Coma is defined as a deep state of unarousable unresponsiveness, characterized by a score of 3 points on the GCS. A comatose state can be caused by a multitude of conditions, making the precise etiology and prognosis of coma difficult to determine. Diagnosis is made clinically with a thorough neurologic examination, including assessment of the brain stem to evaluate for the presence of brain death. Imaging studies and laboratory tests are dictated by the presentation and history. Definitive management depends on the underlying cause.
Last updated: Jan 17, 2024
| Description | Points | |
|---|---|---|
| Eye opening | Spontaneous | 4 |
| Responds to speech | 3 | |
| Responds to pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways | 2 | |
| None | 1 | |
| Best verbal response | Oriented | 5 |
| Confused | 4 | |
| Inappropriate words | 3 | |
| Incomprehensible words | 2 | |
| None | 1 | |
| Best motor Motor Neurons which send impulses peripherally to activate muscles or secretory cells. Nervous System: Histology response | Obeys commands | 6 |
| Localizes pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways | 5 | |
| Withdraws from pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways | 4 | |
| Decorticate posturing Decorticate Posturing Increased Intracranial Pressure (ICP) ( flexion Flexion Examination of the Upper Limbs) | 3 | |
| Decerebrate posturing Decerebrate posturing A condition characterized by abnormal posturing of the limbs that is associated with injury to the brainstem. This may occur as a clinical manifestation or induced experimentally in animals. The extensor reflexes are exaggerated leading to rigid extension of the limbs accompanied by hyperreflexia and opisthotonus. This condition is usually caused by lesions which occur in the region of the brainstem that lies between the red nuclei and the vestibular nuclei. In contrast, decorticate rigidity is characterized by flexion of the elbows and wrists with extension of the legs and feet. The causative lesion for this condition is located above the red nuclei and usually consists of diffuse cerebral damage. Increased Intracranial Pressure (ICP) ( extension Extension Examination of the Upper Limbs) | 2 | |
| None | 1 |
Difficult to determine because of:
| Structural | Toxic | Metabolic |
|---|---|---|
|
|
|
