Carbon monoxide Carbon monoxide Carbon monoxide (CO). A poisonous colorless, odorless, tasteless gas. It combines with hemoglobin to form carboxyhemoglobin, which has no oxygen carrying capacity. The resultant oxygen deprivation causes headache, dizziness, decreased pulse and respiratory rates, unconsciousness, and death. Carbon Monoxide Poisoning (CO) is an odorless, colorless, tasteless, nonirritating gas formed by hydrocarbon combustion (e.g., fires, car exhaust, gas heaters). Carbon monoxide Carbon monoxide Carbon monoxide (CO). A poisonous colorless, odorless, tasteless gas. It combines with hemoglobin to form carboxyhemoglobin, which has no oxygen carrying capacity. The resultant oxygen deprivation causes headache, dizziness, decreased pulse and respiratory rates, unconsciousness, and death. Carbon Monoxide Poisoning has a higher affinity for hemoglobin than oxygen, forming carboxyhemoglobin Carboxyhemoglobin Carbon Monoxide Poisoning (COHb). Increased levels of COHb lead to tissue hypoxia Hypoxia Sub-optimal oxygen levels in the ambient air of living organisms. Ischemic Cell Damage and brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification damage. Symptoms of CO poisoning CO poisoning Carbon monoxide (CO) is an odorless, colorless, tasteless, nonirritating gas formed by hydrocarbon combustion (e.g., fires, car exhaust, gas heaters). Carbon monoxide has a higher affinity to hemoglobin than oxygen, forming carboxyhemoglobin (COHb). Increased levels of COHb lead to tissue hypoxia and brain damage. Carbon Monoxide Poisoning include headache Headache The symptom of pain in the cranial region. It may be an isolated benign occurrence or manifestation of a wide variety of headache disorders. Brain Abscess, nausea Nausea An unpleasant sensation in the stomach usually accompanied by the urge to vomit. Common causes are early pregnancy, sea and motion sickness, emotional stress, intense pain, food poisoning, and various enteroviruses. Antiemetics, weakness, chest pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways, shortness of breath Shortness of breath Dyspnea is the subjective sensation of breathing discomfort. Dyspnea is a normal manifestation of heavy physical or psychological exertion, but also may be caused by underlying conditions (both pulmonary and extrapulmonary). Dyspnea, seizures Seizures A seizure is abnormal electrical activity of the neurons in the cerebral cortex that can manifest in numerous ways depending on the region of the brain affected. Seizures consist of a sudden imbalance that occurs between the excitatory and inhibitory signals in cortical neurons, creating a net excitation. The 2 major classes of seizures are focal and generalized. Seizures, coma Coma Coma is defined as a deep state of unarousable unresponsiveness, characterized by a score of 3 points on the GCS. A comatose state can be caused by a multitude of conditions, making the precise epidemiology and prognosis of coma difficult to determine. Coma, and even death. Oxygen therapy is key to the management of CO poisoning CO poisoning Carbon monoxide (CO) is an odorless, colorless, tasteless, nonirritating gas formed by hydrocarbon combustion (e.g., fires, car exhaust, gas heaters). Carbon monoxide has a higher affinity to hemoglobin than oxygen, forming carboxyhemoglobin (COHb). Increased levels of COHb lead to tissue hypoxia and brain damage. Carbon Monoxide Poisoning.
Last updated: Dec 15, 2025
The symptoms of CO poisoning CO poisoning Carbon monoxide (CO) is an odorless, colorless, tasteless, nonirritating gas formed by hydrocarbon combustion (e.g., fires, car exhaust, gas heaters). Carbon monoxide has a higher affinity to hemoglobin than oxygen, forming carboxyhemoglobin (COHb). Increased levels of COHb lead to tissue hypoxia and brain damage. Carbon Monoxide Poisoning are varied and nonspecific.
The severity of the clinical presentation of CO poisoning CO poisoning Carbon monoxide (CO) is an odorless, colorless, tasteless, nonirritating gas formed by hydrocarbon combustion (e.g., fires, car exhaust, gas heaters). Carbon monoxide has a higher affinity to hemoglobin than oxygen, forming carboxyhemoglobin (COHb). Increased levels of COHb lead to tissue hypoxia and brain damage. Carbon Monoxide Poisoning depends on the amount of CO in the inhaled air, the duration of the exposure, and the general state of health of the affected individual.
