Benign prostatic hyperplasia (BPH) is a condition indicating an increase in the number of stromal and epithelial cells within the prostate gland (transition zone). Benign prostatic hyperplasia is common in men > 50 years of age and may greatly affect their quality of life. The development of BPH involves modifiable and non-modifiable risk factors, which lead to anatomic obstruction and downstream effects on other organ systems. Clinically, patients present with a combination of obstructive and bladder storage symptoms. Diagnosis is made by determining the severity of voiding symptoms through a variety of non-invasive (voiding diary, history, physical examination) and invasive (cystoscopy, urodynamics, transrectal ultrasound imaging) tools. Treatment is multimodal with medical and surgical components (prostatectomy) utilized in combination.
Last updated: Sep 10, 2025
Benign Benign Fibroadenoma prostatic hyperplasia Hyperplasia An increase in the number of cells in a tissue or organ without tumor formation. It differs from hypertrophy, which is an increase in bulk without an increase in the number of cells. Cellular Adaptation ( BPH BPH Benign prostatic hyperplasia (bph) is a condition indicating an increase in the number of stromal and epithelial cells within the prostate gland (transition zone). Benign prostatic hyperplasia is common in men > 50 years of age and may greatly affect their quality of life. Benign Prostatic Hyperplasia) is a histologic diagnosis with an increase in the total number of stromal and epithelial cells within the transition zone Transition Zone Pediatric Gastrointestinal Abnormalities of the prostate Prostate The prostate is a gland in the male reproductive system. The gland surrounds the bladder neck and a portion of the urethra. The prostate is an exocrine gland that produces a weakly acidic secretion, which accounts for roughly 20% of the seminal fluid. gland.
