The urogenital system is derived from intermediate mesoderm Mesoderm The middle germ layer of an embryo derived from three paired mesenchymal aggregates along the neural tube. Gastrulation and Neurulation. The intermediate mesoderm Mesoderm The middle germ layer of an embryo derived from three paired mesenchymal aggregates along the neural tube. Gastrulation and Neurulation differentiates into nephrogenic cords (which will go on to form the urinary system) and an adjacent area known as the gonadal ridge (which will go on to form the gonads Gonads The gamete-producing glands, ovary or testis. Hormones: Overview and Types). The nephrogenic cords elongate in a caudal direction and sequentially develop 3 different structures: the pronephros (rudimentary and nonfunctional), the mesonephros (forms the primitive urinary system), and the metanephros (forms the permanent kidney). Concurrently, the genital system develops in close association with the urinary system. Genital development depends on chromosomal sex Chromosomal sex Sex Determination, which determines whether the primitive gonads Gonads The gamete-producing glands, ovary or testis. Hormones: Overview and Types differentiate into testes Testes Gonadal Hormones or ovaries Ovaries Ovaries are the paired gonads of the female reproductive system that contain haploid gametes known as oocytes. The ovaries are located intraperitoneally in the pelvis, just posterior to the broad ligament, and are connected to the pelvic sidewall and to the uterus by ligaments. These organs function to secrete hormones (estrogen and progesterone) and to produce the female germ cells (oocytes). Ovaries: Anatomy. The gonads Gonads The gamete-producing glands, ovary or testis. Hormones: Overview and Types then secrete certain hormones Hormones Hormones are messenger molecules that are synthesized in one part of the body and move through the bloodstream to exert specific regulatory effects on another part of the body. Hormones play critical roles in coordinating cellular activities throughout the body in response to the constant changes in both the internal and external environments. Hormones: Overview and Types, which direct further development of both the internal and external genital structures.
Last updated: Dec 15, 2025
Develops around week 2 of embryonic life:
Layers:
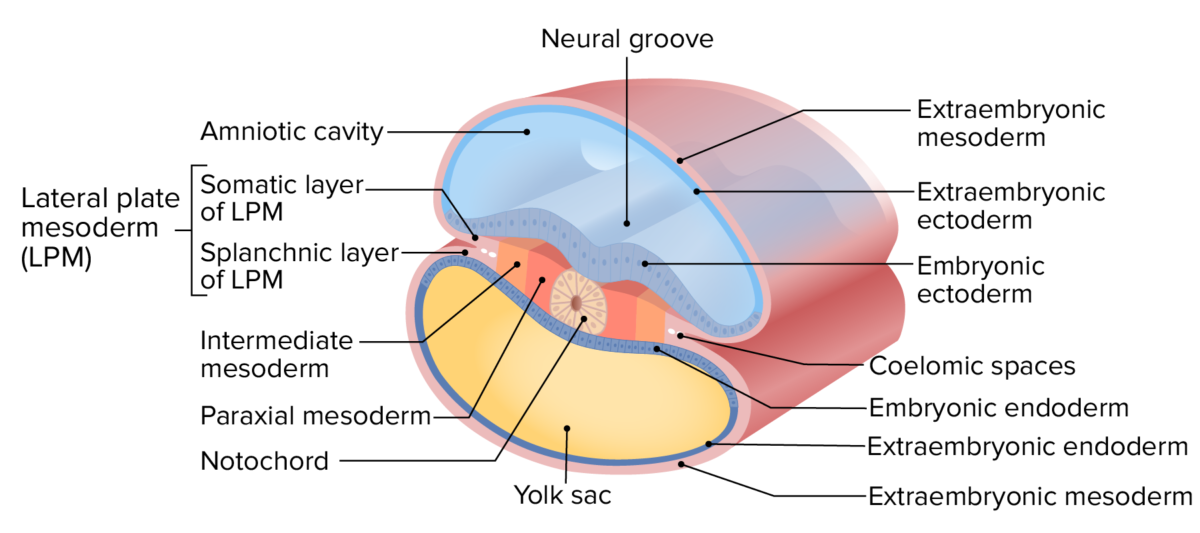
Layers of the trilaminar disc
Image by Lecturio.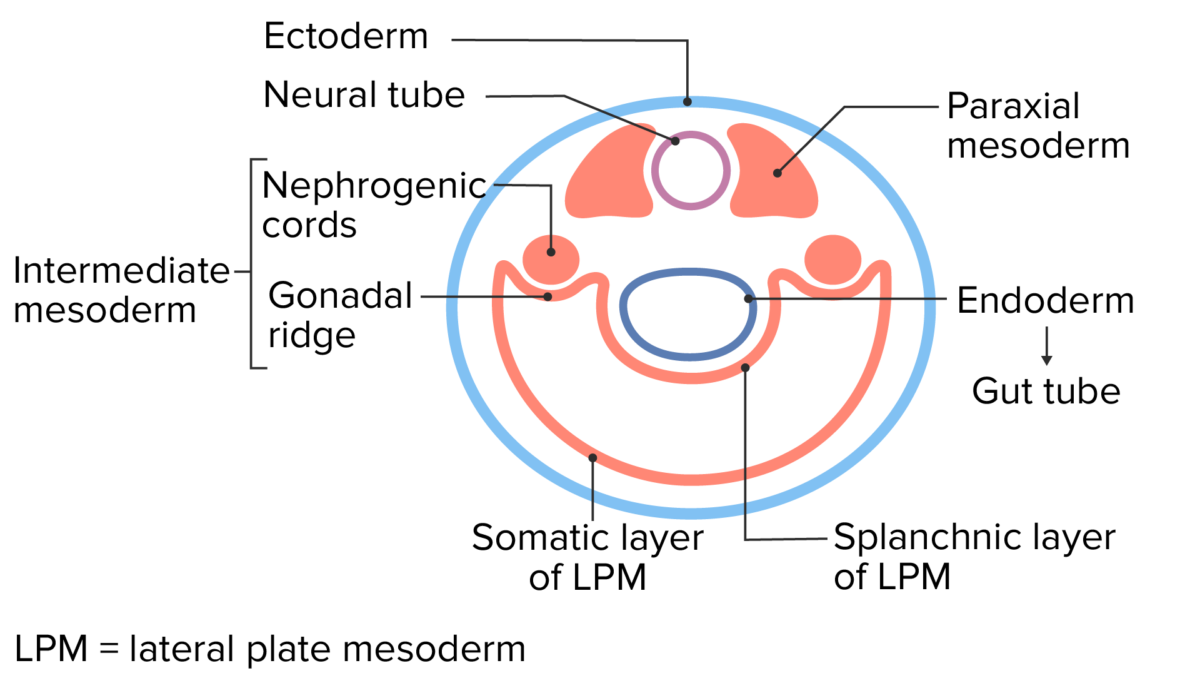
Cross-sectional view of the early embryo
Image by Lecturio.The kidney develops from embryonic mesoderm Mesoderm The middle germ layer of an embryo derived from three paired mesenchymal aggregates along the neural tube. Gastrulation and Neurulation in 3 successive forms from the nephrogenic cords as the cords elongate in a cranial-to-caudal direction.
