Aortic dissection occurs due to shearing stress from pulsatile pressure causing a tear in the tunica intima of the aortic wall. This tear allows blood to flow into the media, creating a “false lumen.” Aortic dissection is most commonly caused by uncontrolled hypertension. Complications arise due to partial occlusion of vital branches off the aorta and reduced blood flow to the brain, visceral organs, and extremities. Patients often present with acute, tearing chest or back pain. Computed tomography is the diagnostic modality of choice. All type A dissections (ascending aorta) are a surgical emergency due to the risk of imminent rupture. Type B dissections (descending aorta) can be managed medically with impulse control using beta-blockers and calcium channel blockers. If there is evidence of malperfusion to visceral organs or extremities, aneurysm dilation to > 5 cm, retrograde extension into the ascending aorta, or intractable pain, the patient will need evaluation for endovascular or open repair.
Last updated: Dec 15, 2025
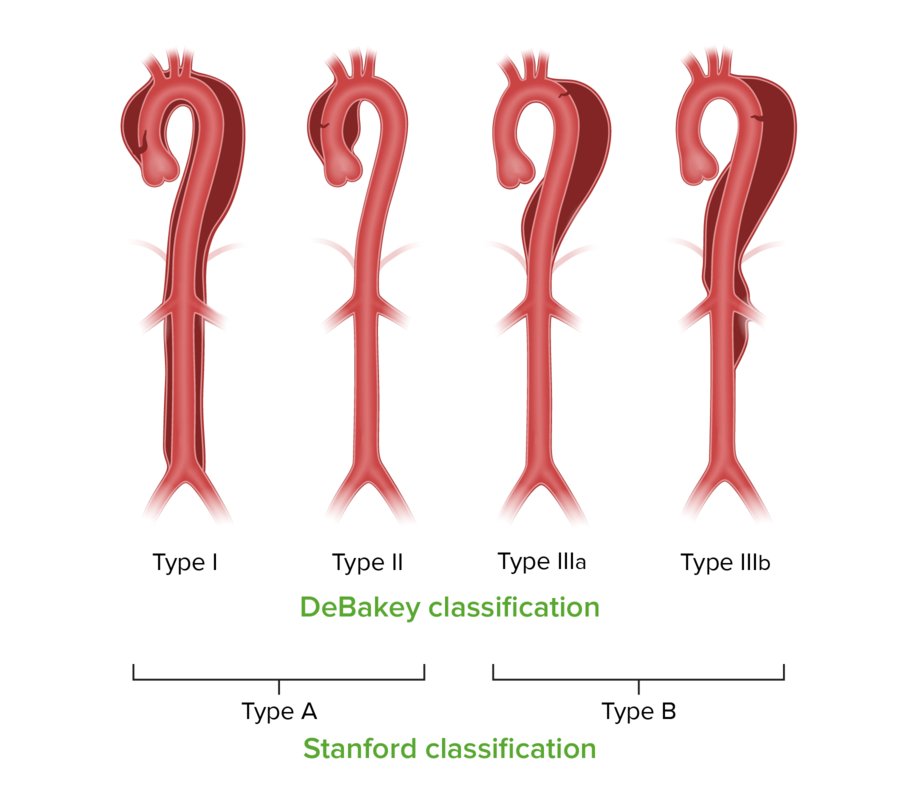
Stanford and DeBakey classifications for aortic dissection
Image by Lecturio.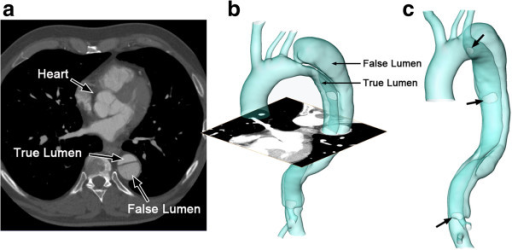
False versus true lumen in aortic dissection
The reconstructed computed tomography (CT) image of an aortic dissection:
1 axial slice of the CT scan (a); reconstructed surface of the aortic dissection (b); positions of the entries along the intimal flap (c; indicated by arrows).
