Diarrheagenic Escherichia coli (E. coli) species are a diverse group of pathogens classified into 5 major pathotypes that can cause intestinal infection and diarrhea. Transmission occurs primarily via consuming contaminated food or water, contact with infected people or animals, and swimming in untreated water. Pathogenesis varies based on the strain, but it can include toxin production, invasion of the mucosal surface, and adhesion with alteration of enterocyte structure. Noninvasive disease tends to present with watery diarrhea, while invasive infections cause bloody diarrhea. The diagnosis can be established with PCR. Management generally consists of supportive therapy (fluids and electrolytes). Antibiotics are reserved for severe or persistent infections and are contraindicated with enterohemorrhagic E. coli because of the risk of hemolytic uremic syndrome.
Last updated: Dec 15, 2025
Scanning electron microscope image of enterotoxigenic Escherichia coli
Image: “Under an extremely high magnification of 44, 818X, twice that of PHIL 10574 and 10575, this scanning electron microscopic (SEM) image revealed some of the morphologic details displayed by a single Gram-negative, rod-shaped, Escherichia coli bacterium.” by Janice Haney Carr. License: Public DomainDiarrheagenic strains of E. coli can be classified into 5 key “pathotypes,” each of which has unique virulence factors Virulence factors Those components of an organism that determine its capacity to cause disease but are not required for its viability per se. Two classes have been characterized: toxins, biological and surface adhesion molecules that affect the ability of the microorganism to invade and colonize a host. Haemophilus and pathologic mechanisms.
Virulence Virulence The degree of pathogenicity within a group or species of microorganisms or viruses as indicated by case fatality rates and/or the ability of the organism to invade the tissues of the host. The pathogenic capacity of an organism is determined by its virulence factors. Proteus traits are distinct for each category of pathogenic E. coli:
Each of the 5 main pathotypes has unique pathologic mechanisms.
