Diverticula are protrusions of the bowel wall occurring most commonly in the colon Colon The large intestines constitute the last portion of the digestive system. The large intestine consists of the cecum, appendix, colon (with ascending, transverse, descending, and sigmoid segments), rectum, and anal canal. The primary function of the colon is to remove water and compact the stool prior to expulsion from the body via the rectum and anal canal. Colon, Cecum, and Appendix: Anatomy. The condition of having diverticula (called diverticulosis) is mostly asymptomatic. These diverticula can become symptomatic, however, when associated with diseases. Diverticulitis is the inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body's defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation of diverticula, often presenting with lower abdominal pain Abdominal Pain Acute Abdomen and changes in bowel habits. The condition may be further complicated by abscess Abscess Accumulation of purulent material in tissues, organs, or circumscribed spaces, usually associated with signs of infection. Chronic Granulomatous Disease, perforation Perforation A pathological hole in an organ, blood vessel or other soft part of the body, occurring in the absence of external force. Esophagitis, fistula Fistula Abnormal communication most commonly seen between two internal organs, or between an internal organ and the surface of the body. Anal Fistula, and bowel obstruction Bowel obstruction Any impairment, arrest, or reversal of the normal flow of intestinal contents toward the anal canal. Ascaris/Ascariasis. Management consists of antibiotics, fluid resuscitation Resuscitation The restoration to life or consciousness of one apparently dead. . Neonatal Respiratory Distress Syndrome, and bowel rest. Surgery is required for complications, failure of medical management, and recurrent disease. In most cases of diverticular bleeding, spontaneous cessation occurs. Invasive intervention will be needed for persistent or recurrent bleeding.
Last updated: Dec 15, 2025
Diverticulosis is the presence of multiple diverticula, which are sac-like protrusions of the bowel wall.
Diverticular disease is diverticulosis with associated symptoms.

Diverticulosis: image showing the large bowel (sigmoid colon) with multiple diverticula
Image: “Large bowel (sigmoid colon)” by Haymanj. License: Public Domain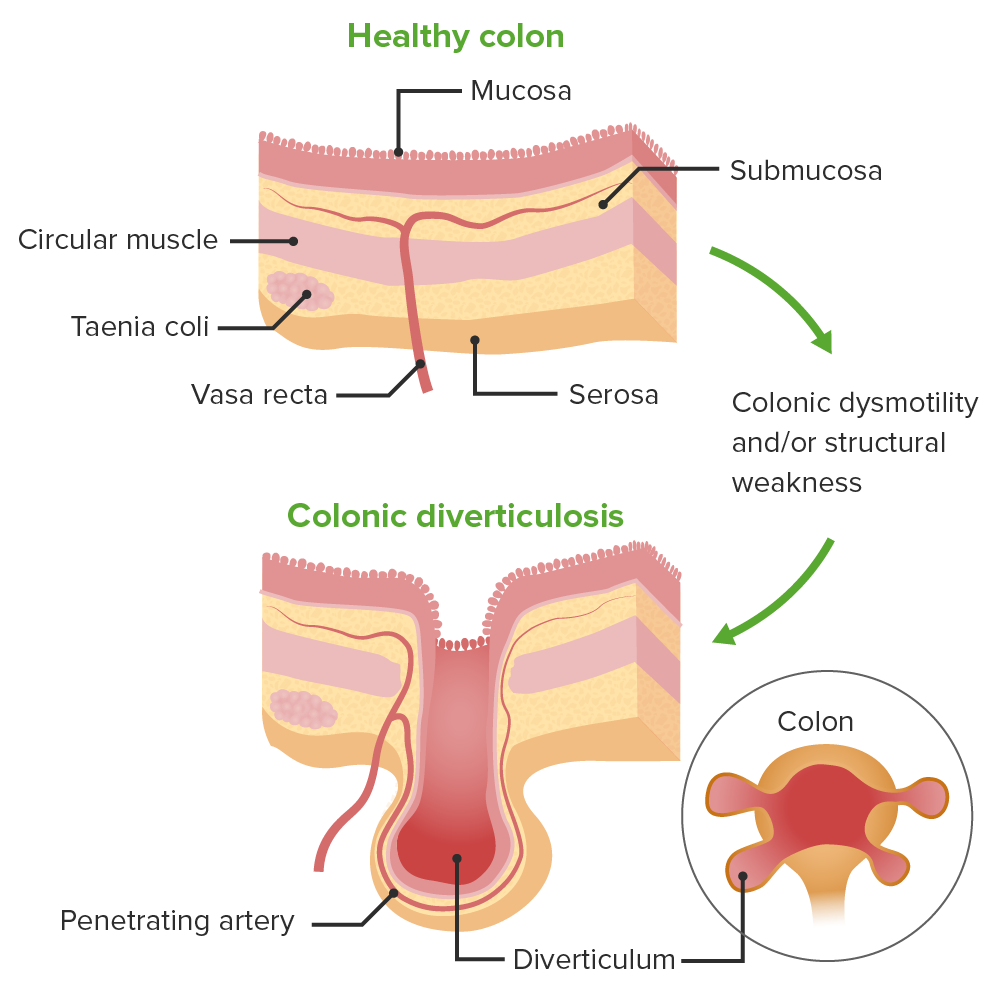
Pathophysiology of the development of diverticulosis from a healthy colon.