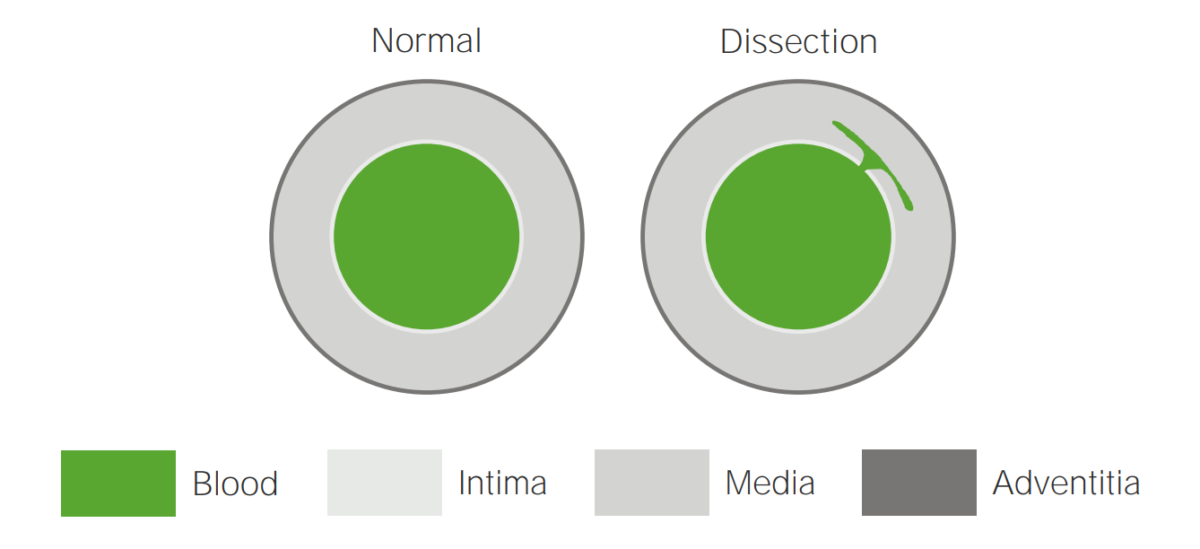
Illustration of an aortic dissection
A tear in the intima allows blood to flow into the media.

Mechanisms of aortic dissections
A tear in the intima, rupture of the vasa vasorum, and ulceration of an atherosclerotic plaque
TL: true lumen
FL: false lumen
Pretest probability Probability Probability is a mathematical tool used to study randomness and provide predictions about the likelihood of something happening. There are several basic rules of probability that can be used to help determine the probability of multiple events happening together, separately, or sequentially. Basics of Probability of aortic dissection Aortic dissection Aortic dissection occurs due to shearing stress from pulsatile pressure causing a tear in the tunica intima of the aortic wall. This tear allows blood to flow into the media, creating a “false lumen.” Aortic dissection is most commonly caused by uncontrolled hypertension. Aortic Dissection may be assessed with the Aortic Dissection Aortic dissection Aortic dissection occurs due to shearing stress from pulsatile pressure causing a tear in the tunica intima of the aortic wall. This tear allows blood to flow into the media, creating a “false lumen.” Aortic dissection is most commonly caused by uncontrolled hypertension. Aortic Dissection Detection-Risk Score (ADD-RS) (calculator)

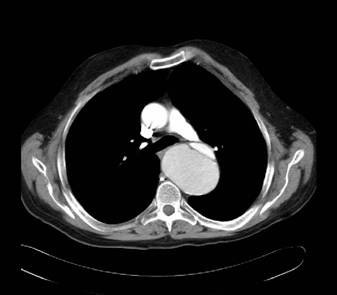
Computed tomography findings in aortic dissection
A: CT scan showing an ascending aortic dissection (gray arrow)
B: CT scan demonstrating an aortic arch dissection (gray arrow)
Computed tomography findings in aortic dissection
CT scan demonstrating the dissection at the level of the aortic valve

Computed tomography findings in aortic dissection
Aortic dissection extending into the left subclavian and axillary arteries, and to the level of bifurcation of the common iliac artery (thick arrows)
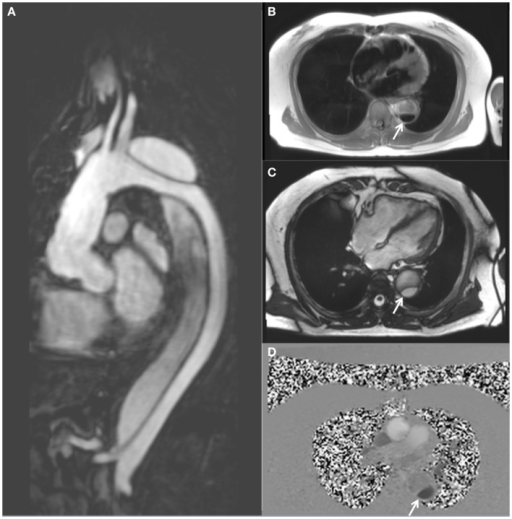
Magnetic resonance imaging demonstrating a descending thoracic aortic dissection:
A: sagittal gadolinium-contrast-enhanced MRA view
B: axial black blood view of the proximal descending thoracic aorta
C: axial true FISP (steady state-free precession) cine view
D: axial phase-contrast view, showing flow patterns in the true and false lumens of the descending aorta (the true lumen is indicated by the white arrow)
Management may vary based on practice location. The following information is based on US and European guidelines.
