The end of a patient’s life has been a difficult, complex, and often controversial aspect of medicine, because, historically, death has been conceptualized as a “failure” on the physician’s part. As our understanding of death has evolved, so has the physician's relationship to it, becoming a companion to the patient in their final moments. Moreover, experienced doctors understand that during the last days of a person’s life, the focus must be on maximizing quality Quality Activities and programs intended to assure or improve the quality of care in either a defined medical setting or a program. The concept includes the assessment or evaluation of the quality of care; identification of problems or shortcomings in the delivery of care; designing activities to overcome these deficiencies; and follow-up monitoring to ensure effectiveness of corrective steps. Quality Measurement and Improvement of life rather than on prolonging it.
Last updated: Dec 15, 2025
The primary purpose of any medical intervention is to prolong life or to improve quality Quality Activities and programs intended to assure or improve the quality of care in either a defined medical setting or a program. The concept includes the assessment or evaluation of the quality of care; identification of problems or shortcomings in the delivery of care; designing activities to overcome these deficiencies; and follow-up monitoring to ensure effectiveness of corrective steps. Quality Measurement and Improvement of life (QOL). At the end of life, preserving a patient’s QOL is more important than prolonging life.
The key principles of medical ethics Ethics Medical ethics are a set of moral values that guide the decision-making of health care professionals in their daily practice. A sense of ethical responsibility has accompanied the profession of medicine since antiquity, and the Hippocratic oath was the 1st document to codify its core ethical principles. Medical Ethics: Basic Principles that apply to end-of-life issues include:
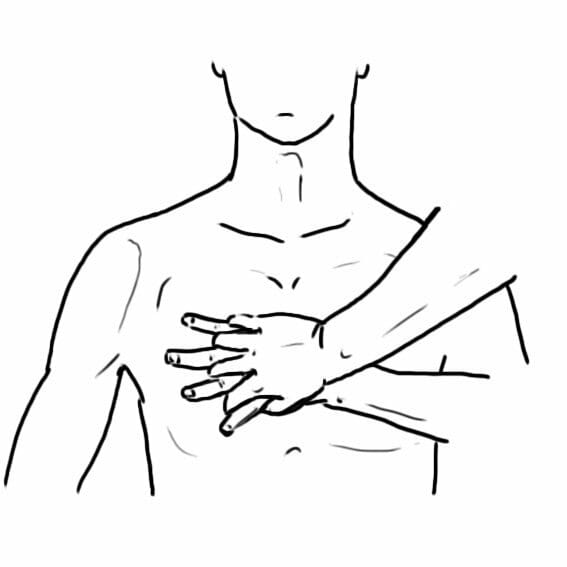
Technique of providing CPR
Image: “Chest-compression-hand-placement” by Another-anon-artist-234. License: CC0 1.0Despite being supported by the medical ethical principle of patient autonomy Autonomy Respect for the patient’s right to self-rule. Medical Ethics: Basic Principles, there is significant controversy surrounding PAD and euthanasia.
Principles involved in organ donation Organ Donation Brain Death include:
Generally, there are 2 types of organ donation Organ Donation Brain Death:
The circumstance of organ retrieval for DCDD are described according to the Maastricht classification:
| Category | Type | Circumstances | Typical location |
|---|---|---|---|
| I | Uncontrolled | Dead on arrival | ED |
| II | Uncontrolled | Unsuccessful resuscitation Resuscitation The restoration to life or consciousness of one apparently dead. . Neonatal Respiratory Distress Syndrome | ED |
| III | Controlled | Cardiac arrest Cardiac arrest Cardiac arrest is the sudden, complete cessation of cardiac output with hemodynamic collapse. Patients present as pulseless, unresponsive, and apneic. Rhythms associated with cardiac arrest are ventricular fibrillation/tachycardia, asystole, or pulseless electrical activity. Cardiac Arrest follows planned withdrawal of life-sustaining treatments | ICU ICU Hospital units providing continuous surveillance and care to acutely ill patients. West Nile Virus |
| IV | Either | Cardiac arrest Cardiac arrest Cardiac arrest is the sudden, complete cessation of cardiac output with hemodynamic collapse. Patients present as pulseless, unresponsive, and apneic. Rhythms associated with cardiac arrest are ventricular fibrillation/tachycardia, asystole, or pulseless electrical activity. Cardiac Arrest in a patient who is brain-dead | ICU ICU Hospital units providing continuous surveillance and care to acutely ill patients. West Nile Virus |