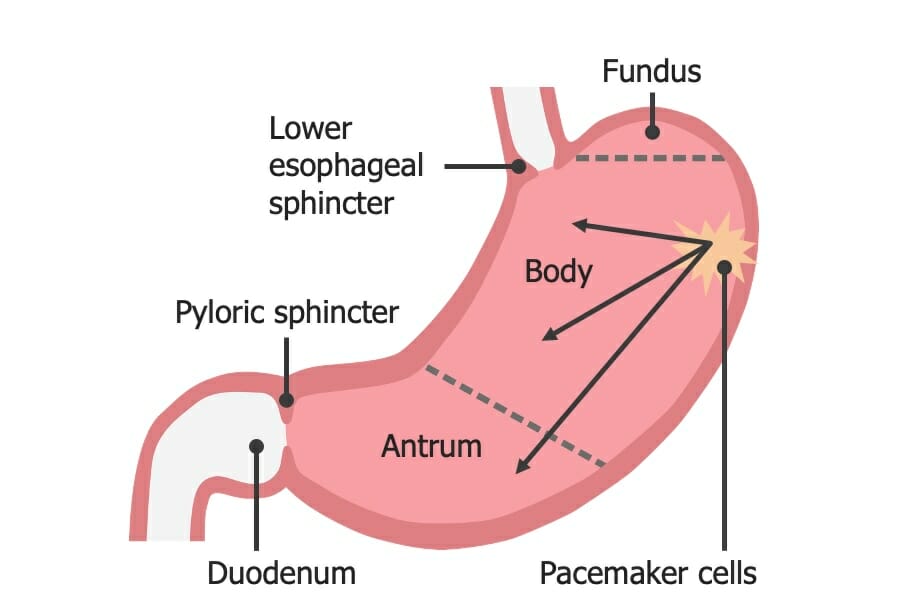
Regions of the stomach and their functions:
In the body of the stomach, the interstitial cells of Cajal are the pacemaker cells triggering regular peristaltic movements.
Mixes chyme Chyme Small Intestine: Anatomy:
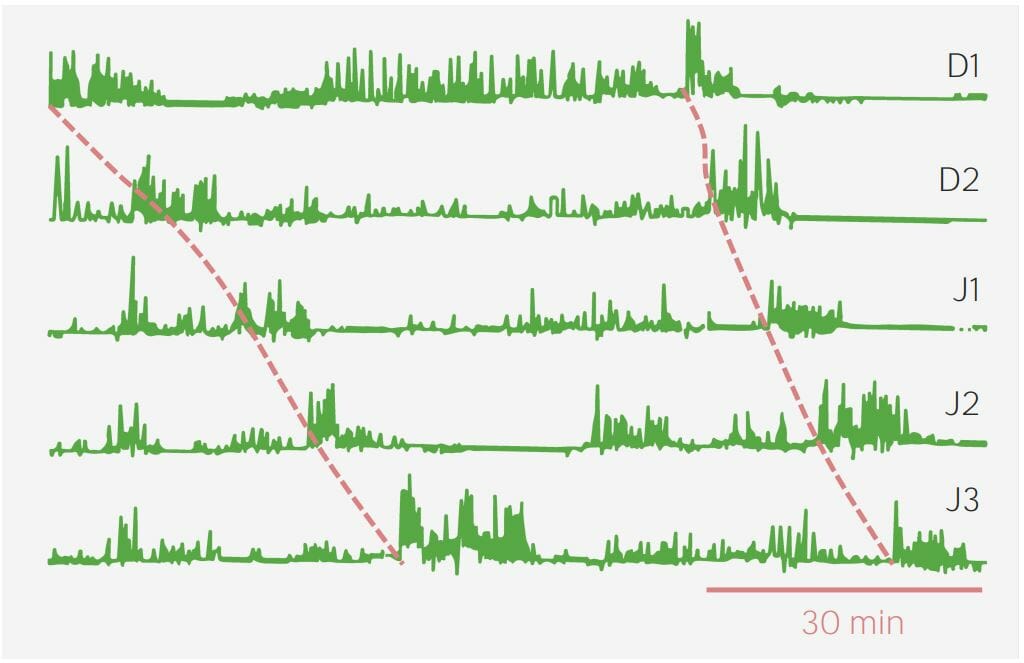
A graph showing the waves of the migrating motor complex during fasting:
The red dotted line shows the phase 3 waves.
The rectum Rectum The rectum and anal canal are the most terminal parts of the lower GI tract/large intestine that form a functional unit and control defecation. Fecal continence is maintained by several important anatomic structures including rectal folds, anal valves, the sling-like puborectalis muscle, and internal and external anal sphincters. Rectum and Anal Canal: Anatomy contains stretch receptors Receptors Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors that stimulate the defecation reflex when the rectum Rectum The rectum and anal canal are the most terminal parts of the lower GI tract/large intestine that form a functional unit and control defecation. Fecal continence is maintained by several important anatomic structures including rectal folds, anal valves, the sling-like puborectalis muscle, and internal and external anal sphincters. Rectum and Anal Canal: Anatomy begins to fill with feces.