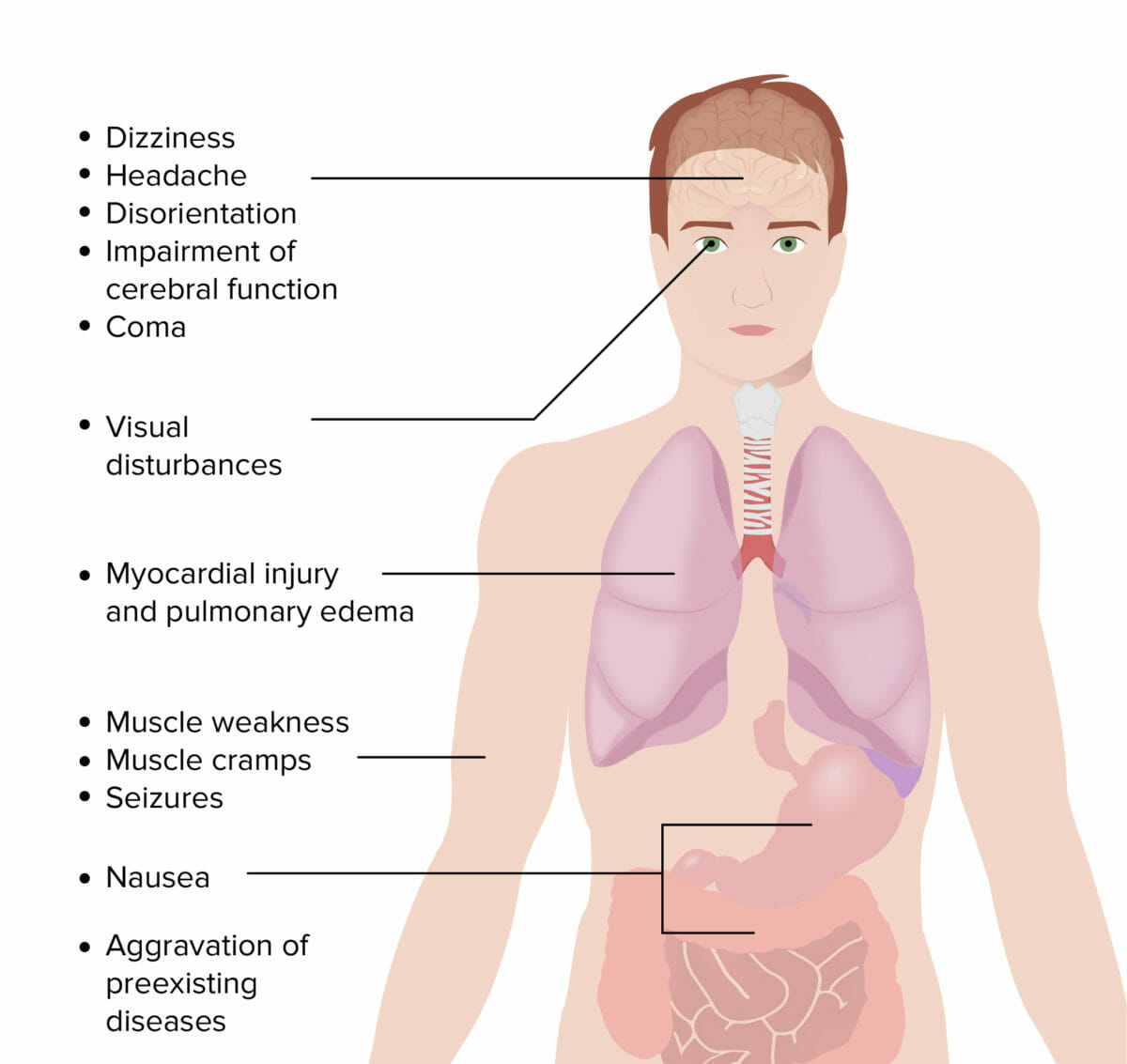
Symptoms of carbon monoxide poisoning
Image by Lecturio.Management may vary based on practice location. The following information is based on US and UK guidelines.[3,5–7,9]
Oxygen therapy
Hyperbaric oxygen Hyperbaric oxygen The therapeutic intermittent administration of oxygen in a chamber at greater than sea-level atmospheric pressures (three atmospheres). It is considered effective treatment for air and gas embolisms, smoke inhalation, acute carbon monoxide poisoning, caisson disease, clostridial gangrene, etc. The list of treatment modalities includes stroke. Decompression Sickness (HBO) for certain conditions[3,4,6]
Additional considerations and follow-up[7,9]
Diagnosis Codes:
These codes are used to document carbon monoxide Carbon monoxide Carbon monoxide (CO). A poisonous colorless, odorless, tasteless gas. It combines with hemoglobin to form carboxyhemoglobin, which has no oxygen carrying capacity. The resultant oxygen deprivation causes headache, dizziness, decreased pulse and respiratory rates, unconsciousness, and death. Carbon Monoxide Poisoning (CO) poisoning. It is crucial to specify the intent (e.g., accidental) and the encounter type, as this is an acute toxic effect.