The overall size of the prostate Prostate The prostate is a gland in the male reproductive system. The gland surrounds the bladder neck and a portion of the urethra. The prostate is an exocrine gland that produces a weakly acidic secretion, which accounts for roughly 20% of the seminal fluid. gland does not correlate with the degree of symptoms.
Benign Benign Fibroadenoma prostatic hyperplasia Hyperplasia An increase in the number of cells in a tissue or organ without tumor formation. It differs from hypertrophy, which is an increase in bulk without an increase in the number of cells. Cellular Adaptation occurs with bladder outlet obstruction Bladder Outlet Obstruction Benign Prostatic Hyperplasia ( BOO BOO Benign Prostatic Hyperplasia), leading to lower urinary tract Urinary tract The urinary tract is located in the abdomen and pelvis and consists of the kidneys, ureters, urinary bladder, and urethra. The structures permit the excretion of urine from the body. Urine flows from the kidneys through the ureters to the urinary bladder and out through the urethra. Urinary Tract: Anatomy symptoms (LUTS), which can greatly affect quality Quality Activities and programs intended to assure or improve the quality of care in either a defined medical setting or a program. The concept includes the assessment or evaluation of the quality of care; identification of problems or shortcomings in the delivery of care; designing activities to overcome these deficiencies; and follow-up monitoring to ensure effectiveness of corrective steps. Quality Measurement and Improvement of life.
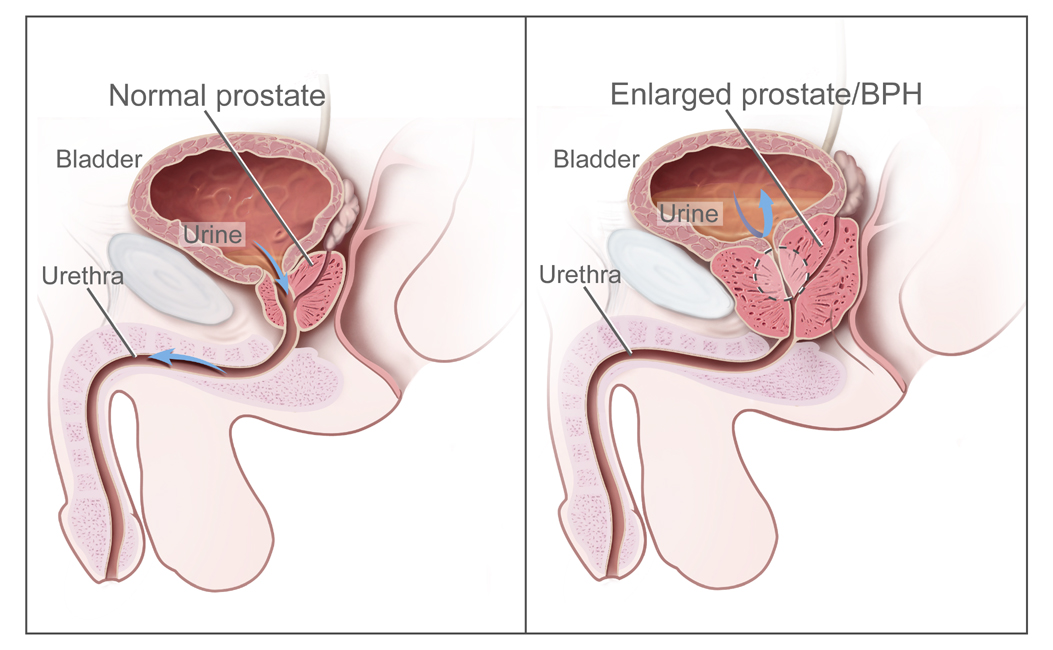
Illustration comparing the normal prostate (left image) and an enlarged prostate or BPH (right image), which is associated with bladder outlet obstruction
Image: “BPH” by National Institutes of Health. License: Public Domain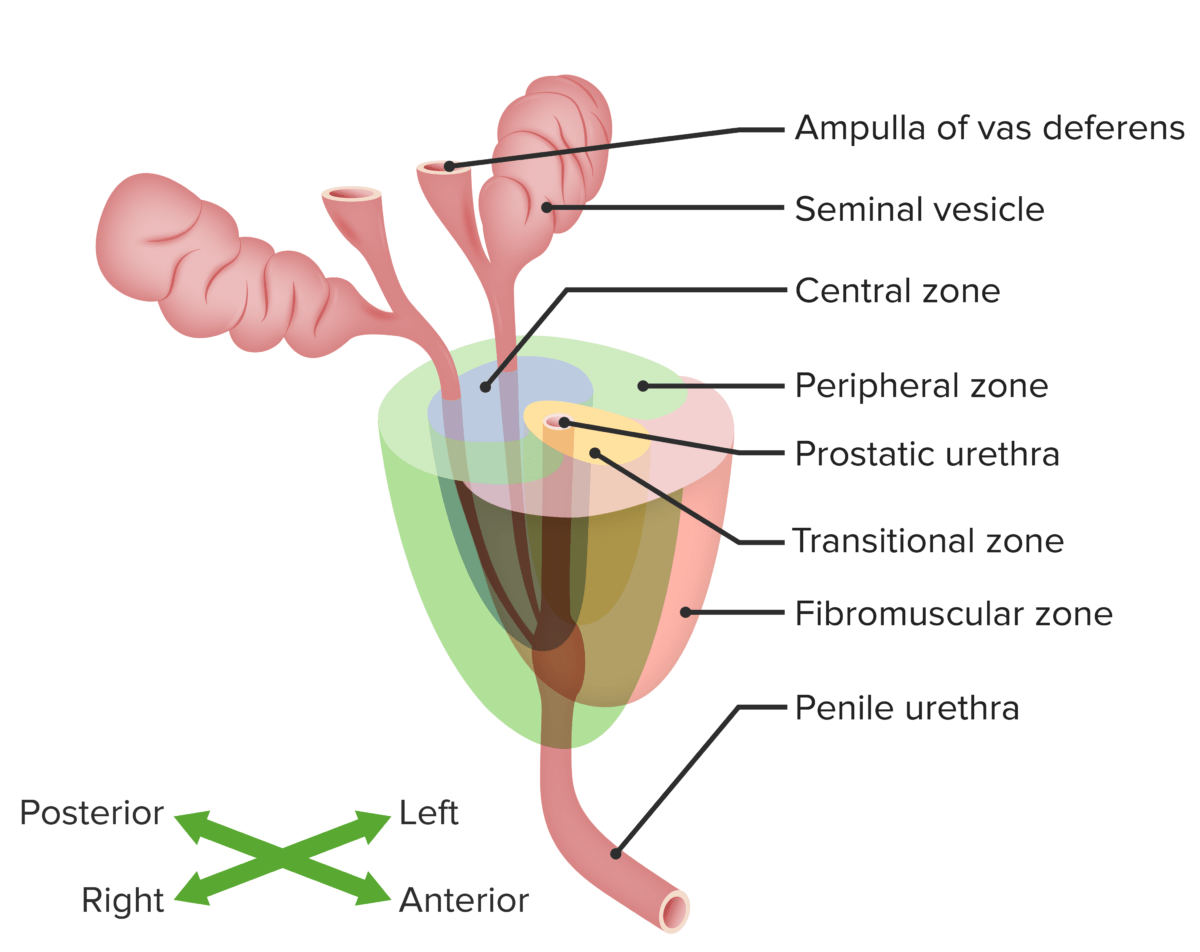
Prostate gland and main prostate zones:
peripheral, transitional and central zones in relation to other structures of the male genitourinary system.