General:
Analgesia Analgesia Methods of pain relief that may be used with or in place of analgesics. Anesthesiology: History and Basic Concepts:
Anti-impulse therapy (minimize shear stress):[8,12,17]
For hypotension Hypotension Hypotension is defined as low blood pressure, specifically < 90/60 mm Hg, and is most commonly a physiologic response. Hypotension may be mild, serious, or life threatening, depending on the cause. Hypotension (typically type A dissection):
| Class I | Class II | Class III | Class IV | |
|---|---|---|---|---|
| Percentage of blood loss | < 15 | 15–30 | 30–40 | > 40 |
| Pulse rate | Normal | 100–120 | 120–140 | > 140 |
| Blood pressure | Normal | Normal | ↓ | Significantly ↓ |
| Pulse pressure | Normal | ↓ | ↓ | ↓ |
| Respiratory rate Respiratory rate The number of times an organism breathes with the lungs (respiration) per unit time, usually per minute. Pulmonary Examination | 14–20 | 20–30 | 30–40 | > 35 |
| Mental status | Slightly anxious | Mildly anxious | Anxious, confused | Confused, lethargic |
| Urine output (mL/hr) | > 30 | 20–30 | 5–15 | Minimal |
| Fluid resuscitation Resuscitation The restoration to life or consciousness of one apparently dead. . Neonatal Respiratory Distress Syndrome strategy | Crystalloid Crystalloid Isotonic solutions of mineral salts, such as ringer’s lactate and sodium chloride (saline solution), used in fluid therapy to rehydrate blood volume. Intravenous Fluids | Crystalloid Crystalloid Isotonic solutions of mineral salts, such as ringer’s lactate and sodium chloride (saline solution), used in fluid therapy to rehydrate blood volume. Intravenous Fluids, possibly blood products | Type-specific blood | Massive transfusion protocol |
Myocardial infarction Myocardial infarction MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction: ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage of the myocardium Myocardium The muscle tissue of the heart. It is composed of striated, involuntary muscle cells connected to form the contractile pump to generate blood flow. Heart: Anatomy due to partial or complete obstruction of the coronary arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology. Most often due to atherosclerosis Atherosclerosis Atherosclerosis is a common form of arterial disease in which lipid deposition forms a plaque in the blood vessel walls. Atherosclerosis is an incurable disease, for which there are clearly defined risk factors that often can be reduced through a change in lifestyle and behavior of the patient. Atherosclerosis of the coronary arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology. Presentation can mimic a dissection, with acute-onset chest pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways. However, the pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways does not typically radiate to the back and gradually increases in severity, and is usually accompanied by elevated troponins, typical ischemic ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG) changes (ST elevations or depressions), and wall motion abnormalities on transthoracic echo.
Horner’s syndrome: interruption to the sympathetic chain innervating the eye due to compression Compression Blunt Chest Trauma, lesion of the neuron, or stroke. Characterized by a constricted pupil Pupil The pupil is the space within the eye that permits light to project onto the retina. Anatomically located in front of the lens, the pupil’s size is controlled by the surrounding iris. The pupil provides insight into the function of the central and autonomic nervous systems. Pupil: Physiology and Abnormalities ( miosis Miosis Pupil: Physiology and Abnormalities), drooping of the upper eyelid ( ptosis Ptosis Cranial Nerve Palsies), and absence of sweating of the face (anhidrosis). A chest X-ray X-ray Penetrating electromagnetic radiation emitted when the inner orbital electrons of an atom are excited and release radiant energy. X-ray wavelengths range from 1 pm to 10 nm. Hard x-rays are the higher energy, shorter wavelength x-rays. Soft x-rays or grenz rays are less energetic and longer in wavelength. The short wavelength end of the x-ray spectrum overlaps the gamma rays wavelength range. The distinction between gamma rays and x-rays is based on their radiation source. Pulmonary Function Tests should be ordered to evaluate for an apical lung mass Mass Three-dimensional lesion that occupies a space within the breast Imaging of the Breast.