Enterotoxigenic E. coli is a noninvasive pathogen. It uses fimbrial adhesins Adhesins Cell-surface components or appendages of bacteria that facilitate adhesion (bacterial adhesion) to other cells or to inanimate surfaces. Most fimbriae of gram-negative bacteria function as adhesins, but in many cases it is a minor subunit protein at the tip of the fimbriae that is the actual adhesin. In gram-positive bacteria, a protein or polysaccharide surface layer serves as the specific adhesin. What is sometimes called polymeric adhesin (biofilms) is distinct from protein adhesin. Diarrheagenic E. coli to bind BIND Hyperbilirubinemia of the Newborn enterocytes in the small intestine Small intestine The small intestine is the longest part of the GI tract, extending from the pyloric orifice of the stomach to the ileocecal junction. The small intestine is the major organ responsible for chemical digestion and absorption of nutrients. It is divided into 3 segments: the duodenum, the jejunum, and the ileum. Small Intestine: Anatomy and produces the following enterotoxins:
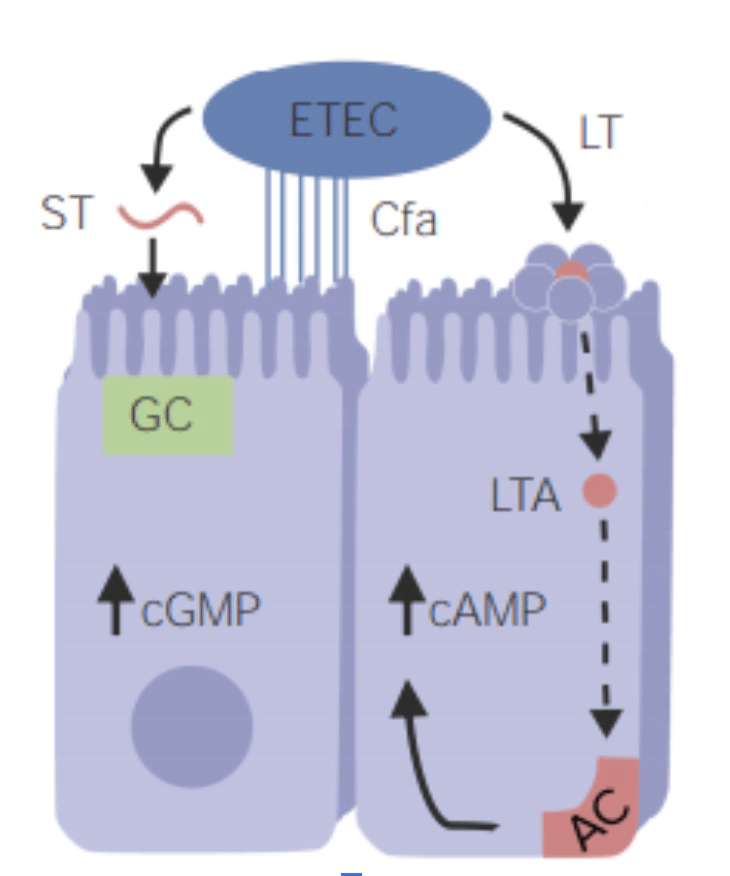
Enterotoxigenic Escherichia coli (ETEC) pathogenesis:
ETEC attaches to enterocytes via colonization factor antigen (CFA; fimbrial adhesin). The heat-stable (ST) enterotoxin causes cyclic guanosine monophosphate (cGMP) accumulation in cells and secretion of fluid and electrolytes into the intestinal lumen. The heat-labile (LT) enterotoxin acts like cholera toxin, which increases cyclic adenosine monophosphate (cAMP) by activating adenylyl cyclase (AC). The general effect is water and chloride hypersecretion and inhibited sodium reabsorption. Noninvasive enterotoxins remain within the intestinal lumen and do not invade the epithelial cells.
GC: guanylyl cyclase
LTA: A subunit of the heat-labile enterotoxin
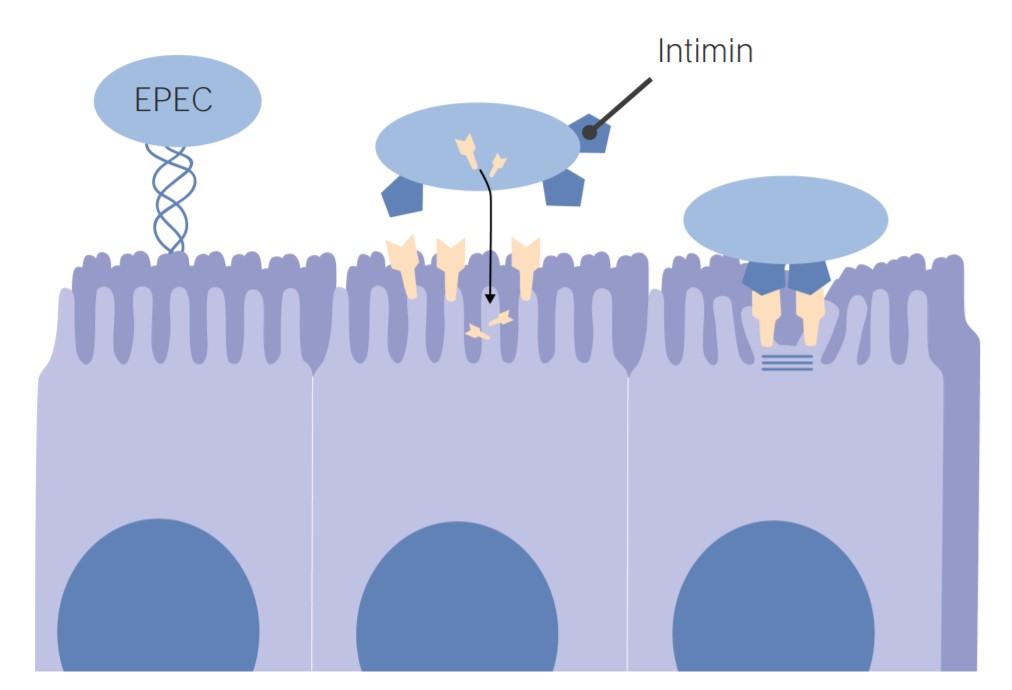
Enteropathogenic Escherichia coli (EPEC) pathogenesis:
EPEC uses intimin adhesion molecules to adhere to the intestinal cells. Binding causes cell deformation (brush border degeneration and loss of microvilli). The characteristic effect of attachment and effacement is the primary cause of diarrhea.
| Pathogenic strain | Pathology |
|---|---|
| ETEC |
Adhesion
Adhesion
The process whereby platelets adhere to something other than platelets, e.g., collagen; basement membrane; microfibrils; or other ‘foreign’ surfaces.