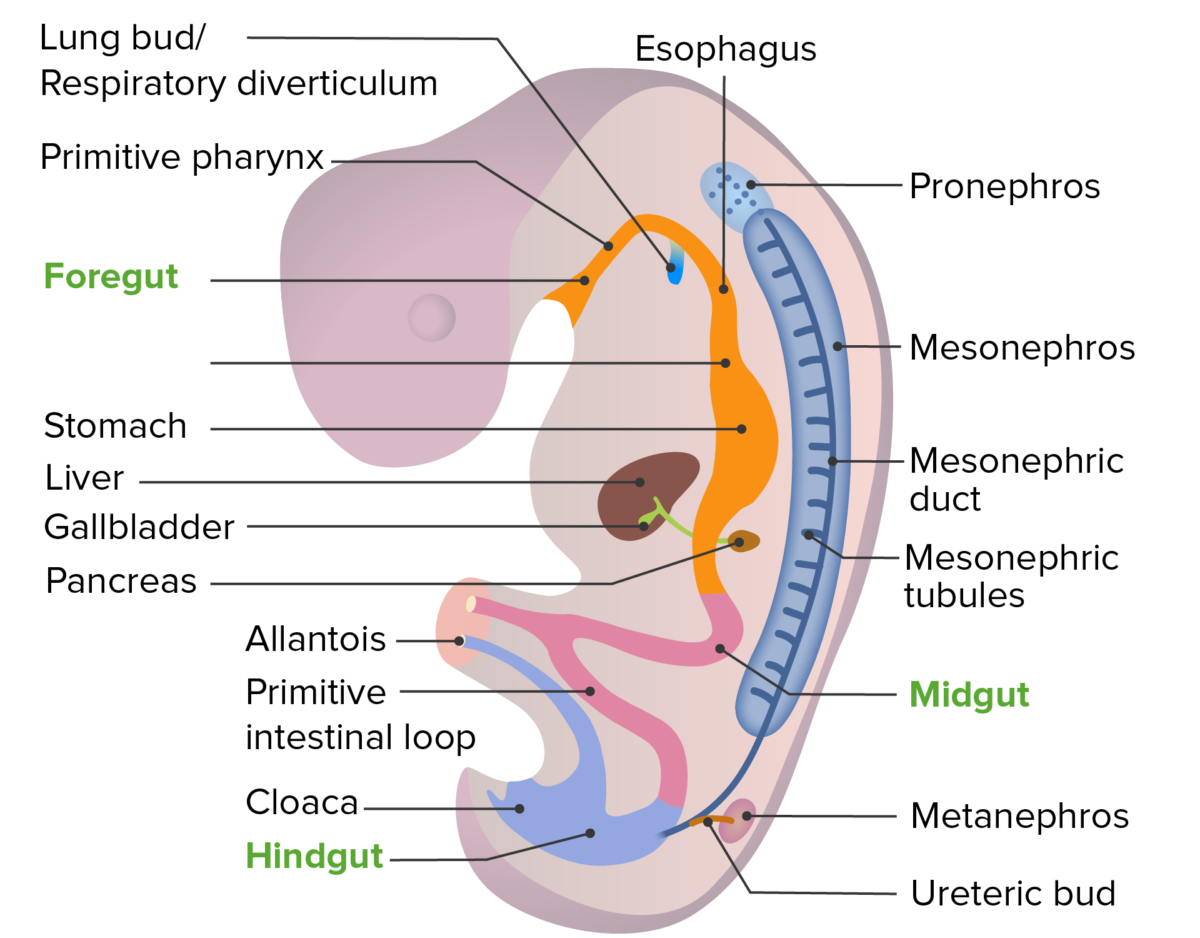
Developmental location of the pronephros, mesonephros, and metanephros in the developing embryo
Image by Lecturio.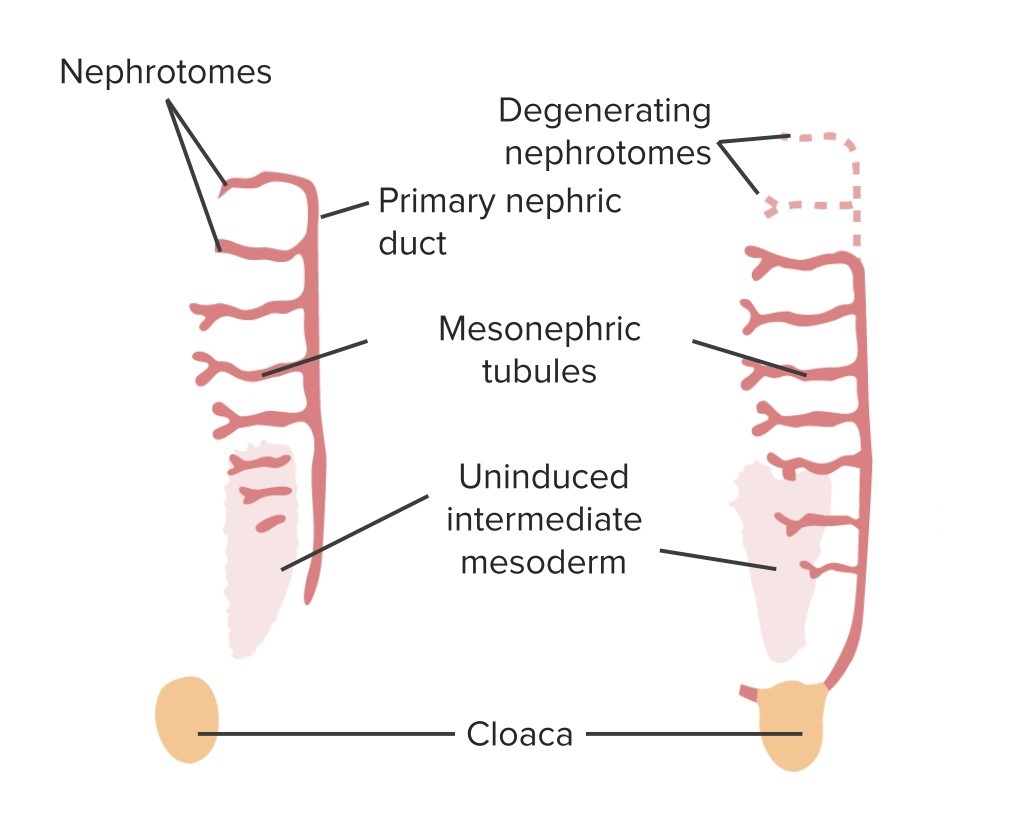
Graphical summary of the mesonephros:
Note that the nephrogenic cords (primary nephric ducts) elongate and join with the cloaca. Mesonephric tubules grow in a stepladder-like pattern and function as a primitive urinary system, while the definitive kidney develops from the metanephros further down in the growing pelvis.
The permanent kidney is formed from the metanephros.
