Decision-making capacity and legal competence are terms often used interchangeably in a hospital setting to describe an individual's ability to make consequential decisions regarding themselves, as a manifestation of their autonomy Autonomy Respect for the patient’s right to self-rule. Medical Ethics: Basic Principles. More specifically, however, capacity describes a patient’s ability to make autonomous decisions regarding their care, as determined by a physician, whereas competence is a legal term that describes a person’s ability to participate in legal processes, as determined by a judge.
Last updated: Dec 15, 2025
Decision-making capacity is a patient’s ability to understand a proposed intervention, its benefits, risks, and alternatives, including the option of no treatment, and make autonomous decisions regarding their care.
There are 4 primary components of medical capacity:
| Component | Determinant elements |
|---|---|
| Understanding |
|
| Communication/expression of choice |
|
| Appreciation |
|
| Reasoning |
|
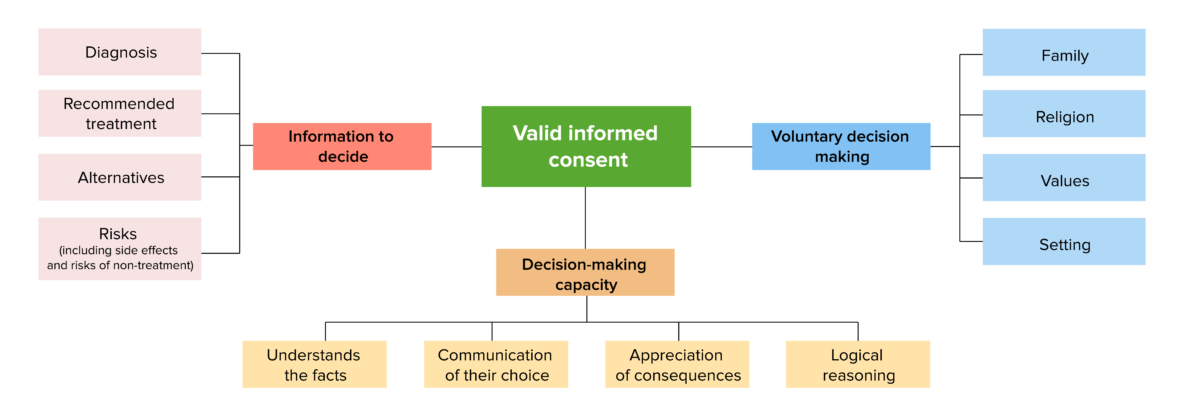
Components of medical decision-making capacity
Image by Lecturio. License: CC BY-NC-SA 4.0The clinician Clinician A physician, nurse practitioner, physician assistant, or another health professional who is directly involved in patient care and has a professional relationship with patients. Clinician–Patient Relationship assesses the 4 elements intuitively through everyday interactions with the patient (e.g., during daily rounds).
The steps below usually take the form of a fluid conversation that doesn’t necessarily follow a strict order. Throughout the conversation, the clinician Clinician A physician, nurse practitioner, physician assistant, or another health professional who is directly involved in patient care and has a professional relationship with patients. Clinician–Patient Relationship should be able to determine if the patient fulfills the 4 elements.
| Fear or discomfort | Expression of fear or discomfort in a clinical setting |
|---|---|
| Age |
|
| Neurologic, psychiatric, or developmental conditions |
|
| Significant cultural or language barriers | Inability to understand the clinical team due to lack of language competency |
Competency, or competence, is a legal term defined as the ability of an individual to participate in legal proceedings, which includes their ability to make medical decisions. Determinations of competence are made by a judge and not by a physician.
The components of competence as determined by a judge are listed below. Note the similarity to the 4 components of medical decision-making capacity.