Coagulation Studies molecules: colonizing
fimbriae
Fimbriae
Thin, hairlike appendages, 1 to 20 microns in length and often occurring in large numbers, present on the cells of gram-negative bacteria, particularly enterobacteriaceae and Neisseria. Unlike flagella, they do not possess motility, but being protein (pilin) in nature, they possess antigenic and hemagglutinating properties. They are of medical importance because some fimbriae mediate the attachment of bacteria to cells via adhesins. Bacterial fimbriae refer to common pili, to be distinguished from the preferred use of ‘pili’.
Escherichia coli Plasmid-encoded toxins:
|
| EPEC | Attachment via BFP and
intimin
Intimin
Escherichia coli → cell deformation → microvilli effacement > 20 toxins injected into cells |
| EAEC EAEC Escherichia coli |
Transcription
Transcription
Transcription of genetic information is the first step in gene expression. Transcription is the process by which DNA is used as a template to make mRNA. This process is divided into 3 stages: initiation, elongation, and termination.
Stages of Transcription activator AggR controls adherence
fimbriae
Fimbriae
Thin, hairlike appendages, 1 to 20 microns in length and often occurring in large numbers, present on the cells of gram-negative bacteria, particularly enterobacteriaceae and Neisseria. Unlike flagella, they do not possess motility, but being protein (pilin) in nature, they possess antigenic and hemagglutinating properties. They are of medical importance because some fimbriae mediate the attachment of bacteria to cells via adhesins. Bacterial fimbriae refer to common pili, to be distinguished from the preferred use of ‘pili’.
Escherichia coli–encoding
genes
Genes
A category of nucleic acid sequences that function as units of heredity and which code for the basic instructions for the development, reproduction, and maintenance of organisms.
DNA Types and Structure (
AAF
AAF
Escherichia coli) Forms a biofilm Biofilm Encrustations formed from microbes (bacteria, algae, fungi, plankton, or protozoa) embedded in an extracellular polymeric substance matrix that is secreted by the microbes. They occur on body surfaces such as teeth (dental deposits); inanimate objects, and bodies of water. Biofilms are prevented from forming by treating surfaces with dentifrices; disinfectants; anti-infective agents; and anti-fouling agents. Staphylococcus Some can produce Shiga toxin Shiga toxin A class of toxins that inhibit protein synthesis by blocking the interaction of ribosomal RNA; with peptide elongation factors. They include shiga toxin which is produced by Shigella dysenteriae and a variety of shiga-like toxins that are produced by pathologic strains of Escherichia coli such as Escherichia coli o157. Diarrheagenic E. coli. |
| EIEC EIEC Escherichia coli | Closely related to
Shigella
Shigella
Shigella is a genus of gram-negative, non-lactose-fermenting facultative intracellular bacilli. Infection spreads most commonly via person-to-person contact or through contaminated food and water. Humans are the only known reservoir.
Shigella Invades intestinal cell, multiplies, and extends into adjacent cells |
| EHEC/STEC | Produces
Shiga toxin
Shiga toxin
A class of toxins that inhibit protein synthesis by blocking the interaction of ribosomal RNA; with peptide elongation factors. They include shiga toxin which is produced by Shigella dysenteriae and a variety of shiga-like toxins that are produced by pathologic strains of Escherichia coli such as Escherichia coli o157.
Diarrheagenic E. coli: Inhibits protein synthesis Synthesis Polymerase Chain Reaction (PCR) → enterocyte death → inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation Microangiopathic vascular injury → HUS HUS Hemolytic uremic syndrome (HUS) is a clinical phenomenon most commonly seen in children that consists of a classic triad of microangiopathic hemolytic anemia, thrombocytopenia, and acute kidney injury. Hemolytic uremic syndrome is a major cause of acute kidney injury in children and is most commonly associated with a prodrome of diarrheal illness caused by shiga-like toxin-producing bacteria. Hemolytic Uremic Syndrome Attaching and effacing lesions |
The epidemiologic and clinical features of the different types of diarrheagenic E. coli are described in the table.[3–5]
| Pathogenic strain | Epidemiology | Clinical features |
|---|---|---|
| ETEC | Most common cause of travelers
diarrhea
Diarrhea
Diarrhea is defined as ≥ 3 watery or loose stools in a 24-hour period. There are a multitude of etiologies, which can be classified based on the underlying mechanism of disease. The duration of symptoms (acute or chronic) and characteristics of the stools (e.g., watery, bloody, steatorrheic, mucoid) can help guide further diagnostic evaluation.