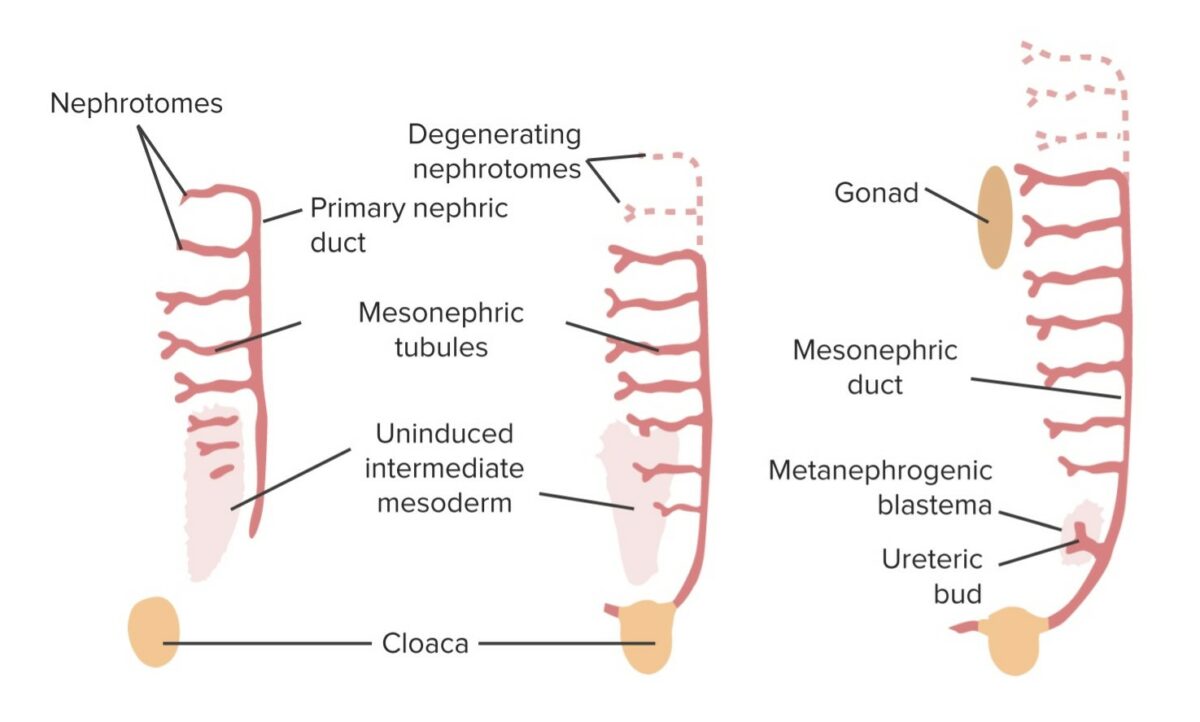
Graphical summary of the developing kidney:
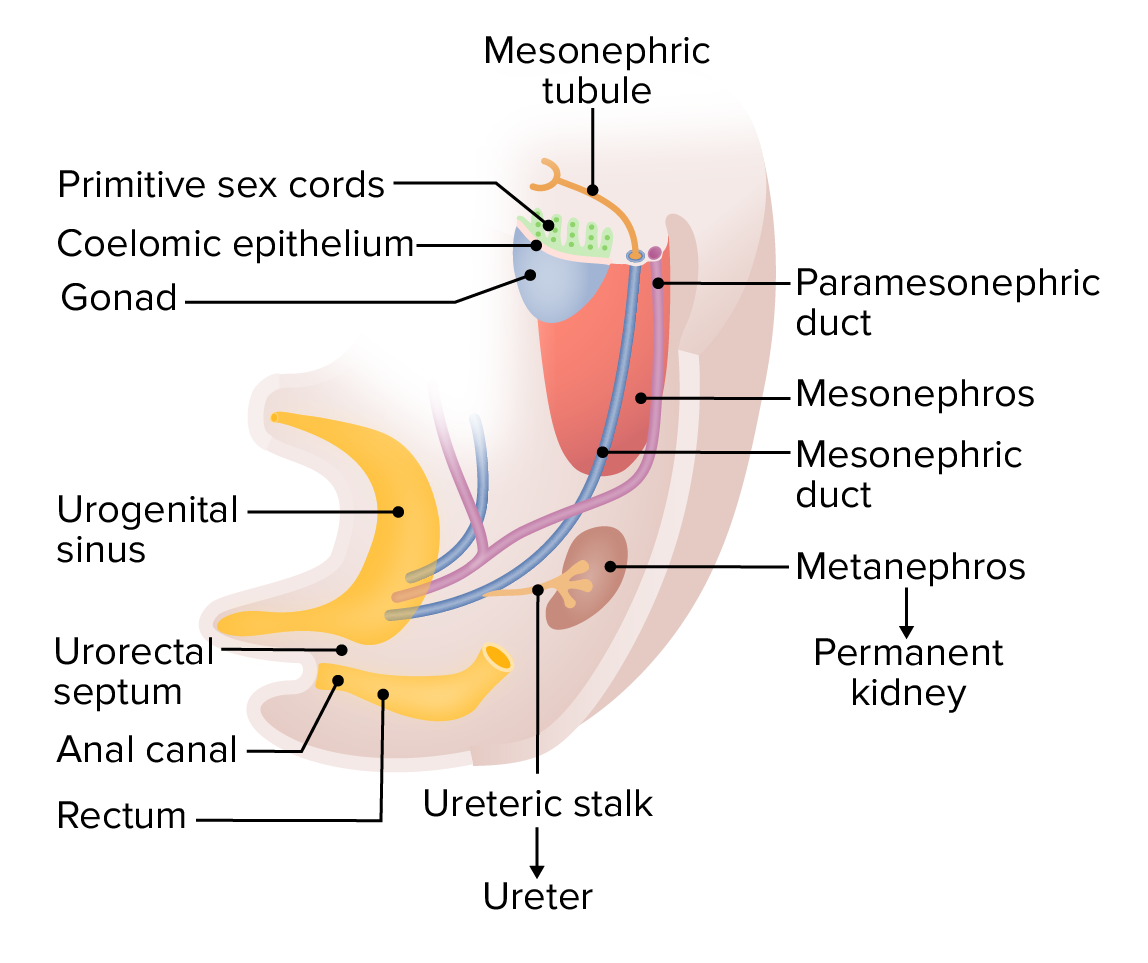
The ureteric bud grows off of the mesonephric duct and into a collection of intermediate mesoderm cells known as the metanephric blastema. Together, these are known as the mesonephros, which develops into the kidney. The mesonephric tubules regress. In males, the mesonephric duct persists in the ejaculatory system.
