Antepartum hemorrhage is defined as vaginal bleeding that occurs after 20 weeks of gestation and is unrelated to labor. The most important causes are placental abruption (most common), placenta previa Placenta Previa Abnormal placentation in which the placenta implants in the lower segment of the uterus (the zone of dilation) and may cover part or all of the opening of the cervix. It is often associated with serious antepartum bleeding and premature labor. Placental Abnormalities (2nd most common), vasa previa, and uterine rupture. Placental abruption and uterine rupture are diagnosed clinically. Placenta previa Placenta Previa Abnormal placentation in which the placenta implants in the lower segment of the uterus (the zone of dilation) and may cover part or all of the opening of the cervix. It is often associated with serious antepartum bleeding and premature labor. Placental Abnormalities and vasa previa are usually diagnosed as part of routine screening Screening Preoperative Care on a midtrimester ultrasound, and digital exams in these women must be avoided. All of these conditions can lead to maternal and/or fetal hemorrhage, necessitating emergency cesarean delivery Cesarean Delivery Cesarean delivery (CD) is the operative delivery of ≥ 1 infants through a surgical incision in the maternal abdomen and uterus. Cesarean deliveries may be indicated for a number of either maternal or fetal reasons, most commonly including fetal intolerance to labor, arrest of labor, a history of prior uterine surgery, fetal malpresentation, and placental abnormalities. Cesarean Delivery (CD) and maternal and/or fetal resuscitation Resuscitation The restoration to life or consciousness of one apparently dead. . Neonatal Respiratory Distress Syndrome.
Last updated: Dec 15, 2025
Antepartum hemorrhage is defined as vaginal bleeding that occurs after 20 weeks of gestation and is unrelated to labor.
| Anatomic location | Causes of antepartum bleeding |
|---|---|
| Placenta Placenta A highly vascularized mammalian fetal-maternal organ and major site of transport of oxygen, nutrients, and fetal waste products. It includes a fetal portion (chorionic villi) derived from trophoblasts and a maternal portion (decidua) derived from the uterine endometrium. The placenta produces an array of steroid, protein and peptide hormones (placental hormones). Placenta, Umbilical Cord, and Amniotic Cavity |
|
| Uterus Uterus The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The uterus has a thick wall made of smooth muscle (the myometrium) and an inner mucosal layer (the endometrium). The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Uterus, Cervix, and Fallopian Tubes: Anatomy | Uterine rupture* |
| Cervix Cervix The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Externally, the cervix is lined by stratified squamous cells; however, the cervical canal is lined by columnar epithelium. Uterus, Cervix, and Fallopian Tubes: Anatomy |
|
| Vagina Vagina The vagina is the female genital canal, extending from the vulva externally to the cervix uteri internally. The structures have sexual, reproductive, and urinary functions and a rich blood supply, mainly arising from the internal iliac artery. Vagina, Vulva, and Pelvic Floor: Anatomy and vulva Vulva The vulva is the external genitalia of the female and includes the mons pubis, labia majora, labia minora, clitoris, vestibule, vestibular bulb, and greater vestibular glands. Vagina, Vulva, and Pelvic Floor: Anatomy |
|
Placental abruption is the complete or partial premature Premature Childbirth before 37 weeks of pregnancy (259 days from the first day of the mother’s last menstrual period, or 245 days after fertilization). Necrotizing Enterocolitis detachment of a normally implanted placenta Placenta A highly vascularized mammalian fetal-maternal organ and major site of transport of oxygen, nutrients, and fetal waste products. It includes a fetal portion (chorionic villi) derived from trophoblasts and a maternal portion (decidua) derived from the uterine endometrium. The placenta produces an array of steroid, protein and peptide hormones (placental hormones). Placenta, Umbilical Cord, and Amniotic Cavity before the birth of the infant.
Clinical relevance:
Bleeding from placental separation may be either external with visible vaginal bleeding (80%), or concealed (blood pools behind the placenta Placenta A highly vascularized mammalian fetal-maternal organ and major site of transport of oxygen, nutrients, and fetal waste products. It includes a fetal portion (chorionic villi) derived from trophoblasts and a maternal portion (decidua) derived from the uterine endometrium. The placenta produces an array of steroid, protein and peptide hormones (placental hormones). Placenta, Umbilical Cord, and Amniotic Cavity) without vaginal bleeding (20%).