Aortic regurgitation Regurgitation Gastroesophageal Reflux Disease (GERD): insufficiency of the aortic valve Aortic valve The valve between the left ventricle and the ascending aorta which prevents backflow into the left ventricle. Heart: Anatomy, causing the backflow of blood into the left ventricle following systole Systole Period of contraction of the heart, especially of the heart ventricles. Cardiac Cycle when the valve is closed. Characterized by soft, high-pitched, early diastolic, decrescendo murmur heard best at the 3rd intercostal space left of the sternal border. Transthoracic echocardiography Transthoracic Echocardiography Imaging of the Heart and Great Vessels is used to confirm the diagnosis.
Pericardial effusion Pericardial effusion Fluid accumulation within the pericardium. Serous effusions are associated with pericardial diseases. Hemopericardium is associated with trauma. Lipid-containing effusion (chylopericardium) results from leakage of thoracic duct. Severe cases can lead to cardiac tamponade. Pericardial Effusion and Cardiac Tamponade and tamponade Tamponade Pericardial effusion, usually of rapid onset, exceeding ventricular filling pressures and causing collapse of the heart with a markedly reduced cardiac output. Pericarditis: fluid in the pericardial sac, which can cause compression Compression Blunt Chest Trauma of the heart and lead to tamponade Tamponade Pericardial effusion, usually of rapid onset, exceeding ventricular filling pressures and causing collapse of the heart with a markedly reduced cardiac output. Pericarditis physiology. Tamponade Tamponade Pericardial effusion, usually of rapid onset, exceeding ventricular filling pressures and causing collapse of the heart with a markedly reduced cardiac output. Pericarditis physiology prevents the heart from filling, resulting in hemodynamic collapse. Beck’s triad Beck’s triad The triad describes the classic findings in cardiac tamponade: hypotension, jugular venous distension, muffled heart sounds on auscultation. Pericardial Effusion and Cardiac Tamponade of distended neck Neck The part of a human or animal body connecting the head to the rest of the body. Peritonsillar Abscess veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology, hypotension Hypotension Hypotension is defined as low blood pressure, specifically < 90/60 mm Hg, and is most commonly a physiologic response. Hypotension may be mild, serious, or life threatening, depending on the cause. Hypotension, and muffled heart sounds Muffled Heart Sounds Pericardial Effusion and Cardiac Tamponade is often seen on physical exam. Diagnosis is confirmed with transthoracic echocardiography Transthoracic Echocardiography Imaging of the Heart and Great Vessels, and management involves drainage of the pericardium Pericardium A conical fibroserous sac surrounding the heart and the roots of the great vessels (aorta; venae cavae; pulmonary artery). Pericardium consists of two sacs: the outer fibrous pericardium and the inner serous pericardium. The latter consists of an outer parietal layer facing the fibrous pericardium, and an inner visceral layer (epicardium) resting next to the heart, and a pericardial cavity between these two layers. Heart: Anatomy.