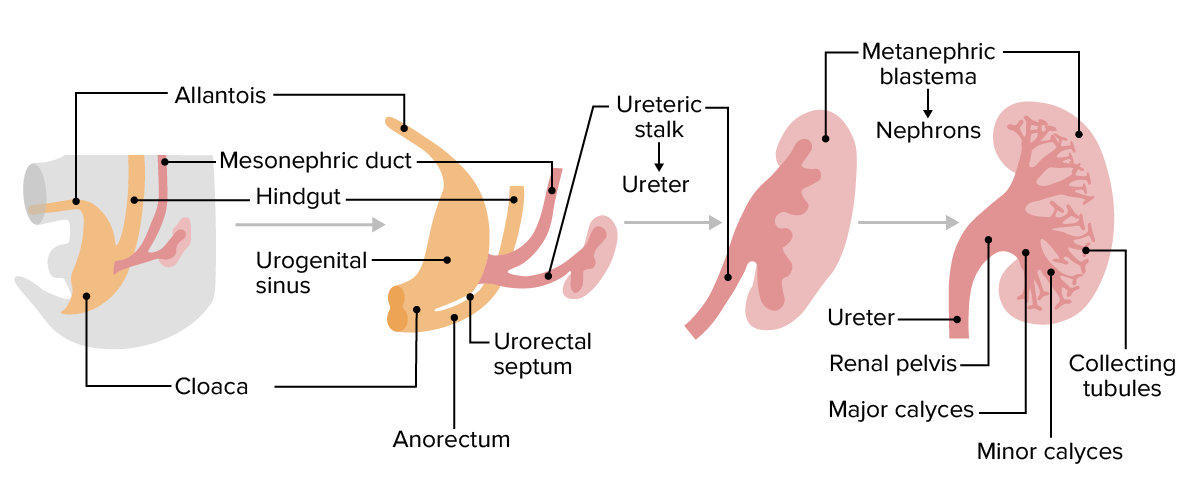
Growth, elongation, and division of the ureteric buds, which form the ureters, the renal pelvis, the major and minor calyces, and the collecting tubule
Image by Lecturio.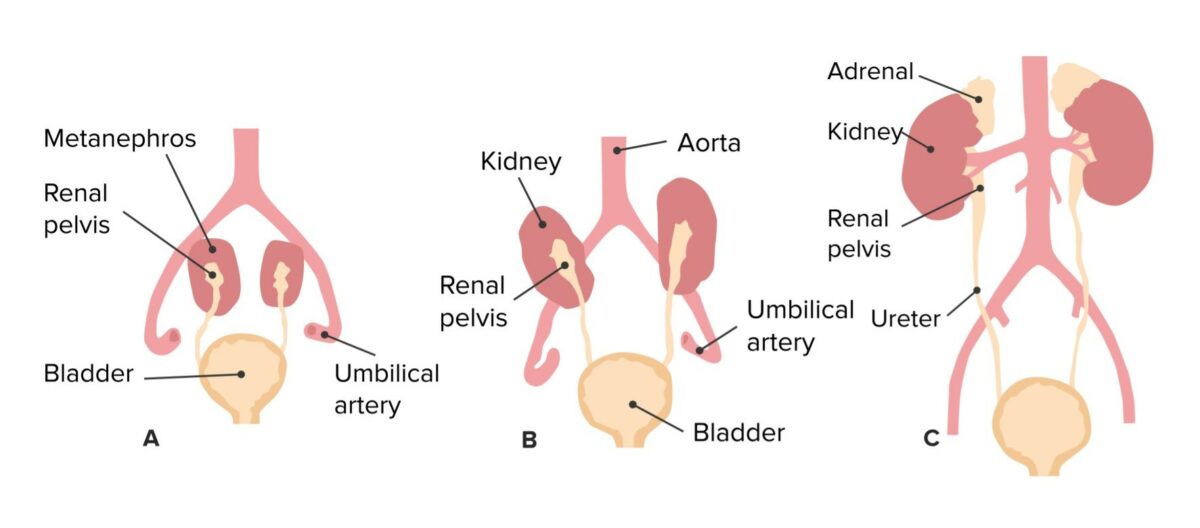
Ascent of the kidneys and corresponding change in vascular supply
Image by Lecturio.Between the 4th and 7th weeks of development, the cloaca Cloaca A dilated cavity extended caudally from the hindgut. In adult birds, reptiles, amphibians, and many fishes but few mammals, cloaca is a common chamber into which the digestive, urinary and reproductive tracts discharge their contents. In most mammals, cloaca gives rise to large intestine; urinary bladder; and genitalia. Development of the Abdominal Organs divides into:
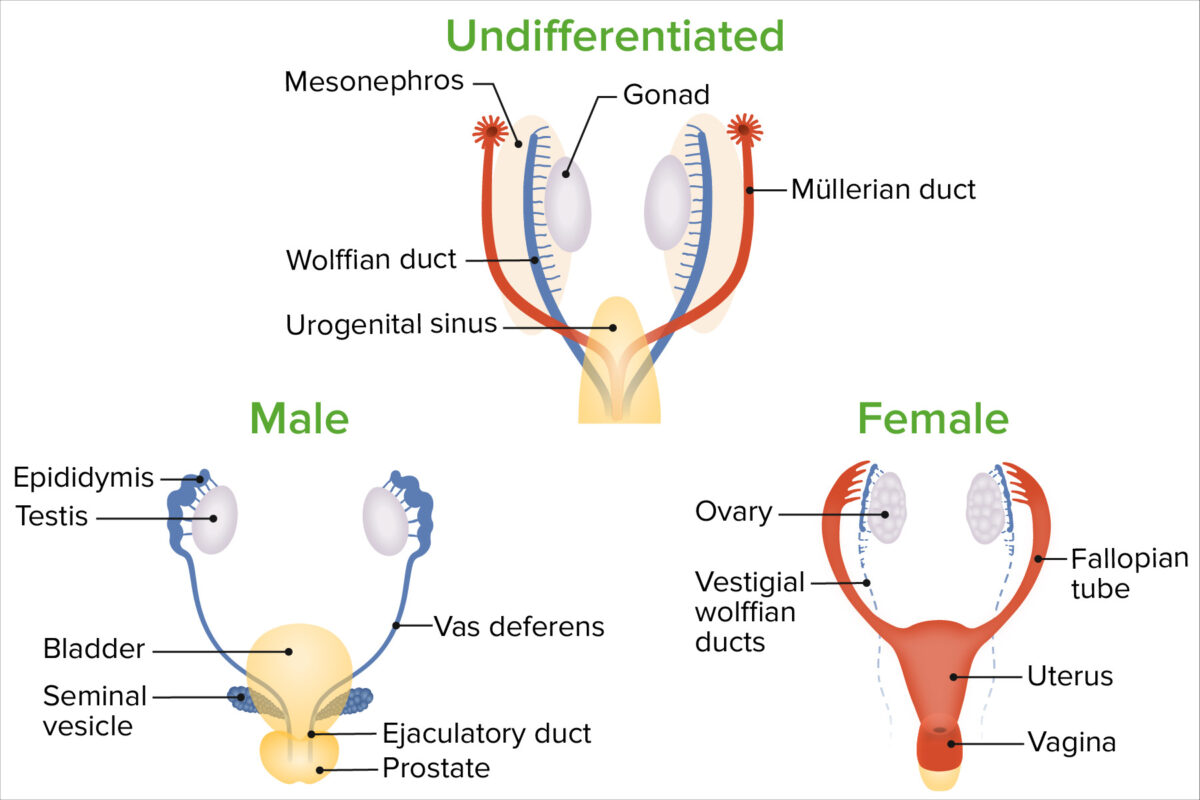
Sex differentiation from the mesonephric (wolffian) and paramesonephric (müllerian) ducts:
In females, the mesonephric ducts regress while the paramesonephric ducts persist. The paramesonephric ducts remain open to the intraembryonic coelom (the eventual peritoneal cavity) near the gonads, and the inferior/medial ends fuse into a common body in the midline, forming the uterus and upper vagina.