The specific sequence of events depends on the underlying etiology, but in general terms:
Evaluation and management may occur simultaneously.
Initial:
Neurologic examination (level of response to stimuli):
Brainstem examination:
Remainder of the physical examination is guided by clinical suspicion of the underlying etiology. For example, if meningitis Meningitis Meningitis is inflammation of the meninges, the protective membranes of the brain, and spinal cord. The causes of meningitis are varied, with the most common being bacterial or viral infection. The classic presentation of meningitis is a triad of fever, altered mental status, and nuchal rigidity. Meningitis is suspected, testing for signs of meningeal irritation Meningeal Irritation Subarachnoid Hemorrhage is warranted.
Brainstem and reflexes:
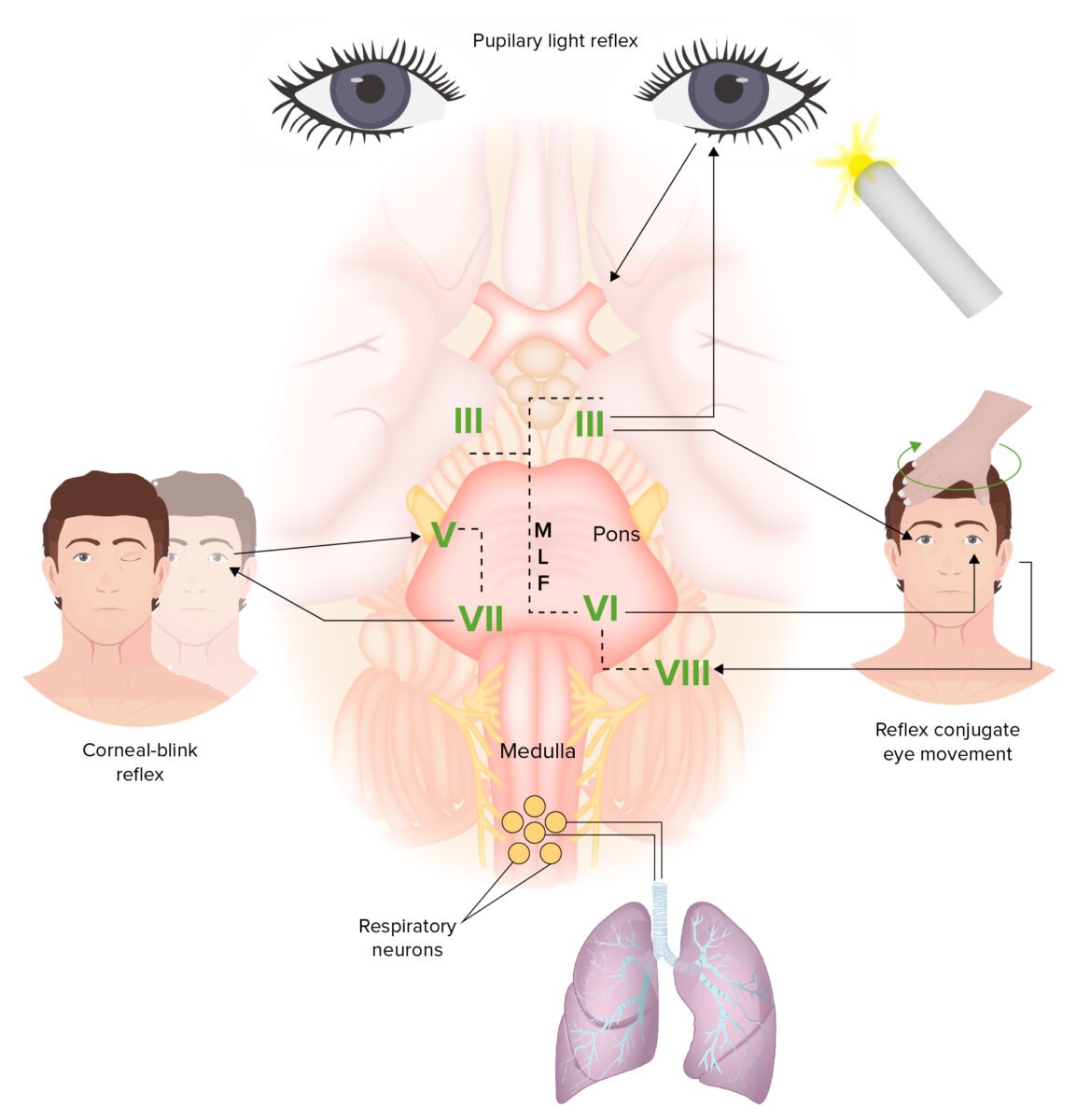
The brainstem connects the pathways between the brain and the spinal cord. Functions controlled by the brainstem include the sleep-wake cycle, brainstem reflexes, and regulation of cardiac rhythm and breathing. The afferent limb of the pupillary light reflex is the optic nerve (CN II); the efferent limb is the oculomotor nerve (CN III). The oculocephalic reflex (dolls eye reflex) involves rotation of the head, a motion detected by the vestibular nerve (CN VIII). The signals then reach the vestibular nucleus. Output is then sent to CN III, which innervates the medial rectus, and the abducens nerve (CN VI), which innervates the lateral rectus. Eye movement coordination is via the medial longitudinal fasciculus (MLF), which has fibers connecting the abducens nucleus to the contralateral oculomotor nucleus. The connection is important in performing horizontal conjugate gaze. The corneal reflex is caused by a loop via the sensory trigeminal nerve (CN V) in the cornea, which projects to the facial nucleus, and the facial nerve (CN VII), which exits the facial nucleus and innervates the orbicularis oculi muscle.
Diagnosis of coma is strictly clinical and relies on a robust neurologic examination. Further investigation (imaging and labs) are carried out to determine etiology.
The laboratory studies to be requested depend on the suspected underlying etiology. Some routine analyses include:
CT/MRI to evaluate for:
Recovery is defined as the return of the ability to convincingly and consistently follow commands.