Diarrhea > 200 million cases/year |
Incubation
Incubation
The amount time between exposure to an infectious agent and becoming symptomatic.
Rabies Virus: 1–3 days Symptoms last 1–5 days:
|
| EPEC | Infants or young children (< 2 years of age) Most common in resource-limited areas |
|
| EAEC EAEC Escherichia coli | Children, patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with HIV HIV Anti-HIV Drugs, and people in resource-limited areas |
|
| EIEC EIEC Escherichia coli | Uncommon; appears in outbreaks Outbreaks Sudden increase in the incidence of a disease. The concept includes epidemics and pandemics. Influenza Viruses/Influenza and as sporadic Sporadic Selective IgA Deficiency cases |
|
| EHEC/STEC |
Outbreaks
Outbreaks
Sudden increase in the incidence of a disease. The concept includes epidemics and pandemics.
Influenza Viruses/Influenza of serotype O157:H7 HUS HUS Hemolytic uremic syndrome (HUS) is a clinical phenomenon most commonly seen in children that consists of a classic triad of microangiopathic hemolytic anemia, thrombocytopenia, and acute kidney injury. Hemolytic uremic syndrome is a major cause of acute kidney injury in children and is most commonly associated with a prodrome of diarrheal illness caused by shiga-like toxin-producing bacteria. Hemolytic Uremic Syndrome is most common in those < 5 and in those > 60 years of age. |
Incubation
Incubation
The amount time between exposure to an infectious agent and becoming symptomatic.
Rabies Virus period: 3–4 days For the 1st 1–3 days, diarrhea Diarrhea Diarrhea is defined as ≥ 3 watery or loose stools in a 24-hour period. There are a multitude of etiologies, which can be classified based on the underlying mechanism of disease. The duration of symptoms (acute or chronic) and characteristics of the stools (e.g., watery, bloody, steatorrheic, mucoid) can help guide further diagnostic evaluation. Diarrhea is nonbloody, then it becomes bloody in 90% of cases. Other symptoms
HUS HUS Hemolytic uremic syndrome (HUS) is a clinical phenomenon most commonly seen in children that consists of a classic triad of microangiopathic hemolytic anemia, thrombocytopenia, and acute kidney injury. Hemolytic uremic syndrome is a major cause of acute kidney injury in children and is most commonly associated with a prodrome of diarrheal illness caused by shiga-like toxin-producing bacteria. Hemolytic Uremic Syndrome:
|
Diagnosing diarrheagenic E. coli requires a careful history; the diagnosis is confirmed through stool testing.[1,2,6]
Distinguishes diarrheagenic E. coli strains from other types of infectious diarrhea Diarrhea Diarrhea is defined as ≥ 3 watery or loose stools in a 24-hour period. There are a multitude of etiologies, which can be classified based on the underlying mechanism of disease. The duration of symptoms (acute or chronic) and characteristics of the stools (e.g., watery, bloody, steatorrheic, mucoid) can help guide further diagnostic evaluation. Diarrhea.
Indications:[2,13]
Stool tests:
Specimens:
Management is primarily supportive and may include antibiotics.[2,5,6] Confirmed infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease should be reported to the local health department.
Evaluate for dehydration Dehydration The condition that results from excessive loss of water from a living organism. Volume Depletion and Dehydration and provide supportive care:
Antibiotics:
Diagnosis Codes:
Infection with
diarrheagenic E. coli
Diarrheagenic E. coli
Diarrheagenic Escherichia coli are a diverse group of E. coli that are classified into 5 major pathotypes which can cause intestinal infection and diarrhea. Transmission is often through the fecal-oral route via the consumption of contaminated food or water. Pathogenesis varies based on the strain, but it can include toxin production, invasion of the mucosal surface, and adhesion with alteration of enterocyte structure.
Diarrheagenic E. coli is coded based on the specific pathotype, such as
Enterohemorrhagic E. coli
Enterohemorrhagic E. coli
Strains of Escherichia coli that are a subgroup of shiga-toxigenic Escherichia coli. They cause non-bloody and bloody diarrhea; hemolytic uremic syndrome; and hemorrhagic colitis. An important member of this subgroup is Escherichia coli o157-h7.