In males, the mesonephric ducts are closely associated with the gonads; they enter the urogenital sinus separately on each side becoming parts of the ejaculatory system, while the urogenital sinus becomes the bladder and prostate.
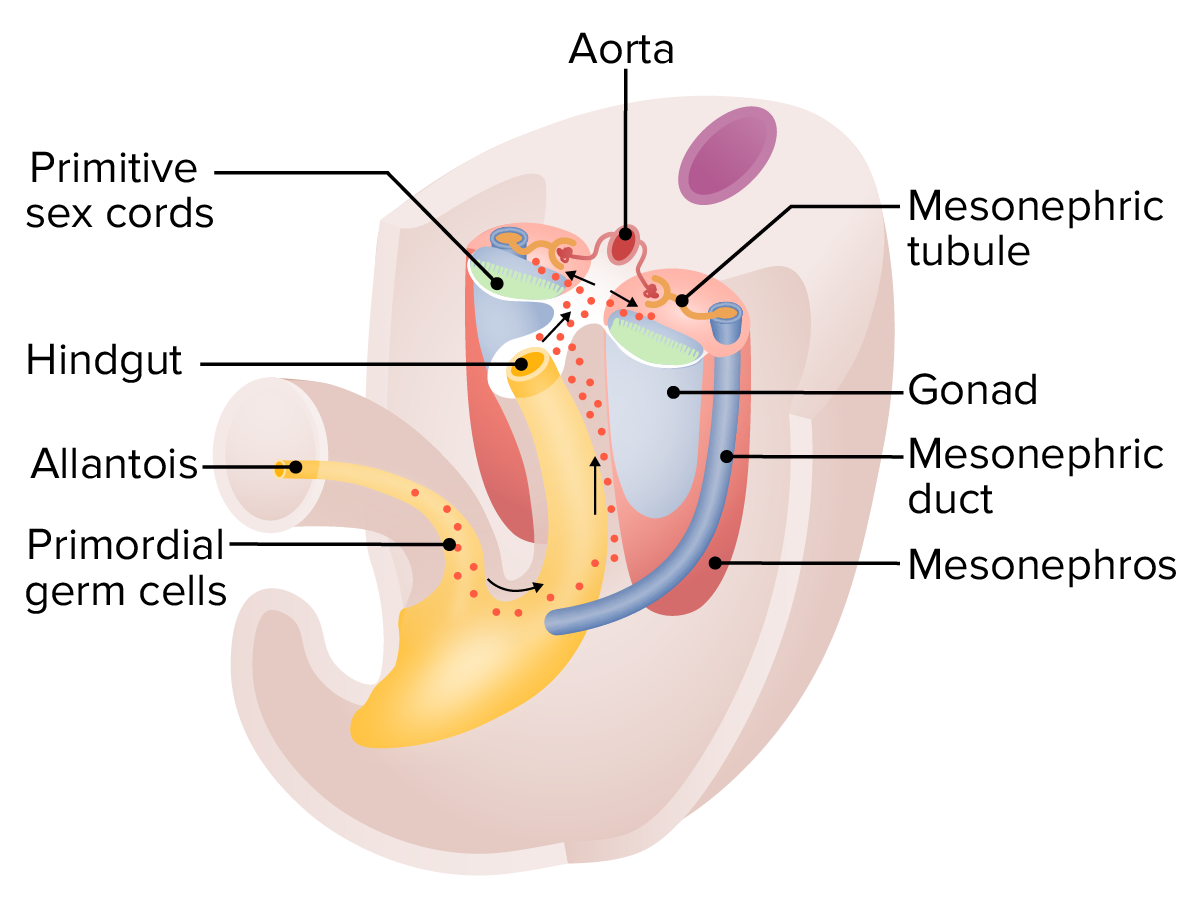
Migration of the primordial germ cells around 5 weeks:
These germ cells begin as epiblast cells and start developing within the yolk sac. The cells then migrate down the allantois, along the dorsal mesentery of the hindgut, and then invade the gonadal ridges, which are beginning to form the early gonads.
Formation of primitive sex cords:
At around 6 weeks, the mesothelium of the gonads invades underlying mesoderm, forming the primitive sex cords. Paramesonephric ducts develop alongside the mesonephric ducts. At this stage, the mesonephric ducts are functioning as part of the primitive urinary system (mesonephros); however, as the definitive kidney (from the metanephros) takes over, the mesonephric ducts will begin differentiating into male genital structures in males or regress in females.
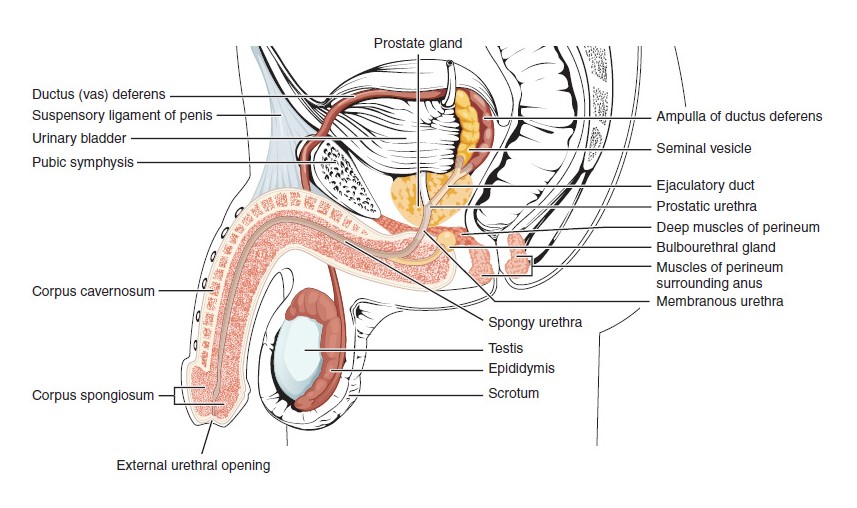
Structures of the male reproductive system
Image: “Male Reproductive System” by OpenStax College. License: CC BY 4.0, cropped by Lecturio.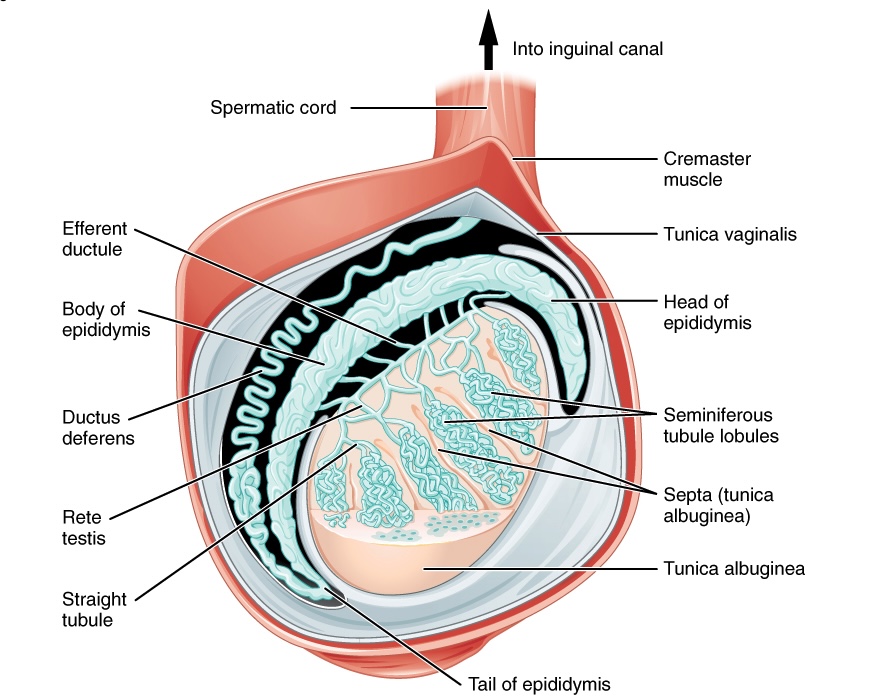