Colonic diverticula form when mucosa and submucosa herniate through the envelope that surrounds the intramural vasa recta (nutrient vessels).
Diverticulitis is often mild, with mesentery Mesentery A layer of the peritoneum which attaches the abdominal viscera to the abdominal wall and conveys their blood vessels and nerves. Peritoneum: Anatomy and pericolic fat walling off a small perforation Perforation A pathological hole in an organ, blood vessel or other soft part of the body, occurring in the absence of external force. Esophagitis. More extensive disease can lead to complications.
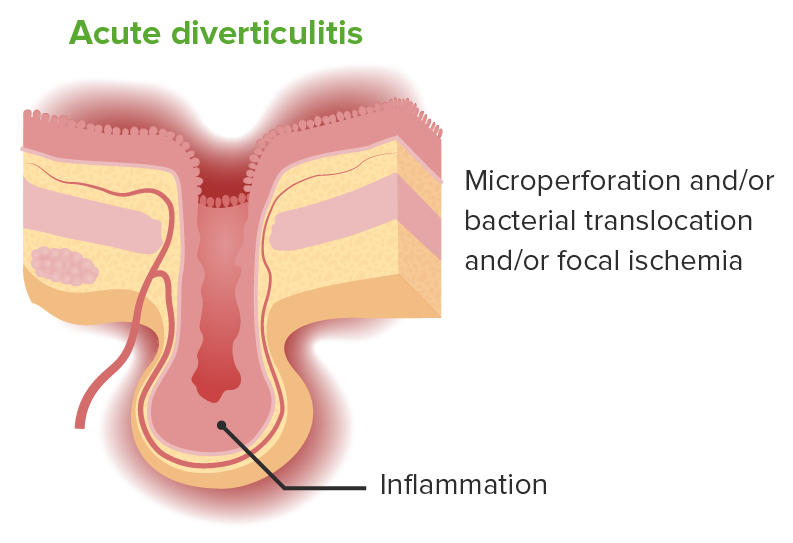
Pathophysiology of diverticulitis.
Acute diverticulitis is inflammation localized to a diverticulum and the surrounding mucosa. The process may include microperforation or bacterial translocation, or focal ischemia.
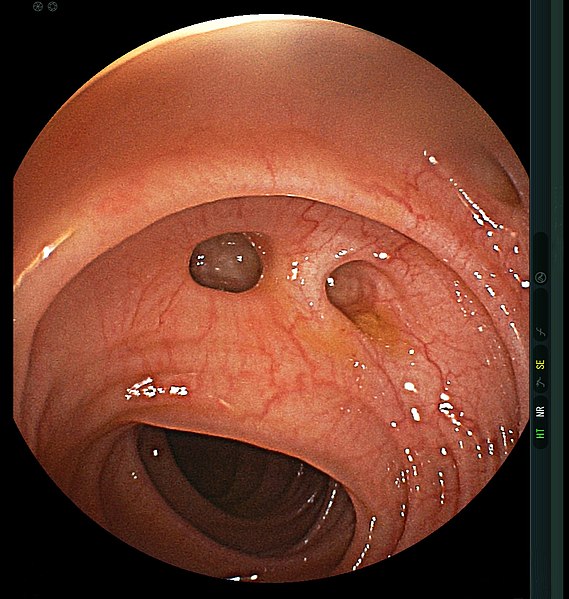
Diverticulosis: colonoscopy showing diverticula in the colon
Image: “Diverticulum” by MAC 06. License: CC BY 4.0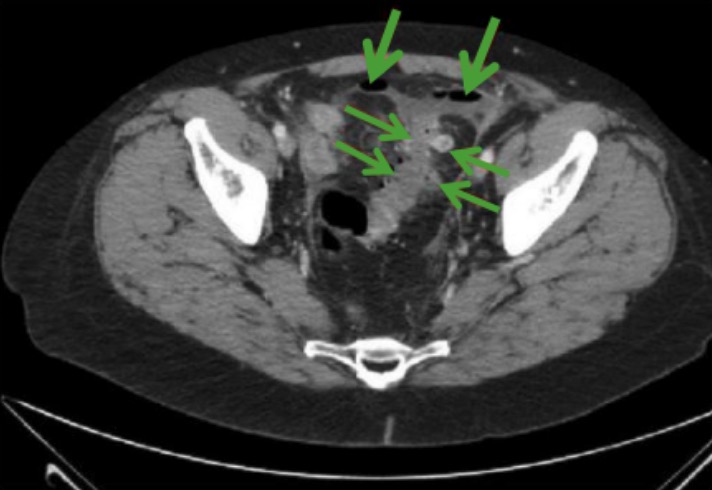
Imaging illustrating diverticulitis:
CT scan showing perforated diverticulitis (horizontal arrows) and free abdominal air (vertical arrows)
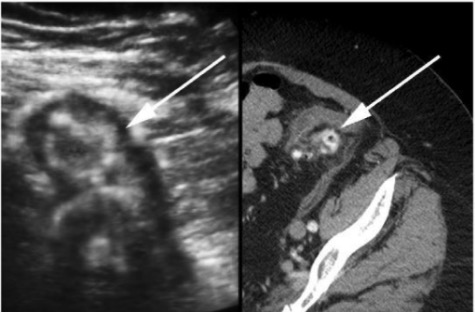
Ultrasound and CT scan images of diverticulitis:
Transabdominal sonographic view of the patient’s abdomen (left) and associated axial CT (right) revealing inflamed diverticula (arrow).
Related imaging findings of diverticulitis such as edematous diverticula with thickened hypoechoic walls and hyperechoic centers, and surrounding hyperechoic zones representing inflamed fat.
