Colorectal cancer (CRC) is the 2nd-leading cause of cancer-related death in the United States. Almost all cases of CRC are adenocarcinoma and the majority of lesions come from the malignant transformation of an adenomatous polyp. As most CRCs are asymptomatic, screening is essential in detecting early disease. Screening is recommended to start at the age of 45 years, utilizing various screening tools available with colonoscopy, flexible sigmoidoscopy, and fecal tests among them. For high-risk individuals, earlier and more frequent screening Screening Preoperative Care is recommended. Other stool-based strategies and visualization tests are also available for CRC screening Screening Preoperative Care.
Last updated: Dec 15, 2025
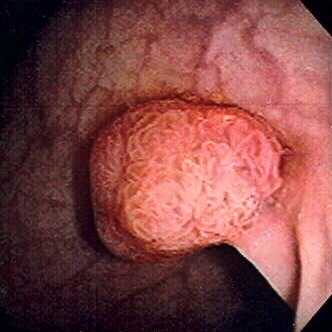
Polyp of sigmoid colon revealed by colonoscopy: The polyp is pedunculated (with a short stalk).
Image: “Colon polyp” by Dr. F.C. Turner. License: CC BY 2.5Colorectal cancer Colorectal cancer Colorectal cancer (CRC) is the 2nd leading cause of cancer-related deaths in the United States. Colorectal cancer is a heterogeneous disease that arises from genetic and epigenetic abnormalities, with influence from environmental factors. Colorectal Cancer is generally a preventable cancer when proper screening Screening Preoperative Care is performed. Screening Screening Preoperative Care:[1-4,11]
Screening Screening Preoperative Care guidelines are based on the most recent US and UK task force and societal guidelines.
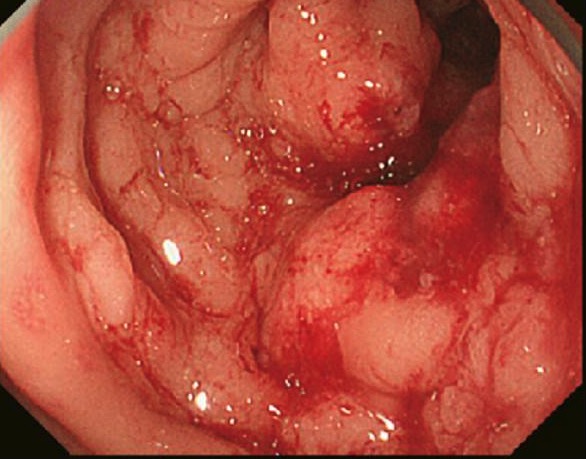
Colon cancer found on colonoscopy confirmed via biopsy
Image: “Primary tumor” by Second Department of Surgery, Wakayama Medical University, School of Medicine, 811-1 Kimiidera, Wakayama 641-8510, Japan. License: CC BY 2.0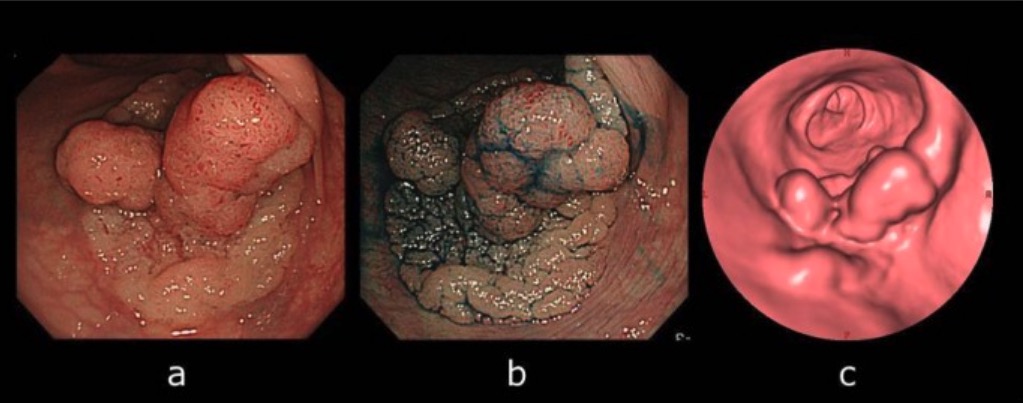
Computed tomographic colonography (CTC) and colonoscopy:
A: Colonoscopy view of the lesion
B: Lesion became apparent by indigo-carmine spraying.