Anatomy of the testis
Image: “Anatomy of the testis” by OpenStax College. License: CC BY 4.0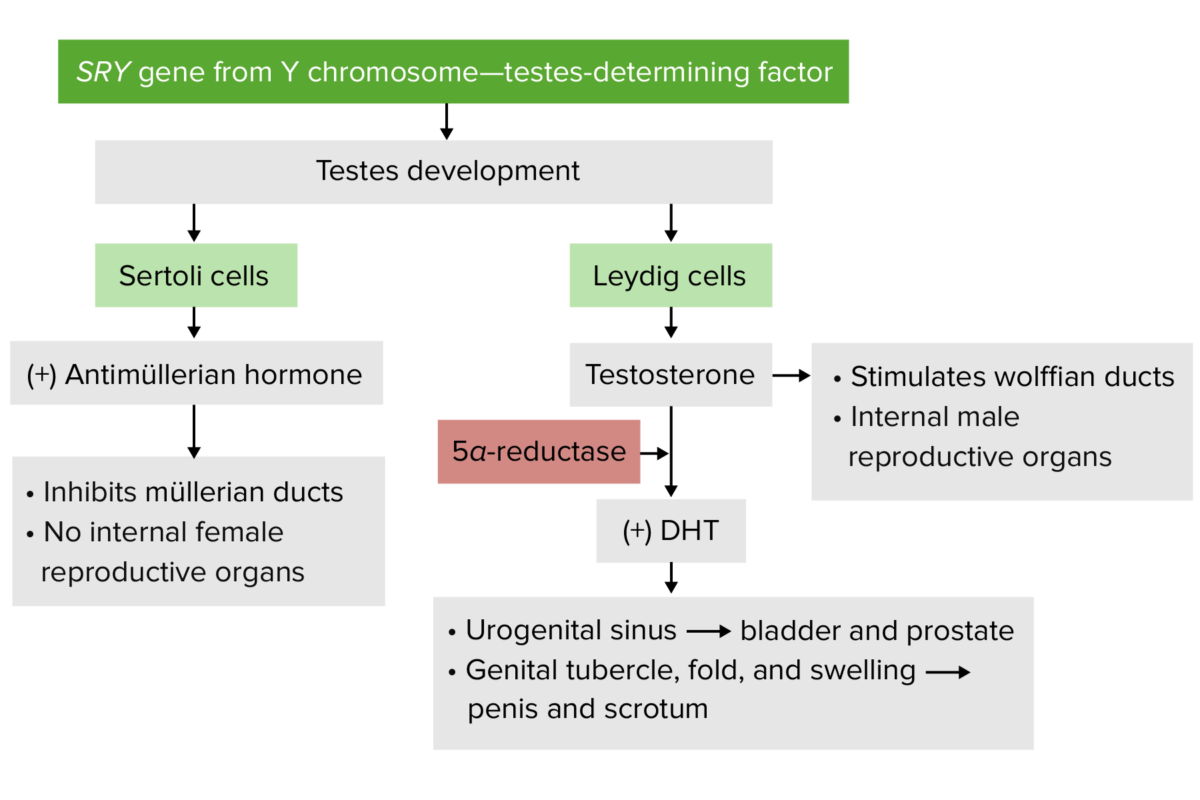
Male development
Image by Lecturio.Step 1: Fusion of the paramesonephric ducts
Step 2: Connection of the fused paramesonephric ducts to the urogenital sinus Urogenital Sinus Congenital Malformations of the Female Reproductive System
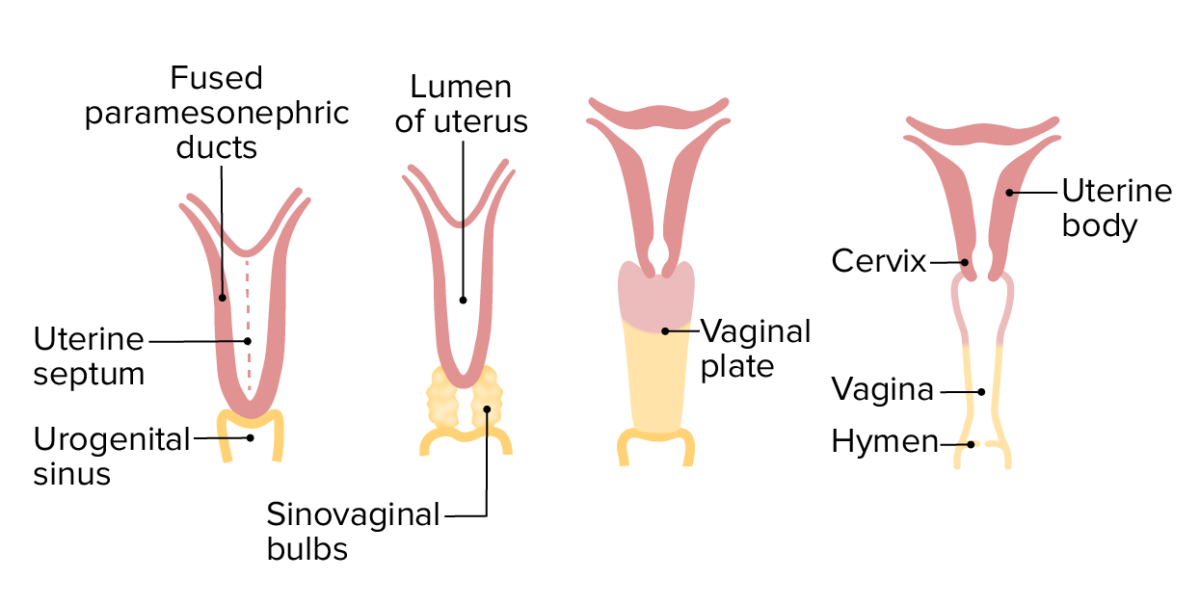
Development of the uterus, cervix, and vagina (anterior view)
Image by Lecturio.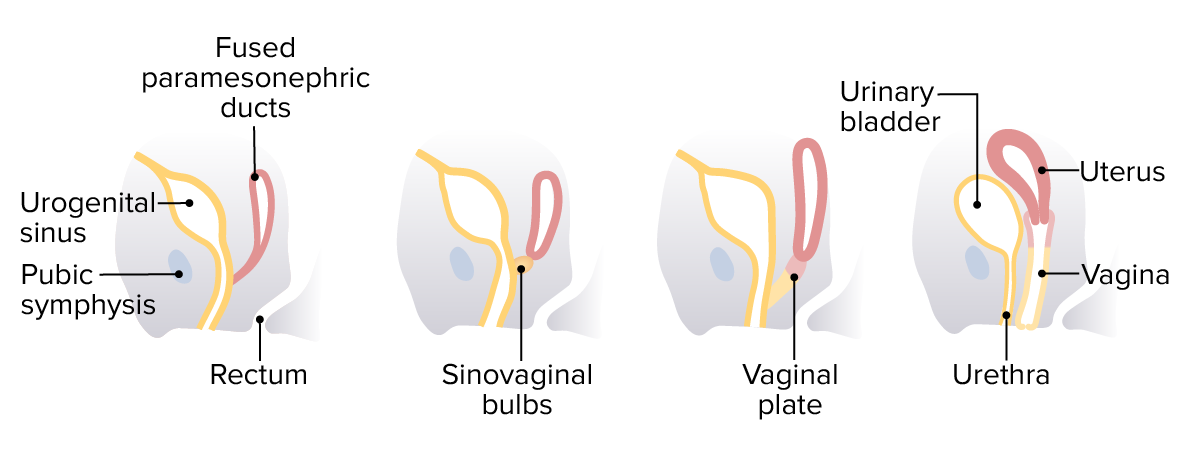
Development of the uterus, cervix, and vagina (lateral view)
Image by Lecturio.| Undifferentiated structure | In the presence of testosterone Testosterone A potent androgenic steroid and major product secreted by the leydig cells of the testis. Its production is stimulated by luteinizing hormone from the pituitary gland. In turn, testosterone exerts feedback control of the pituitary LH and FSH secretion. Depending on the tissues, testosterone can be further converted to dihydrotestosterone or estradiol. Androgens and Antiandrogens | Estrogen Estrogen Compounds that interact with estrogen receptors in target tissues to bring about the effects similar to those of estradiol. Estrogens stimulate the female reproductive organs, and the development of secondary female sex