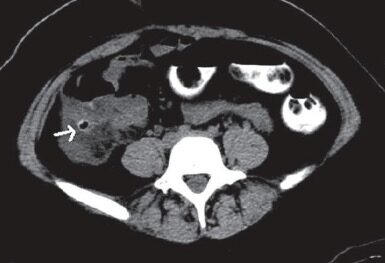
Imaging illustrating diverticulitis: CT scan with oral contrast shows an inflamed right-sided cecal diverticulum (arrow).
Image: “Cecal diverticulitis” by Monika Sharma and Anjali Agrawal. License: CC BY 2.0| Hinchey 1a | Phlegmon (localized) |
|---|---|
| Hinchey 1b | Pericolonic/mesenteric abscess Abscess Accumulation of purulent material in tissues, organs, or circumscribed spaces, usually associated with signs of infection. Chronic Granulomatous Disease |
| Hinchey 2 | Pelvic abscess Abscess Accumulation of purulent material in tissues, organs, or circumscribed spaces, usually associated with signs of infection. Chronic Granulomatous Disease |
| Hinchey 3 | Generalized purulent peritonitis Peritonitis Inflammation of the peritoneum lining the abdominal cavity as the result of infectious, autoimmune, or chemical processes. Primary peritonitis is due to infection of the peritoneal cavity via hematogenous or lymphatic spread and without intra-abdominal source. Secondary peritonitis arises from the abdominal cavity itself through rupture or abscess of intra-abdominal organs. Penetrating Abdominal Injury |
| Hinchey 4 | Generalized feculent peritonitis Peritonitis Inflammation of the peritoneum lining the abdominal cavity as the result of infectious, autoimmune, or chemical processes. Primary peritonitis is due to infection of the peritoneal cavity via hematogenous or lymphatic spread and without intra-abdominal source. Secondary peritonitis arises from the abdominal cavity itself through rupture or abscess of intra-abdominal organs. Penetrating Abdominal Injury |