C: CTC showing laterally spreading lesion
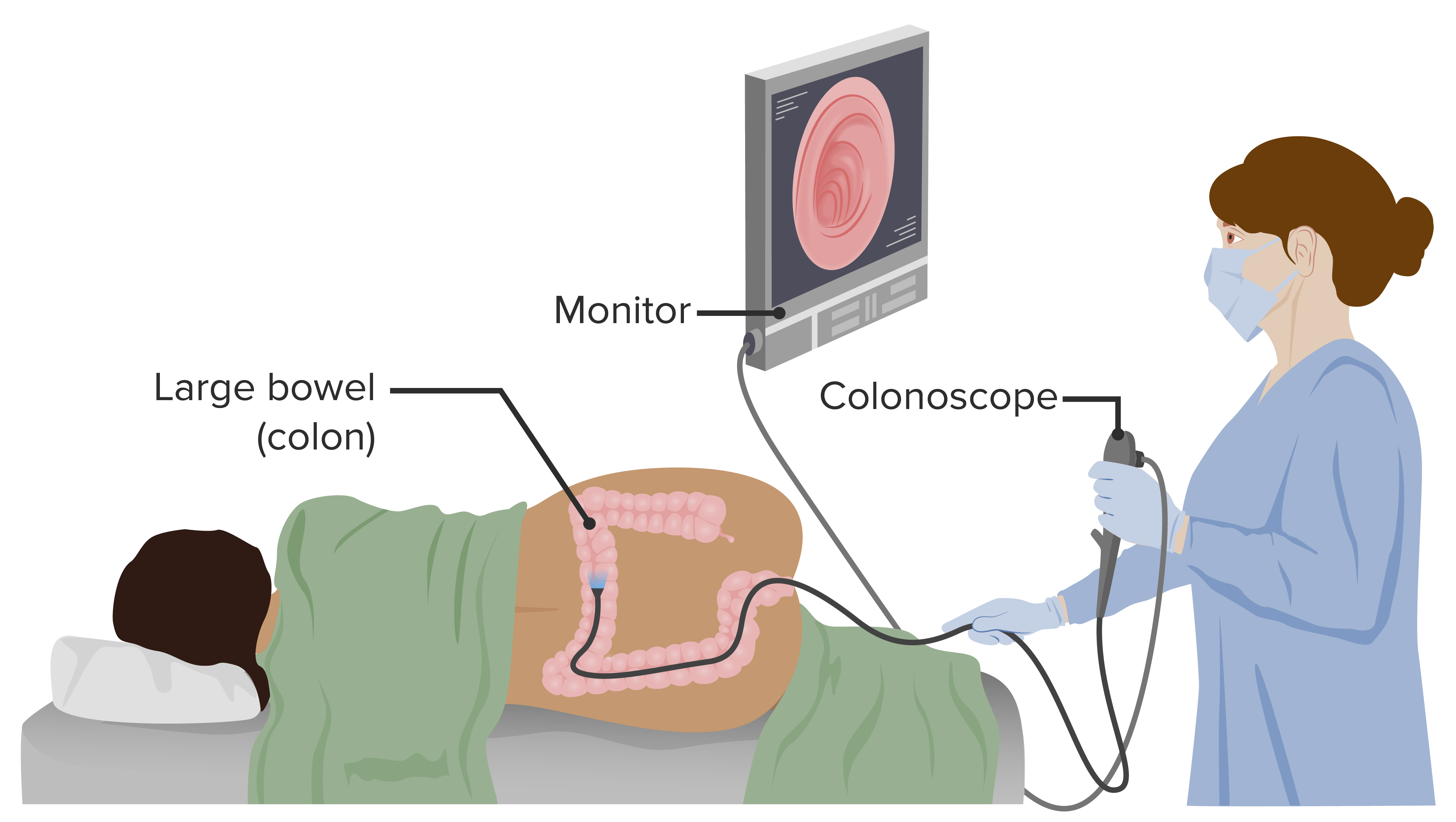
Colonoscopy is a diagnostic procedure that allows visualization of the rectum, colon, and a portion of the terminal ileum. Colonoscopy also has a therapeutic role, allowing biopsy of found lesions.
Image by Lecturio.For an average-risk individual, screening Screening Preoperative Care is initiated at 45 years of age.[6-11]
Note on post-colonoscopy CRCs (PCCRCs)[8]
Screening Screening Preoperative Care Encounter Codes:
These ICD-10 codes ICD-10 Codes Colorectal Cancer Screening (Clinical) are used to specify that a visit’s purpose is for colorectal cancer Colorectal cancer Colorectal cancer (CRC) is the 2nd leading cause of cancer-related deaths in the United States. Colorectal cancer is a heterogeneous disease that arises from genetic and epigenetic abnormalities, with influence from environmental factors. Colorectal Cancer screening Screening Preoperative Care, which is essential for insurance coverage of procedures like a screening Screening Preoperative Care colonoscopy Colonoscopy Endoscopic examination, therapy or surgery of the luminal surface of the colon. Colorectal Cancer Screening.