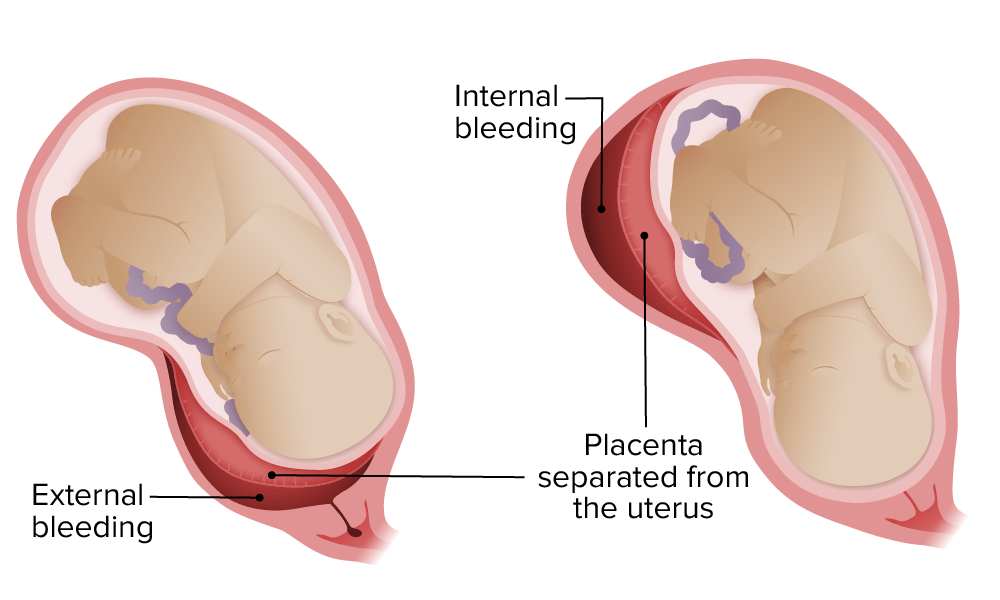
Placental abruption: External versus concealed bleeding
Image by Lecturio.The diagnosis of placental abruption is usually clinical, based on the history, exam, and fetal monitoring Fetal monitoring The primary goals of antepartum testing and monitoring are to assess fetal well-being, identify treatable situations that may cause complications, and evaluate for chromosomal abnormalities. These tests are divided into screening tests (which include cell-free DNA testing, serum analyte testing, and nuchal translucency measurements), and diagnostic tests, which provide a definitive diagnosis of aneuploidy and include chorionic villus sampling (CVS) and amniocentesis. Antepartum Testing and Monitoring.
Definitions:
Clinical relevance:
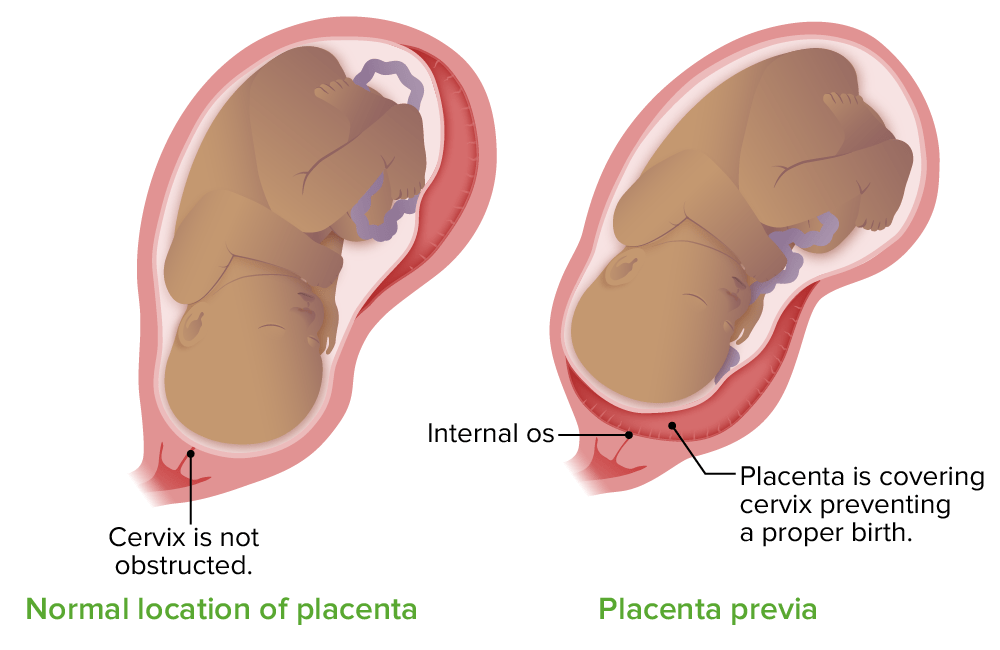
Location of the placenta in placenta previa
Image by Lecturio.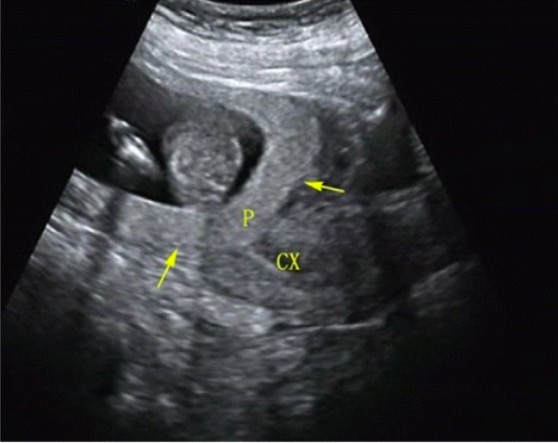
Transabdominal ultrasound showing placenta previa
P = placenta
CX = cervix
Definitions:
Clinical significance:
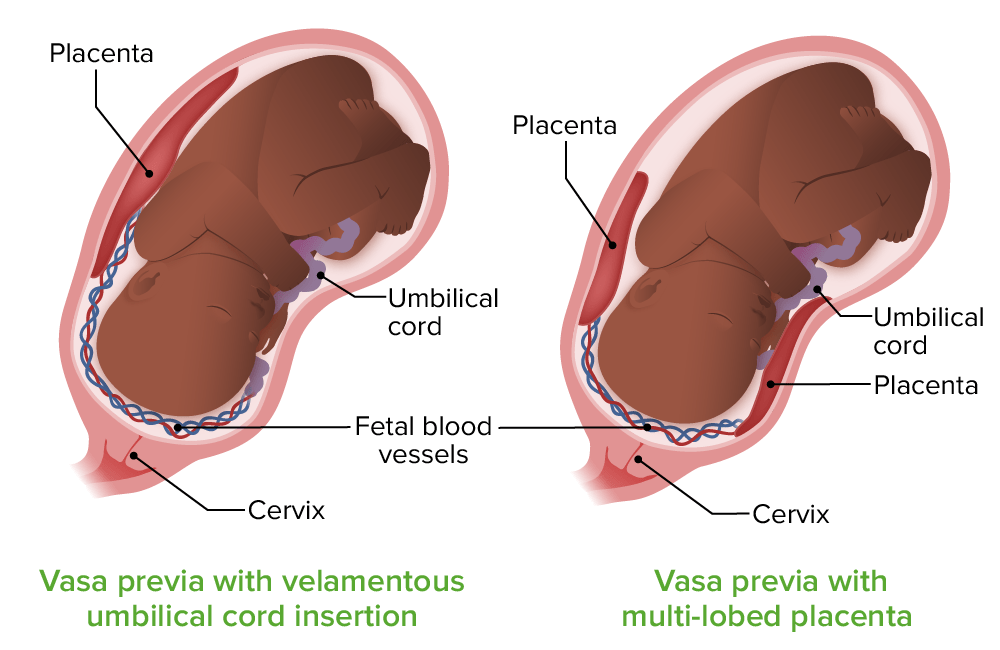
Vasa previa:
On the left, the vessels in the umbilical cord run directly over the internal cervical os (vasa previa) and lack the protective Wharton jelly (velamentous cord insertion). On the right, the vasa previa vessels run to an accessory lobe of the placenta; the vessels also lack Wharton jelly.
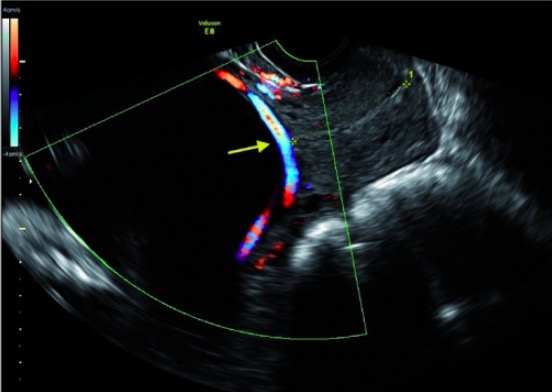
Transvaginal ultrasound showing a vasa previa:
The color Doppler shows blood flowing through the vasa previa vessel over the internal cervical os. The cervical canal is marked with the yellow asterisks on each end.
Uterine rupture is a clinically significant disruption in all layers of the uterus Uterus The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The uterus has a thick wall made of smooth muscle (the myometrium) and an inner mucosal layer (the endometrium). The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Uterus, Cervix, and Fallopian Tubes: Anatomy, usually through a previous uterine scar Scar Dermatologic Examination.
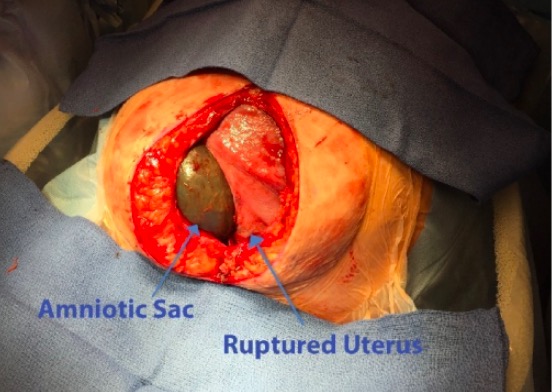
Uterine rupture:
This woman has undergone a laparotomy through a vertical midline incision. Within the abdominal cavity, a bulging amniotic sac is noted through a large defect in the anterior uterine wall.
| Condition | Typical presentation | Important risk factors | Typical management |
|---|---|---|---|
| Placental abruption |
|
|
Emergent delivery |
| Placenta previa Placenta Previa Abnormal placentation in which the placenta implants in the lower segment of the uterus (the zone of dilation) and may cover part or all of the opening of the cervix. It is often associated with serious antepartum bleeding and premature labor. Placental Abnormalities | Painless bleeding OR asymptomatic |
|
|
| Vasa previa | Painless bleeding OR asymptomatic |
|
|
| Uterine rupture |
|
|
|