Pneumothorax Pneumothorax A pneumothorax is a life-threatening condition in which air collects in the pleural space, causing partial or full collapse of the lung. A pneumothorax can be traumatic or spontaneous. Patients present with a sudden onset of sharp chest pain, dyspnea, and diminished breath sounds on exam. Pneumothorax: a life-threatening condition in which air collects in the pleural space Pleural space The thin serous membrane enveloping the lungs (lung) and lining the thoracic cavity. Pleura consist of two layers, the inner visceral pleura lying next to the pulmonary parenchyma and the outer parietal pleura. Between the two layers is the pleural cavity which contains a thin film of liquid. Pleuritis, causing partial or full collapse of the lung. Pneumothorax Pneumothorax A pneumothorax is a life-threatening condition in which air collects in the pleural space, causing partial or full collapse of the lung. A pneumothorax can be traumatic or spontaneous. Patients present with a sudden onset of sharp chest pain, dyspnea, and diminished breath sounds on exam. Pneumothorax can be traumatic or spontaneous. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship present with a sudden onset of sharp chest pain Sharp Chest Pain Chest Pain, dyspnea Dyspnea Dyspnea is the subjective sensation of breathing discomfort. Dyspnea is a normal manifestation of heavy physical or psychological exertion, but also may be caused by underlying conditions (both pulmonary and extrapulmonary). Dyspnea, and diminished breath sounds on exam. A large or tension pneumothorax Tension Pneumothorax Pneumothorax can result in cardiopulmonary collapse. Diagnosis is made with imaging. Management includes needle decompression Needle Decompression Pneumothorax and chest tube ( thoracostomy Thoracostomy Surgical procedure involving the creation of an opening (stoma) into the chest cavity for drainage; used in the treatment of pleural effusion; pneumothorax; hemothorax; and empyema. Hemothorax) placement.
Pulmonary embolism Pulmonary Embolism Pulmonary embolism (PE) is a potentially fatal condition that occurs as a result of intraluminal obstruction of the main pulmonary artery or its branches. The causative factors include thrombi, air, amniotic fluid, and fat. In PE, gas exchange is impaired due to the decreased return of deoxygenated blood to the lungs. Pulmonary Embolism: obstruction of the pulmonary arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology, most often due to thrombus migration from the deep venous system. Signs and symptoms include pleuritic chest pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways, dyspnea Dyspnea Dyspnea is the subjective sensation of breathing discomfort. Dyspnea is a normal manifestation of heavy physical or psychological exertion, but also may be caused by underlying conditions (both pulmonary and extrapulmonary). Dyspnea, tachypnea Tachypnea Increased respiratory rate. Pulmonary Examination, and tachycardia Tachycardia Abnormally rapid heartbeat, usually with a heart rate above 100 beats per minute for adults. Tachycardia accompanied by disturbance in the cardiac depolarization (cardiac arrhythmia) is called tachyarrhythmia. Sepsis in Children. Severe cases can result in hemodynamic instability or cardiopulmonary arrest Cardiopulmonary arrest Cardiac arrest is the sudden, complete cessation of cardiac output with hemodynamic collapse. Patients present as pulseless, unresponsive, and apneic. Rhythms associated with cardiac arrest are ventricular fibrillation/tachycardia, asystole, or pulseless electrical activity. Cardiac Arrest. A chest CT with angiography Angiography Radiography of blood vessels after injection of a contrast medium. Cardiac Surgery is the primary method of diagnosis. Management includes oxygenation, anticoagulation Anticoagulation Pulmonary Hypertension Drugs, and thrombolytic therapy for unstable patients Unstable Patients Blunt Chest Trauma.
Diagnosis Codes:
These ICD-10 codes ICD-10 Codes Aortic Dissection (Clinical) are critical for classifying an aortic dissection Aortic dissection Aortic dissection occurs due to shearing stress from pulsatile pressure causing a tear in the tunica intima of the aortic wall. This tear allows blood to flow into the media, creating a “false lumen.” Aortic dissection is most commonly caused by uncontrolled hypertension. Aortic Dissection based on its location, which dictates the urgency and type of treatment. Type A dissections involving the ascending aorta Ascending aorta Mediastinum and Great Vessels: Anatomy (I71.01) are surgical emergencies.
| Domain | Code | Description |
|---|---|---|
| ICD-10-CM | I71.01 | Dissection of ascending aorta Ascending aorta Mediastinum and Great Vessels: Anatomy |
| ICD-10-CM | I71.02 | Dissection of aortic arch Aortic arch Mediastinum and Great Vessels: Anatomy |
| ICD-10-CM | I71.03 | Dissection of descending thoracic aorta Aorta The main trunk of the systemic arteries. Mediastinum and Great Vessels: Anatomy |
| SNOMED CT | 399122003 | Aortic dissection Aortic dissection Aortic dissection occurs due to shearing stress from pulsatile pressure causing a tear in the tunica intima of the aortic wall. This tear allows blood to flow into the media, creating a “false lumen.” Aortic dissection is most commonly caused by uncontrolled hypertension. Aortic Dissection (disorder) |
Evaluation & Workup:
These CPT codes are used to order the urgent imaging needed to confirm a diagnosis of aortic dissection Aortic dissection Aortic dissection occurs due to shearing stress from pulsatile pressure causing a tear in the tunica intima of the aortic wall. This tear allows blood to flow into the media, creating a “false lumen.” Aortic dissection is most commonly caused by uncontrolled hypertension. Aortic Dissection, with CT angiography Angiography Radiography of blood vessels after injection of a contrast medium. Cardiac Surgery being the most common and fastest modality.