| Coding System | Code | Description |
|---|---|---|
| ICD-10-CM | Z12.11 | Encounter for screening Screening Preoperative Care for malignant neoplasm of colon Colon The large intestines constitute the last portion of the digestive system. The large intestine consists of the cecum, appendix, colon (with ascending, transverse, descending, and sigmoid segments), rectum, and anal canal. The primary function of the colon is to remove water and compact the stool prior to expulsion from the body via the rectum and anal canal. Colon, Cecum, and Appendix: Anatomy |
| ICD-10-CM | Z12.12 | Encounter for screening Screening Preoperative Care for malignant neoplasm of rectum Rectum The rectum and anal canal are the most terminal parts of the lower GI tract/large intestine that form a functional unit and control defecation. Fecal continence is maintained by several important anatomic structures including rectal folds, anal valves, the sling-like puborectalis muscle, and internal and external anal sphincters. Rectum and Anal Canal: Anatomy |
Screening Screening Preoperative Care & Diagnostic Procedures:
These codes represent the various methods for colorectal cancer Colorectal cancer Colorectal cancer (CRC) is the 2nd leading cause of cancer-related deaths in the United States. Colorectal cancer is a heterogeneous disease that arises from genetic and epigenetic abnormalities, with influence from environmental factors. Colorectal Cancer screening Screening Preoperative Care, including a screening Screening Preoperative Care colonoscopy Colonoscopy Endoscopic examination, therapy or surgery of the luminal surface of the colon. Colorectal Cancer Screening (the gold standard), a stool-based fecal occult blood test Fecal occult blood test Colorectal Cancer (FOBT), and a stool DNA test Stool DNA test Stool-based composite of tests including molecular assays testing for DNA (KRAS) mutations, gene amplification technique testing for methylation biomarkers, FIT Colorectal Cancer Screening.
| Coding System | Code | Description |
|---|---|---|
| HCPCS | G0121 | Colorectal cancer Colorectal cancer Colorectal cancer (CRC) is the 2nd leading cause of cancer-related deaths in the United States. Colorectal cancer is a heterogeneous disease that arises from genetic and epigenetic abnormalities, with influence from environmental factors. Colorectal Cancer screening Screening Preoperative Care; colonoscopy Colonoscopy Endoscopic examination, therapy or surgery of the luminal surface of the colon. Colorectal Cancer Screening on individual not meeting criteria for high risk |
| CPT | 82270 | Blood, occult, by peroxidase activity (eg, guaiac), qualitative; feces, 1-3 simultaneous determinations |
| CPT | 81528 | Oncology (colorectal) screening Screening Preoperative Care, quantitative real-time target and signal amplification of 10 DNA DNA A deoxyribonucleotide polymer that is the primary genetic material of all cells. Eukaryotic and prokaryotic organisms normally contain DNA in a double-stranded state, yet several important biological processes transiently involve single-stranded regions. DNA, which consists of a polysugar-phosphate backbone possessing projections of purines (adenine and guanine) and pyrimidines (thymine and cytosine), forms a double helix that is held together by hydrogen bonds between these purines and pyrimidines (adenine to thymine and guanine to cytosine). DNA Types and Structure markers and fecal hemoglobin |
Abnormal Findings Codes:
These codes are used to document findings from a screening Screening Preoperative Care, such as the discovery of a colon Colon The large intestines constitute the last portion of the digestive system. The large intestine consists of the cecum, appendix, colon (with ascending, transverse, descending, and sigmoid segments), rectum, and anal canal. The primary function of the colon is to remove water and compact the stool prior to expulsion from the body via the rectum and anal canal. Colon, Cecum, and Appendix: Anatomy polyp (a precursor to cancer) or an established malignant neoplasm of the colon Colon The large intestines constitute the last portion of the digestive system. The large intestine consists of the cecum, appendix, colon (with ascending, transverse, descending, and sigmoid segments), rectum, and anal canal. The primary function of the colon is to remove water and compact the stool prior to expulsion from the body via the rectum and anal canal. Colon, Cecum, and Appendix: Anatomy.
| Coding System | Code | Description |
|---|---|---|
| ICD-10-CM | K63.5 | Polyp of colon Colon The large intestines constitute the last portion of the digestive system. The large intestine consists of the cecum, appendix, colon (with ascending, transverse, descending, and sigmoid segments), rectum, and anal canal. The primary function of the colon is to remove water and compact the stool prior to expulsion from the body via the rectum and anal canal. Colon, Cecum, and Appendix: Anatomy |
| ICD-10-CM | C18.9 | Malignant neoplasm of colon Colon The large intestines constitute the last portion of the digestive system. The large intestine consists of the cecum, appendix, colon (with ascending, transverse, descending, and sigmoid segments), rectum, and anal canal. The primary function of the colon is to remove water and compact the stool prior to expulsion from the body via the rectum and anal canal. Colon, Cecum, and Appendix: Anatomy, unspecified |
Follow-up Procedures:
This CPT code is for a colonoscopy Colonoscopy Endoscopic examination, therapy or surgery of the luminal surface of the colon. Colorectal Cancer Screening that includes the removal of a polyp or tumor Tumor Inflammation. When a screening Screening Preoperative Care colonoscopy Colonoscopy Endoscopic examination, therapy or surgery of the luminal surface of the colon. Colorectal Cancer Screening (G-code) becomes diagnostic/therapeutic, this CPT code is used for billing.
| Coding System | Code | Description |
|---|---|---|
| CPT | 45385 | Colonoscopy Colonoscopy Endoscopic examination, therapy or surgery of the luminal surface of the colon. Colorectal Cancer Screening, flexible; with removal of tumor Tumor Inflammation(s), polyp(s), or other lesion(s) by snare technique |