characteristics. Estrogenic chemicals include natural, synthetic, steroidal, or non-steroidal compounds. Ovaries: Anatomy/lack of testosterone Testosterone A potent androgenic steroid and major product secreted by the leydig cells of the testis. Its production is stimulated by luteinizing hormone from the pituitary gland. In turn, testosterone exerts feedback control of the pituitary LH and FSH secretion. Depending on the tissues, testosterone can be further converted to dihydrotestosterone or estradiol. Androgens and Antiandrogens |
|---|---|---|
| Urogenital sinus Urogenital Sinus Congenital Malformations of the Female Reproductive System |
|
|
| Genital tubercle (forms erectile tissue) |
|
|
| Genital folds |
|
Labia minora Labia minora Vagina, Vulva, and Pelvic Floor: Anatomy |
| Genital swelling Swelling Inflammation | Scrotum Scrotum A cutaneous pouch of skin containing the testicles and spermatic cords. Testicles: Anatomy | Labia majora Labia majora Vagina, Vulva, and Pelvic Floor: Anatomy |
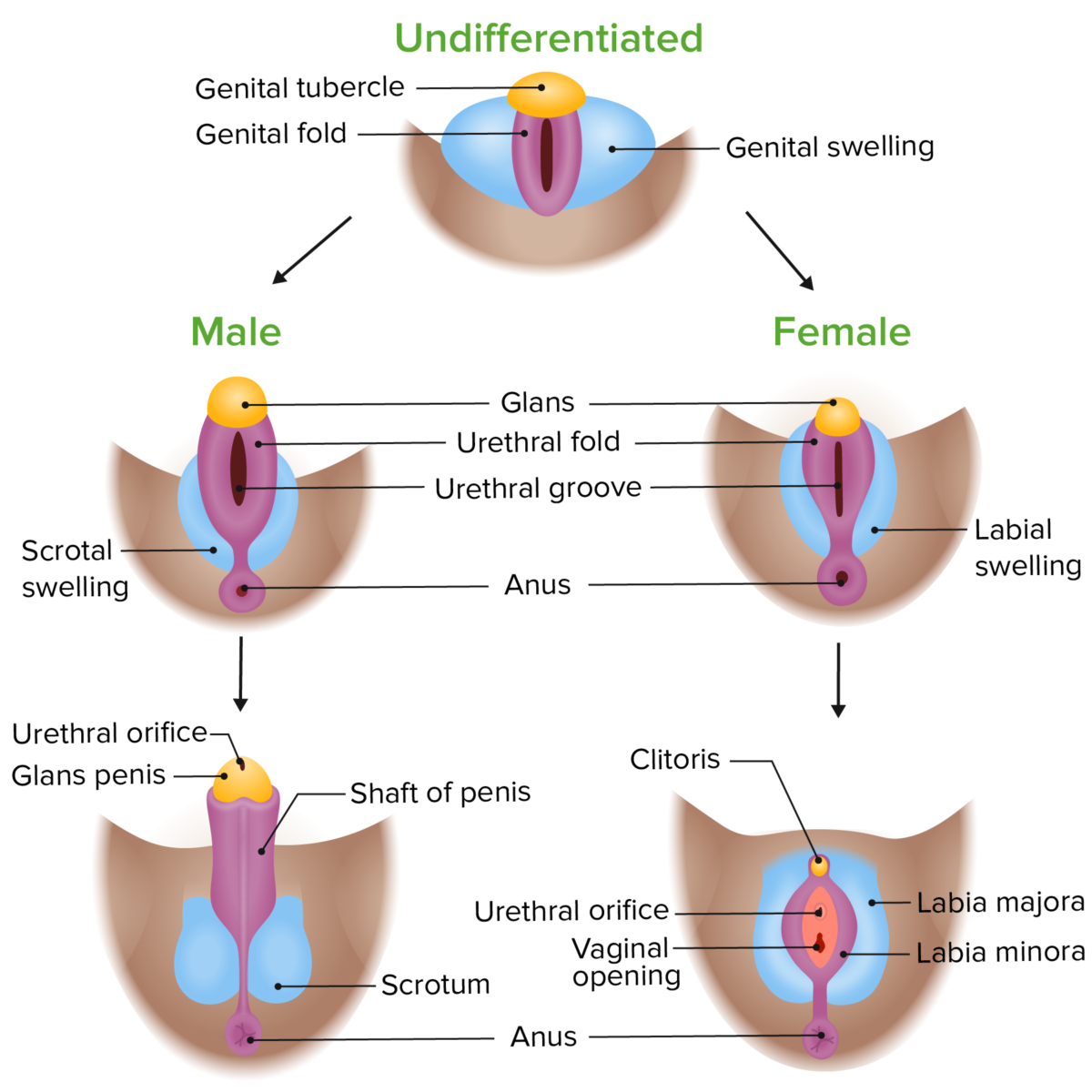
Phenotypic differentiation of the external genitalia in male and female embryos:
Both male and female external genitalia develop from the same starting structures but diverge as they are exposed to different levels of androgens and estrogens.