| Domain | Code | Description |
|---|---|---|
| CPT | 71275 | Computed tomography angiography Angiography Radiography of blood vessels after injection of a contrast medium. Cardiac Surgery, chest (noncoronary), with contrast material |
| CPT | 93312 | Echocardiography Echocardiography Ultrasonic recording of the size, motion, and composition of the heart and surrounding tissues. The standard approach is transthoracic. Tricuspid Valve Atresia (TVA), transesophageal ( TEE TEE Ultrasonic recording of the size, motion, and composition of the heart and surrounding tissues using a transducer placed in the esophagus. Imaging of the Heart and Great Vessels), real-time with image documentation Documentation Systematic organization, storage, retrieval, and dissemination of specialized information, especially of a scientific or technical nature. It often involves authenticating or validating information. Advance Directives |
Procedures/Interventions:
This CPT code is used to bill for the emergency open-heart surgery required to repair a Type A aortic dissection Aortic dissection Aortic dissection occurs due to shearing stress from pulsatile pressure causing a tear in the tunica intima of the aortic wall. This tear allows blood to flow into the media, creating a “false lumen.” Aortic dissection is most commonly caused by uncontrolled hypertension. Aortic Dissection, which involves replacing the damaged portion of the ascending aorta Ascending aorta Mediastinum and Great Vessels: Anatomy with a synthetic graft Graft A piece of living tissue that is surgically transplanted Organ Transplantation.
| Domain | Code | Description |
|---|---|---|
| CPT | 33860 | Ascending aorta Ascending aorta Mediastinum and Great Vessels: Anatomy graft Graft A piece of living tissue that is surgically transplanted Organ Transplantation, with cardiopulmonary bypass |
| CPT | 33880 | Endovascular repair of descending thoracic aorta Aorta The main trunk of the systemic arteries. Mediastinum and Great Vessels: Anatomy (eg, aneurysm Aneurysm An aneurysm is a bulging, weakened area of a blood vessel that causes an abnormal widening of its diameter > 1.5 times the size of the native vessel. Aneurysms occur more often in arteries than in veins and are at risk of dissection and rupture, which can be life-threatening. Thoracic Aortic Aneurysms, dissection) (TEVAR) |
Medications:
These codes are used to prescribe intravenous medications for the immediate medical management of aortic dissection Aortic dissection Aortic dissection occurs due to shearing stress from pulsatile pressure causing a tear in the tunica intima of the aortic wall. This tear allows blood to flow into the media, creating a “false lumen.” Aortic dissection is most commonly caused by uncontrolled hypertension. Aortic Dissection, aimed at aggressively lowering blood pressure and heart rate Heart rate The number of times the heart ventricles contract per unit of time, usually per minute. Cardiac Physiology with drugs like labetalol Labetalol A salicylamide derivative that is a non-cardioselective blocker of beta-adrenergic receptors and alpha-1 adrenergic receptors. Subarachnoid Hemorrhage and nitroprusside Nitroprusside A powerful vasodilator used in emergencies to lower blood pressure or to improve cardiac function. It is also an indicator for free sulfhydryl groups in proteins. Nitrates.
| Domain | Code | Description |
|---|---|---|
| RxNorm | 6135 | Labetalol Labetalol A salicylamide derivative that is a non-cardioselective blocker of beta-adrenergic receptors and alpha-1 adrenergic receptors. Subarachnoid Hemorrhage (ingredient) |
| RxNorm | 3939 | Esmolol Esmolol Antiadrenergic Drugs (ingredient) |
| RxNorm | 7480 | Nitroprusside Nitroprusside A powerful vasodilator used in emergencies to lower blood pressure or to improve cardiac function. It is also an indicator for free sulfhydryl groups in proteins. Nitrates (ingredient) |
| ATC | C07AG | Alpha and beta blocking agents |