Rationale:
Procedures:
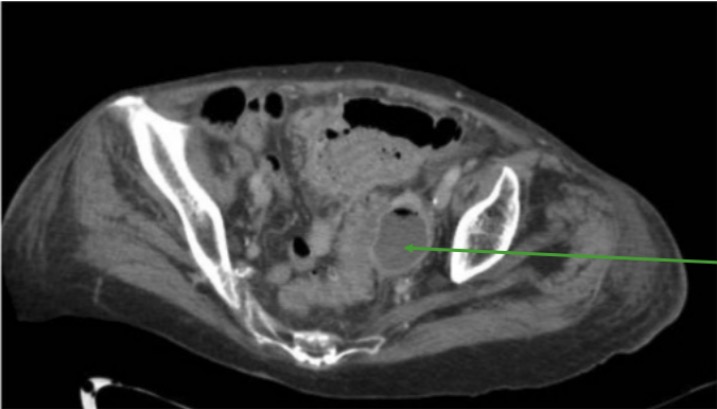
Imaging illustrating a sigmoid diverticulitis-related abscess: CT scan showing peri-colonic fluid collection with air-fluid level (green arrow) consistent with an abscess
Image: “Sigmoid diverticulitis” by Department of Surgery, Macerata Hospital, Macerata, Italy. License: CC BY 4.0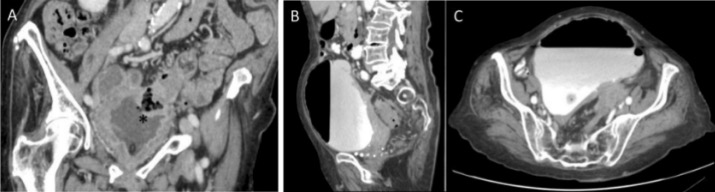
Colovesical fistula:
A: thickening of the wall of the bowel and bladder (black asterisk)
B and C: collection of contrast and air into the bladder

Diverticulitis fistulizing to the umbilicus: the inflamed and macerated umbilicus and periumbilical skin with fecal material in the umbilical pit
Image: “Diverticulitis fistulizing to the umbilicus” by Second Department of Surgery, Democritus University of Thrace, Medical School, 68 100 Alexandroupolis, Greece. License: CC BY 3.0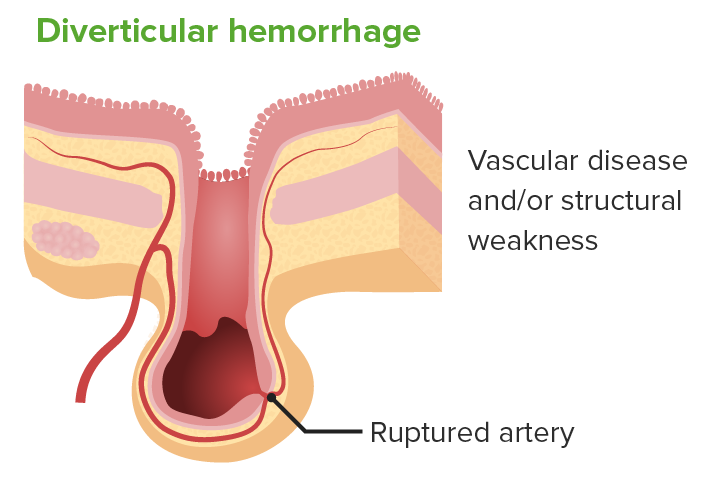
Illustration of diverticular hemorrhage:
Arterial bleeding can complicate diverticulosis, with vascular disease or structural weakness as likely contributing factors. The condtion is the most common source of lower gastrointestinal bleeding.
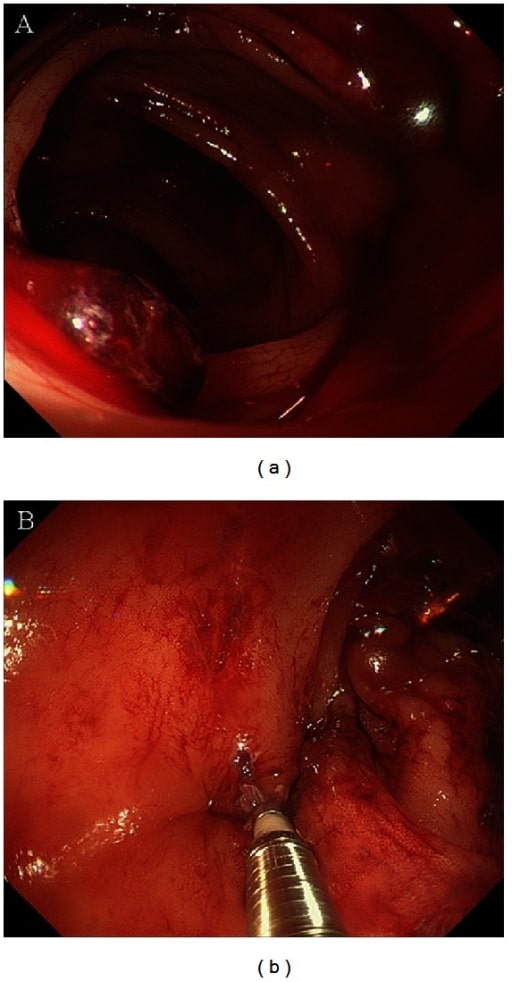
Diverticular bleeding:
(a) colonoscopy view of diverticular bleeding in the hepatic flexure
(b) endoscopic treatment using hemoclips