| Coding System | Code | Description |
|---|---|---|
| ICD-10-CM | T58.91XA | Toxic effect of carbon monoxide Carbon monoxide Carbon monoxide (CO). A poisonous colorless, odorless, tasteless gas. It combines with hemoglobin to form carboxyhemoglobin, which has no oxygen carrying capacity. The resultant oxygen deprivation causes headache, dizziness, decreased pulse and respiratory rates, unconsciousness, and death. Carbon Monoxide Poisoning from unspecified source, accidental (unintentional), initial encounter |
| SNOMED CT | 38914008 | Carbon monoxide Carbon monoxide Carbon monoxide (CO). A poisonous colorless, odorless, tasteless gas. It combines with hemoglobin to form carboxyhemoglobin, which has no oxygen carrying capacity. The resultant oxygen deprivation causes headache, dizziness, decreased pulse and respiratory rates, unconsciousness, and death. Carbon Monoxide Poisoning poisoning (disorder) |
Evaluation & Workup:
This CPT code is for measuring the carboxyhemoglobin Carboxyhemoglobin Carbon Monoxide Poisoning level in the blood, which is the definitive test to confirm the diagnosis and quantify the severity of CO poisoning CO poisoning Carbon monoxide (CO) is an odorless, colorless, tasteless, nonirritating gas formed by hydrocarbon combustion (e.g., fires, car exhaust, gas heaters). Carbon monoxide has a higher affinity to hemoglobin than oxygen, forming carboxyhemoglobin (COHb). Increased levels of COHb lead to tissue hypoxia and brain damage. Carbon Monoxide Poisoning.
| Coding System | Code | Description |
|---|---|---|
| CPT | 82375 | Carboxyhemoglobin Carboxyhemoglobin Carbon Monoxide Poisoning; quantitative |
| CPT | 93000 | Electrocardiogram Electrocardiogram An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG), routine ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG) with at least 12 leads |
Procedures & Interventions:
The primary treatment is oxygen therapy. This code is for hyperbaric oxygen Hyperbaric oxygen The therapeutic intermittent administration of oxygen in a chamber at greater than sea-level atmospheric pressures (three atmospheres). It is considered effective treatment for air and gas embolisms, smoke inhalation, acute carbon monoxide poisoning, caisson disease, clostridial gangrene, etc. The list of treatment modalities includes stroke. Decompression Sickness (HBO) therapy, a specialized treatment used for severe cases of CO poisoning CO poisoning Carbon monoxide (CO) is an odorless, colorless, tasteless, nonirritating gas formed by hydrocarbon combustion (e.g., fires, car exhaust, gas heaters). Carbon monoxide has a higher affinity to hemoglobin than oxygen, forming carboxyhemoglobin (COHb). Increased levels of COHb lead to tissue hypoxia and brain damage. Carbon Monoxide Poisoning to accelerate the elimination Elimination The initial damage and destruction of tumor cells by innate and adaptive immunity. Completion of the phase means no cancer growth. Cancer Immunotherapy of CO from the body.
| Coding System | Code | Description |
|---|---|---|
| CPT | 99183 | Physician or other qualified health care professional attendance and supervision of hyperbaric oxygen Hyperbaric oxygen The therapeutic intermittent administration of oxygen in a chamber at greater than sea-level atmospheric pressures (three atmospheres). It is considered effective treatment for air and gas embolisms, smoke inhalation, acute carbon monoxide poisoning, caisson disease, clostridial gangrene, etc. The list of treatment modalities includes stroke. Decompression Sickness therapy |
Complications:
These codes document the severe organ damage that can result from CO-induced hypoxia Hypoxia Sub-optimal oxygen levels in the ambient air of living organisms. Ischemic Cell Damage, including myocardial injury (heart damage) and delayed or permanent neurologic damage like anoxic brain injury Anoxic Brain Injury Persistent Vegetative State.
| Coding System | Code | Description |
|---|---|---|
| ICD-10-CM | I5A | Non-ischemic myocardial injury (acute) (chronic) |
| ICD-10-CM | G93.1 | Anoxic brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification damage, not elsewhere classified |