Prevalence Prevalence The total number of cases of a given disease in a specified population at a designated time. It is differentiated from incidence, which refers to the number of new cases in the population at a given time. Measures of Disease Frequency of BPH BPH Benign prostatic hyperplasia (bph) is a condition indicating an increase in the number of stromal and epithelial cells within the prostate gland (transition zone). Benign prostatic hyperplasia is common in men > 50 years of age and may greatly affect their quality of life. Benign Prostatic Hyperplasia increases with age:[2]
Risk factors:[2]
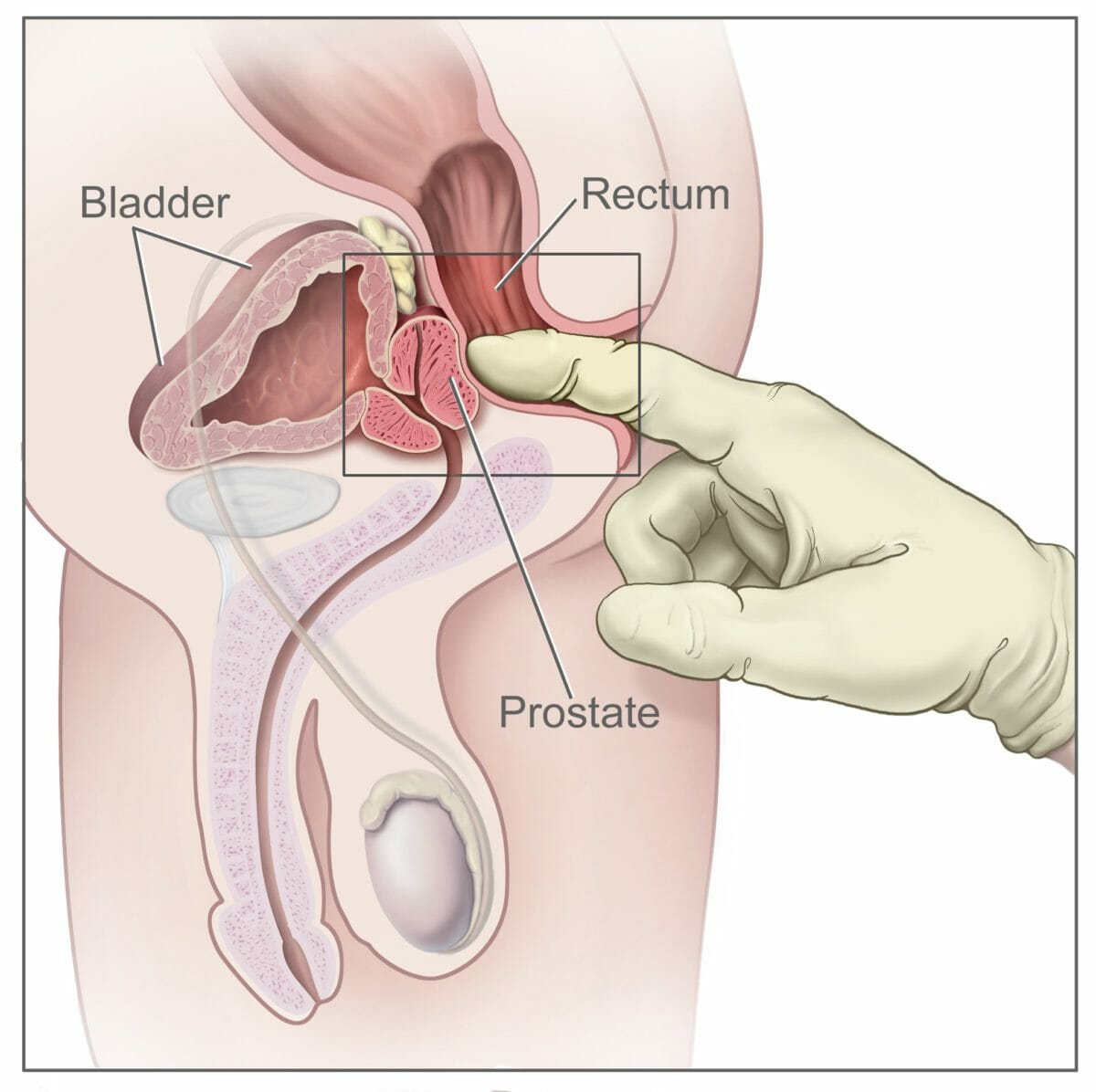
Digital rectal exam (side view of the male reproductive and urinary anatomy, including the prostate, rectum, and bladder):
The doctor inserts a gloved, lubricated finger into the rectum and feels the prostate to check for abnormalities.