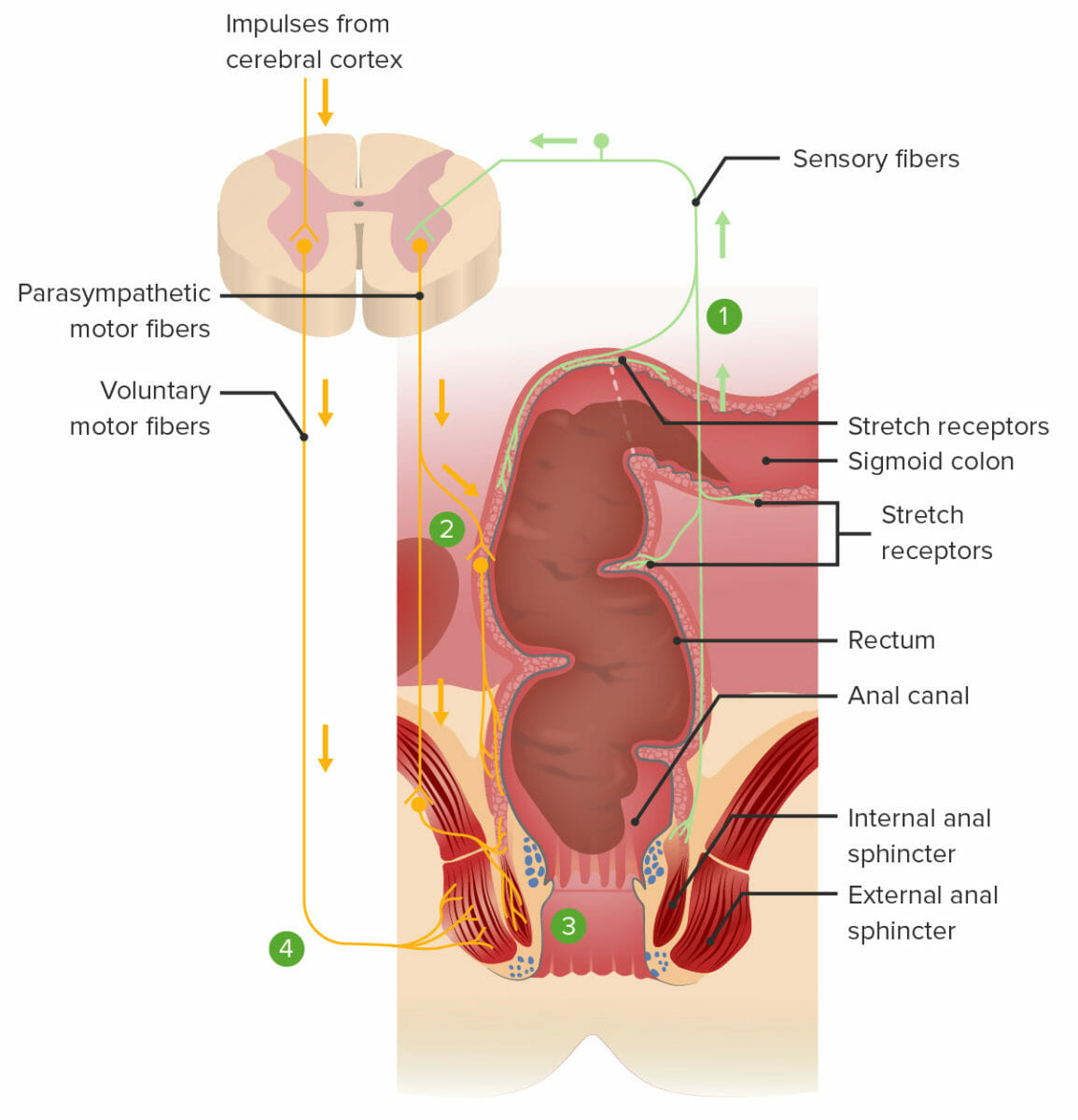
The defecation reflex:
1. Feces stretch the rectum and stimulate the stretch receptors, transmitting the signal to the spinal cord.
2. A spinal reflex sends parasympathetic motor signals to the myenteric nerve plexus, resulting in contraction of the smooth muscles within the rectum and pushing feces downward.
3. The same spinal reflex also sends parasympathetic motor signals to relax the internal anal sphincter.
4. Voluntary impulses from the brain prevent defecation by keeping the external anal sphincter contracted. Defecation will occur if voluntary signals allow the external anal sphincter to relax.