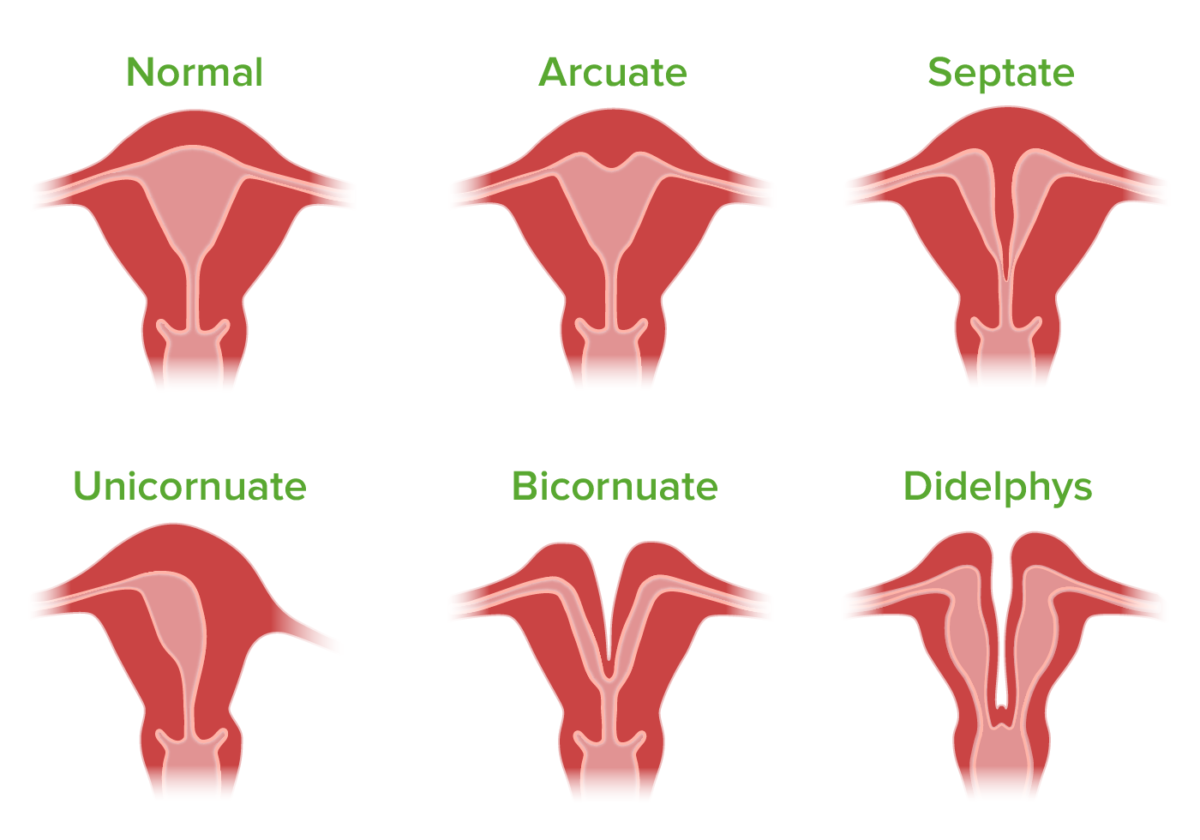
Illustration showing types of congenital malformations of the uterus
Image by Lecturio. License: CC BY-NC-SA 4.0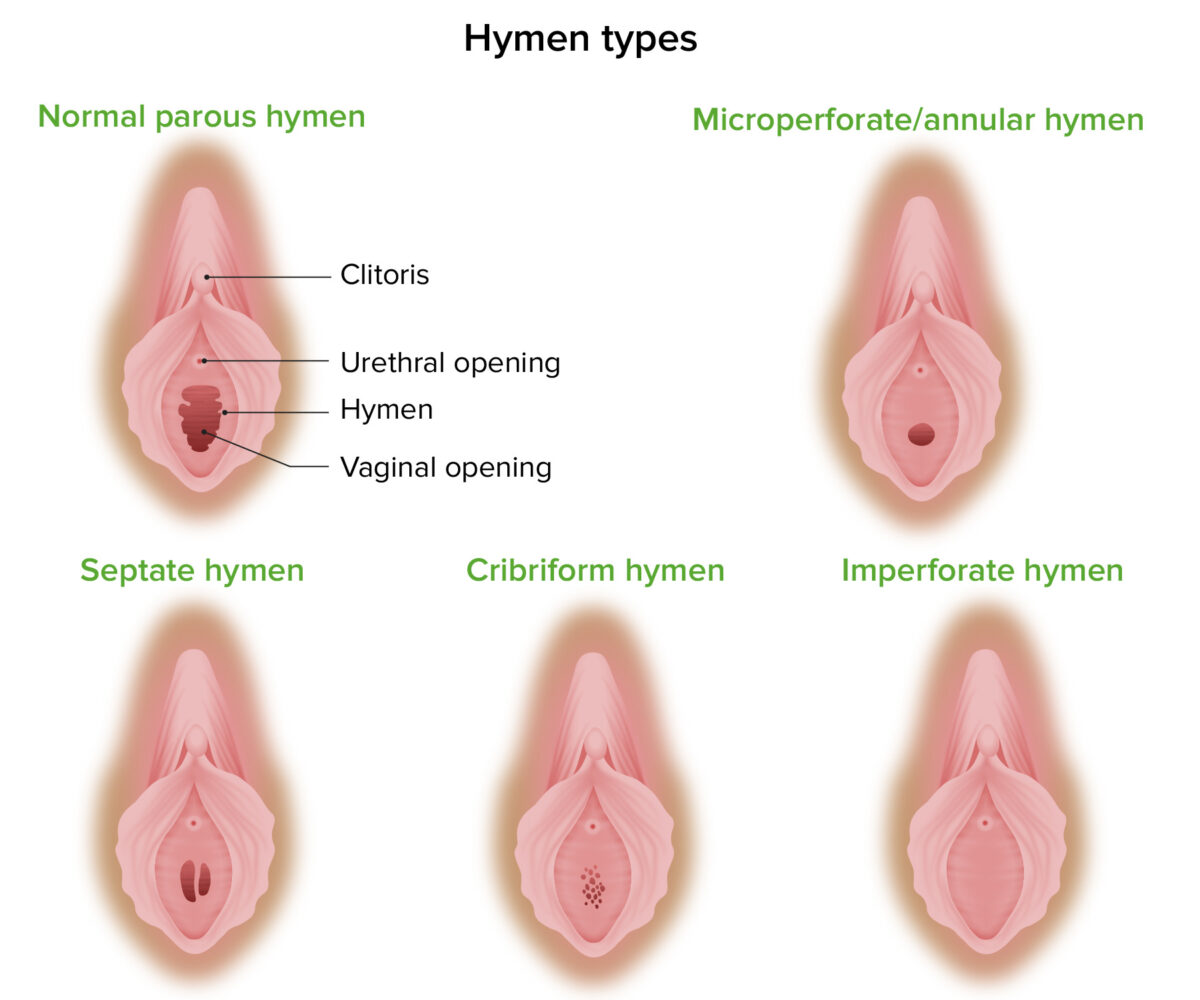
Normal parous hymen compared to common hymen malformations, including microperforate, septate, cribriform, and imperforate hymens
Image by Lecturio. License: CC BY-NC-SA 4.0Disorders of sexual development (DSDs) are a group of conditions characterized by atypical sexual development in an individual, which may involve abnormalities in the structure and/or function of the internal reproductive organs and/or external genitalia.