Treatment may vary based on locale. The following recommendations are based on the most recent US and European guidelines.
| Pharmacologic class | Medication | Dose | Titration | Directions |
|---|---|---|---|---|
| Alpha-1 adrenergic receptor Receptor Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors blocker | Alfuzosin | 10 mg | None | Once daily immediately following a meal at the same time each day |
| Silodosin | 8 mg | None | Once daily with a meal at the same time each day | |
| Tamsulosin Tamsulosin A sulfonamide derivative and adrenergic alpha-1 receptor antagonist that is used to relieve symptoms of urinary obstruction caused by benign prostatic hyperplasia. Antiadrenergic Drugs immediate-release (IR) | 0.4 mg | None | Once daily approximately 30 minutes after a meal at the same time each day; 0.8 mg dose may be administered as 0.4 mg twice daily | |
| 0.8 mg | Inadequate response after 2–4 weeks | |||
| Tamsulosin Tamsulosin A sulfonamide derivative and adrenergic alpha-1 receptor antagonist that is used to relieve symptoms of urinary obstruction caused by benign prostatic hyperplasia. Antiadrenergic Drugs extended-release (ER) | 0.4 mg | None | Once daily with a meal at the same time each day; maximum, 0.4 mg once daily | |
| Doxazosin Doxazosin A prazosin-related compound that is a selective alpha-1-adrenergic blocker. Antiadrenergic Drugs IR | 1 mg | Days 1–3 | Titration reduces orthostatic effects; once daily at bedtime | |
| 2 mg | Days 4–14 | |||
| 4 mg | Weeks 2–6 | |||
| 8 mg | Week 7 and beyond | |||
| Doxazosin Doxazosin A prazosin-related compound that is a selective alpha-1-adrenergic blocker. Antiadrenergic Drugs ER | 4 mg | Days 1–21 | Once daily with AM meal | |
| 8 mg | Week 4 and beyond | |||
| Terazosin Terazosin Antiadrenergic Drugs | 1 mg | Days 1–3 | Once daily at bedtime | |
| 2 mg | Days 4–14 | |||
| 5 mg | Weeks 2–6 | |||
| 10 mg | Week 7 and beyond | |||
| 20 mg | Inadequate response after 4–6 weeks of 10 mg/day | |||
| PDE-5 | Tadalafil Tadalafil A carboline derivative and phosphodiesterase 5 inhibitor that is used primarily to treat erectile dysfunction; benign prostatic hyperplasia and primary pulmonary hypertension. Phosphodiesterase Inhibitors | 5 mg | None | Once daily by mouth; maximum, 5 mg daily |
| 5-ARIs | Finasteride Finasteride An orally active 3-oxo-5-alpha-steroid 4-dehydrogenase inhibitor. It is used as a surgical alternative for treatment of benign prostatic hyperplasia. Androgens and Antiandrogens | 5 mg | None | Once daily by mouth; maximum, 5 mg daily |
| Dutasteride Dutasteride A 5-alpha-reductase inhibitor that is reported to inhibit both type-1 and type 2 isoforms of the enzyme and is used to treat benign prostatic hyperplasia. Androgens and Antiandrogens | 0.5 mg | None | Once daily by mouth; maximum 0.5 mg daily | |
| Beta-3 adrenergic agonists Adrenergic agonists Sympathomimetic drugs, also known as adrenergic agonists, mimic the action of the stimulators (î±, β, or dopamine receptors) of the sympathetic autonomic nervous system. Sympathomimetic drugs are classified based on the type of receptors the drugs act on (some agents act on several receptors but 1 is predominate). Sympathomimetic Drugs | Mirabegron | 25 mg | May increase after 4 weeks of therapy, if needed | Once daily by mouth; maximum, 50 mg daily |
| Vibegron | 75 mg | None | Once daily by mouth; maximum, 75 mg daily | |