Escherichia coli (EHEC), which produces
Shiga toxin
Shiga toxin
A class of toxins that inhibit protein synthesis by blocking the interaction of ribosomal RNA; with peptide elongation factors. They include shiga toxin which is produced by Shigella dysenteriae and a variety of shiga-like toxins that are produced by pathologic strains of Escherichia coli such as Escherichia coli o157.
Diarrheagenic E. coli, or
Enterotoxigenic E. coli
Enterotoxigenic E. coli
Strains of Escherichia coli that produce or contain at least one member of either heat-labile or heat-stable enterotoxins. The organisms colonize the mucosal surface of the small intestine and elaborate their enterotoxins causing diarrhea. They are mainly associated with tropical and developing countries and affect susceptible travelers to those places.
Escherichia coli (ETEC), a common cause of traveler’s
diarrhea
Diarrhea
Diarrhea is defined as ≥ 3 watery or loose stools in a 24-hour period. There are a multitude of etiologies, which can be classified based on the underlying mechanism of disease. The duration of symptoms (acute or chronic) and characteristics of the stools (e.g., watery, bloody, steatorrheic, mucoid) can help guide further diagnostic evaluation.
Diarrhea.
| Coding System | Code | Description |
|---|---|---|
| ICD-10-CM | A04.3 | Enterohemorrhagic Escherichia coli Enterohemorrhagic Escherichia coli Strains of Escherichia coli that are a subgroup of shiga-toxigenic Escherichia coli. They cause non-bloody and bloody diarrhea; hemolytic uremic syndrome; and hemorrhagic colitis. An important member of this subgroup is Escherichia coli o157-h7. Diarrheagenic E. coli infection |
| ICD-10-CM | A04.1 | Enterotoxigenic Escherichia coli Enterotoxigenic Escherichia coli Strains of Escherichia coli that produce or contain at least one member of either heat-labile or heat-stable enterotoxins. The organisms colonize the mucosal surface of the small intestine and elaborate their enterotoxins causing diarrhea. They are mainly associated with tropical and developing countries and affect susceptible travelers to those places. Diarrheagenic E. coli infection |
| ICD-10-CM | A04.0 | Enteropathogenic Escherichia coli Enteropathogenic Escherichia coli Strains of Escherichia coli characterized by attaching-and-effacing histopathology. These strains of bacteria intimately adhere to the epithelial cell membrane and show effacement of microvilli. In developed countries they are associated with infantile diarrhea and infantile gastroenteritis and, in contrast to ETEC strains, do not produce endotoxins. Diarrheagenic E. coli infection |
Evaluation & Workup:
These codes are for stool studies used to identify the pathogenic E. coli. This includes a standard stool culture and a specific assay for
Shiga toxin
Shiga toxin
A class of toxins that inhibit protein synthesis by blocking the interaction of ribosomal RNA; with peptide elongation factors. They include shiga toxin which is produced by Shigella dysenteriae and a variety of shiga-like toxins that are produced by pathologic strains of Escherichia coli such as Escherichia coli o157.
Diarrheagenic E. coli, which is crucial for identifying EHEC.
| Coding System | Code | Description |
|---|---|---|
| CPT | 87045 | Culture, bacterial; stool |
| CPT | 87427 | Infectious agent antigen detection Antigen detection Respiratory Syncytial Virus by immunoassay technique; Shiga-like toxin Shiga-Like Toxin Hemolytic Uremic Syndrome |
Complications:
This code is for
Hemolytic Uremic Syndrome
Hemolytic uremic syndrome
A syndrome that is associated with microvascular diseases of the kidney, such as renal cortical necrosis. It is characterized by hemolytic anemia; thrombocytopenia; and acute renal failure.
Hypocoagulable Conditions (
HUS
HUS
Hemolytic uremic syndrome (HUS) is a clinical phenomenon most commonly seen in children that consists of a classic triad of microangiopathic hemolytic anemia, thrombocytopenia, and acute kidney injury. Hemolytic uremic syndrome is a major cause of acute kidney injury in children and is most commonly associated with a prodrome of diarrheal illness caused by shiga-like toxin-producing bacteria.
Hemolytic Uremic Syndrome), a life-threatening complication primarily associated with Shiga toxin-producing E. coli (EHEC) infection.
| Coding System | Code | Description |
|---|---|---|
| ICD-10-CM | D59.31 | Shiga toxin-associated hemolytic-uremic syndrome (STEC-HUS) |