| Anticholinergic Anticholinergic Anticholinergic drugs block the effect of the neurotransmitter acetylcholine at the muscarinic receptors in the central and peripheral nervous systems. Anticholinergic agents inhibit the parasympathetic nervous system, resulting in effects on the smooth muscle in the respiratory tract, vascular system, urinary tract, GI tract, and pupils of the eyes. Anticholinergic Drugs agents | Fesoterodine Fesoterodine Anticholinergic Drugs | 4 mg | May increase after 2 weeks of therapy if needed | Once daily by mouth; maximum, 8 mg daily |
| Tolterodine Tolterodine An antimuscarinic agent selective for the muscarinic receptors of the bladder that is used in the treatment of urinary incontinence and urinary urge incontinence. Anticholinergic Drugs IR | 1–2 mg | None | Twice daily by mouth; maximum, 2 mg twice daily | |
| Tolterodine Tolterodine An antimuscarinic agent selective for the muscarinic receptors of the bladder that is used in the treatment of urinary incontinence and urinary urge incontinence. Anticholinergic Drugs ER | 2–4 mg daily | Once daily by mouth; maximum, 4 mg once daily | ||
| Oxybutynin Oxybutynin Anticholinergic Drugs IR | 5 mg | May increase dosing frequency up to 4 times/day in 5-mg increments every 1–2 weeks, as needed | Twice daily by mouth; maximum, 5 mg 4 times daily | |
| Oxybutynin Oxybutynin Anticholinergic Drugs ER | 5–10 mg | Once daily by mouth; maximum, 30 mg daily | ||
| Darifenacin Darifenacin Anticholinergic Drugs | 7.5 mg | May increase after ≥ 2 weeks as needed | Once daily by mouth; maximum, 15 mg daily | |
| Solifenacin Solifenacin A quinuclidine and tetrahydroisoquinoline derivative and selective m3 muscarinic antagonist. It is used as a urologic agent in the treatment of urinary incontinence. Anticholinergic Drugs | 5 mg daily | Once daily by mouth; maximum, 10 mg daily | ||
| Trospium IR | 20 mg twice daily | None | Twice daily by mouth (once daily if age > 75 years); maximum, 20 mg twice daily | |
| Trospium ER | 60 mg daily | Once daily by mouth; maximum, 60 mg daily |
Diagnosis Codes:
This code is used to diagnose
Benign
Benign
Fibroadenoma Prostatic
Hyperplasia
Hyperplasia
An increase in the number of cells in a tissue or organ without tumor formation. It differs from hypertrophy, which is an increase in bulk without an increase in the number of cells.
Cellular Adaptation (
BPH
BPH
Benign prostatic hyperplasia (bph) is a condition indicating an increase in the number of stromal and epithelial cells within the prostate gland (transition zone). Benign prostatic hyperplasia is common in men > 50 years of age and may greatly affect their quality of life.
Benign Prostatic Hyperplasia), a non-cancerous enlargement of the
prostate
Prostate
The prostate is a gland in the male reproductive system. The gland surrounds the bladder neck and a portion of the urethra. The prostate is an exocrine gland that produces a weakly acidic secretion, which accounts for roughly 20% of the seminal fluid.
gland that is common in older men and can cause lower
urinary tract
Urinary tract
The urinary tract is located in the abdomen and pelvis and consists of the kidneys, ureters, urinary bladder, and urethra. The structures permit the excretion of urine from the body. Urine flows from the kidneys through the ureters to the urinary bladder and out through the urethra.
Urinary Tract: Anatomy symptoms (LUTS).
| Coding System | Code | Description |
|---|---|---|
| ICD-10-CM | N40.1 | Benign Benign Fibroadenoma prostatic hyperplasia Hyperplasia An increase in the number of cells in a tissue or organ without tumor formation. It differs from hypertrophy, which is an increase in bulk without an increase in the number of cells. Cellular Adaptation with lower urinary tract Urinary tract The urinary tract is located in the abdomen and pelvis and consists of the kidneys, ureters, urinary bladder, and urethra. The structures permit the excretion of urine from the body. Urine flows from the kidneys through the ureters to the urinary bladder and out through the urethra. Urinary Tract: Anatomy symptoms |
| ICD-10-CM | N40.0 | Benign Benign Fibroadenoma prostatic hyperplasia Hyperplasia An increase in the number of cells in a tissue or organ without tumor formation. It differs from hypertrophy, which is an increase in bulk without an increase in the number of cells. Cellular Adaptation without lower urinary tract Urinary tract The urinary tract is located in the abdomen and pelvis and consists of the kidneys, ureters, urinary bladder, and urethra. The structures permit the excretion of urine from the body. Urine flows from the kidneys through the ureters to the urinary bladder and out through the urethra. Urinary Tract: Anatomy symptoms |
Procedures/Interventions:
This code is for a
Transurethral Resection of the Prostate
Transurethral resection of the prostate
Removal of all or part of the prostate, often using a cystoscope and/or resectoscope passed through the urethra.
Benign Prostatic Hyperplasia (
TURP
TURP
Removal of all or part of the prostate, often using a cystoscope and/or resectoscope passed through the urethra.
Benign Prostatic Hyperplasia), a common and effective surgical procedure to relieve the obstruction caused by
BPH
BPH
Benign prostatic hyperplasia (bph) is a condition indicating an increase in the number of stromal and epithelial cells within the prostate gland (transition zone). Benign prostatic hyperplasia is common in men > 50 years of age and may greatly affect their quality of life.
Benign Prostatic Hyperplasia by removing excess
prostate
Prostate
The prostate is a gland in the male reproductive system. The gland surrounds the bladder neck and a portion of the urethra. The prostate is an exocrine gland that produces a weakly acidic secretion, which accounts for roughly 20% of the seminal fluid.
tissue.
| Coding System | Code | Description |
|---|---|---|
| CPT | 52601 | Transurethral electrosurgical resection of prostate Prostate The prostate is a gland in the male reproductive system. The gland surrounds the bladder neck and a portion of the urethra. The prostate is an exocrine gland that produces a weakly acidic secretion, which accounts for roughly 20% of the seminal fluid. , including control of postoperative bleeding, complete |
Medications:
These codes are for the two main classes of medications used to treat
BPH
BPH
Benign prostatic hyperplasia (bph) is a condition indicating an increase in the number of stromal and epithelial cells within the prostate gland (transition zone). Benign prostatic hyperplasia is common in men > 50 years of age and may greatly affect their quality of life.
Benign Prostatic Hyperplasia.
Alpha-blockers
Alpha-blockers
Drugs that bind to but do not activate alpha-adrenergic receptors thereby blocking the actions of endogenous or exogenous adrenergic agonists. Adrenergic alpha-antagonists are used in the treatment of hypertension, vasospasm, peripheral vascular disease, shock, and pheochromocytoma.
Antiadrenergic Drugs like
tamsulosin
Tamsulosin
A sulfonamide derivative and adrenergic alpha-1 receptor antagonist that is used to relieve symptoms of urinary obstruction caused by benign prostatic hyperplasia.
Antiadrenergic Drugs relax the smooth muscle of the
prostate
Prostate
The prostate is a gland in the male reproductive system. The gland surrounds the bladder neck and a portion of the urethra. The prostate is an exocrine gland that produces a weakly acidic secretion, which accounts for roughly 20% of the seminal fluid.
, while 5-alpha-reductase inhibitors like
finasteride
Finasteride
An orally active 3-oxo-5-alpha-steroid 4-dehydrogenase inhibitor. It is used as a surgical alternative for treatment of benign prostatic hyperplasia.
Androgens and Antiandrogens shrink the
prostate
Prostate
The prostate is a gland in the male reproductive system. The gland surrounds the bladder neck and a portion of the urethra. The prostate is an exocrine gland that produces a weakly acidic secretion, which accounts for roughly 20% of the seminal fluid.
over time.
| Coding System | Code | Description |
|---|---|---|
| RxNorm | 41133 | Tamsulosin Tamsulosin A sulfonamide derivative and adrenergic alpha-1 receptor antagonist that is used to relieve symptoms of urinary obstruction caused by benign prostatic hyperplasia. Antiadrenergic Drugs (ingredient) |
| RxNorm | 4419 | Finasteride Finasteride An orally active 3-oxo-5-alpha-steroid 4-dehydrogenase inhibitor. It is used as a surgical alternative for treatment of benign prostatic hyperplasia. Androgens and Antiandrogens (ingredient) |