The heart is a 4-chambered muscular pump Pump ACES and RUSH: Resuscitation Ultrasound Protocols made primarily of cardiac muscle Cardiac muscle The muscle tissue of the heart. It is composed of striated, involuntary muscle cells connected to form the contractile pump to generate blood flow. Muscle Tissue: Histology tissue. The heart is divided into 4 chambers: 2 upper chambers for receiving blood from the great vessels, known as the right and left atria, and 2 stronger lower chambers, known as the right and left ventricles, which pump Pump ACES and RUSH: Resuscitation Ultrasound Protocols blood throughout the body. Blood flows through the heart in 1 direction, moving from the right side of the heart, through the lungs Lungs Lungs are the main organs of the respiratory system. Lungs are paired viscera located in the thoracic cavity and are composed of spongy tissue. The primary function of the lungs is to oxygenate blood and eliminate CO2. Lungs: Anatomy, and then returning to the left side of the heart, where it is pumped out to the rest of the body. As blood moves through the heart, 4 important valves prevent backflow. The heart muscle itself is supplied by the coronary arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology. The heart also has its own conduction system, triggering its own rhythmic contractions.
Last updated: Dec 15, 2025
The heart is a 4-chambered muscular pump Pump ACES and RUSH: Resuscitation Ultrasound Protocols made of cardiac muscle Cardiac muscle The muscle tissue of the heart. It is composed of striated, involuntary muscle cells connected to form the contractile pump to generate blood flow. Muscle Tissue: Histology tissue.

General structure and flow of blood through the heart:
Blue denotes the path of deoxygenated blood, while red indicates the path of oxygenated blood.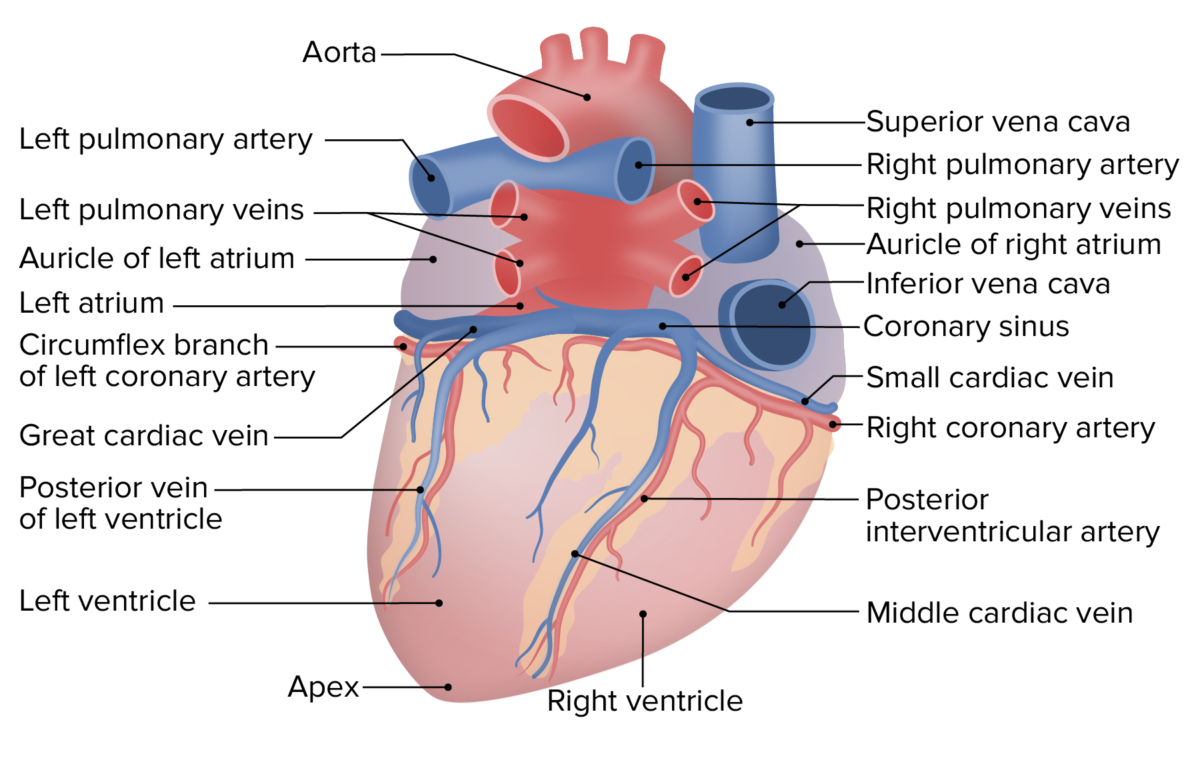
External anatomy of the heart, posterior view
Image by Lecturio.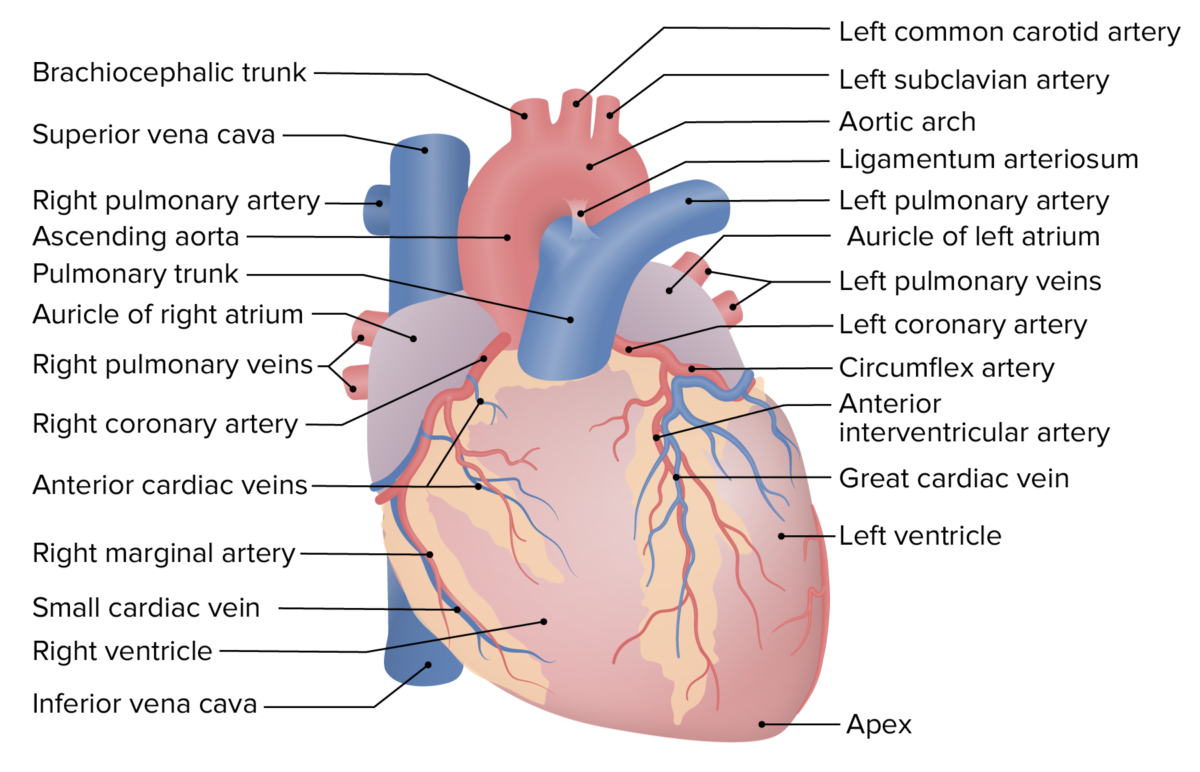
External anatomy of the heart, anterior view
Image by Lecturio.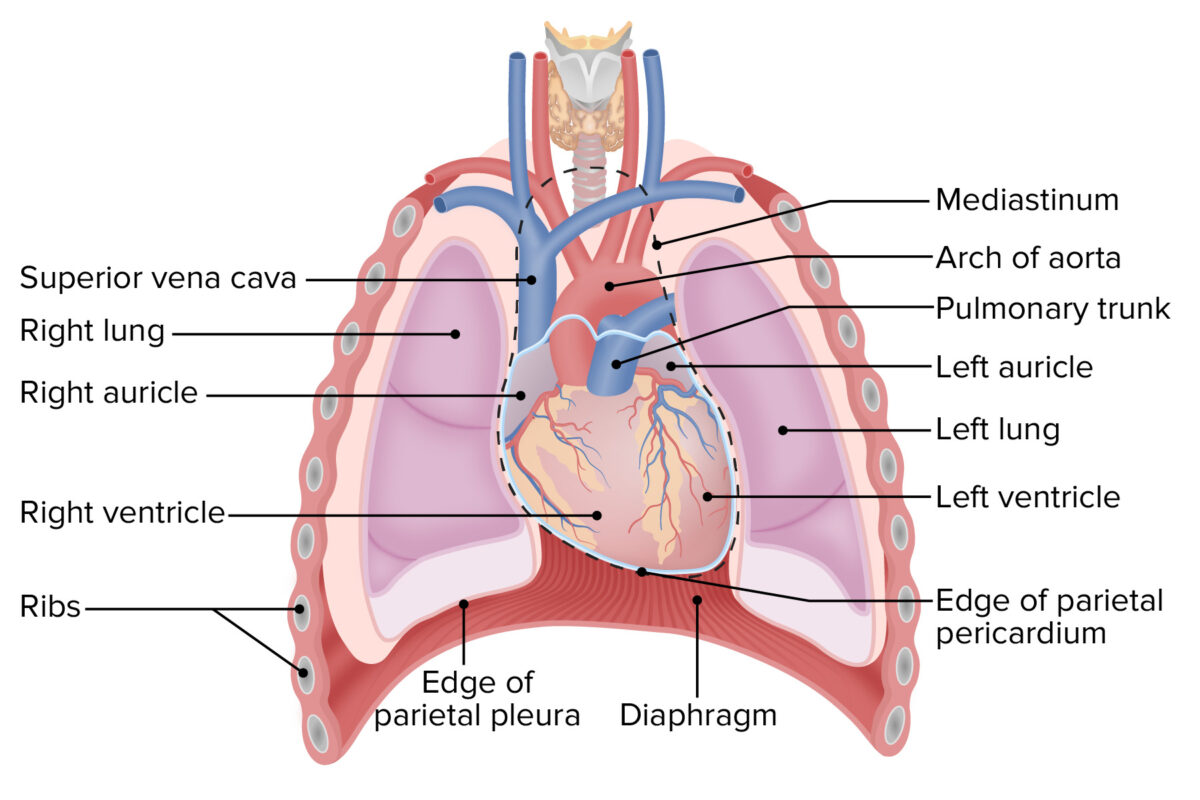
Position of the heart in the thoracic cavity, anterior view
Image by Lecturio.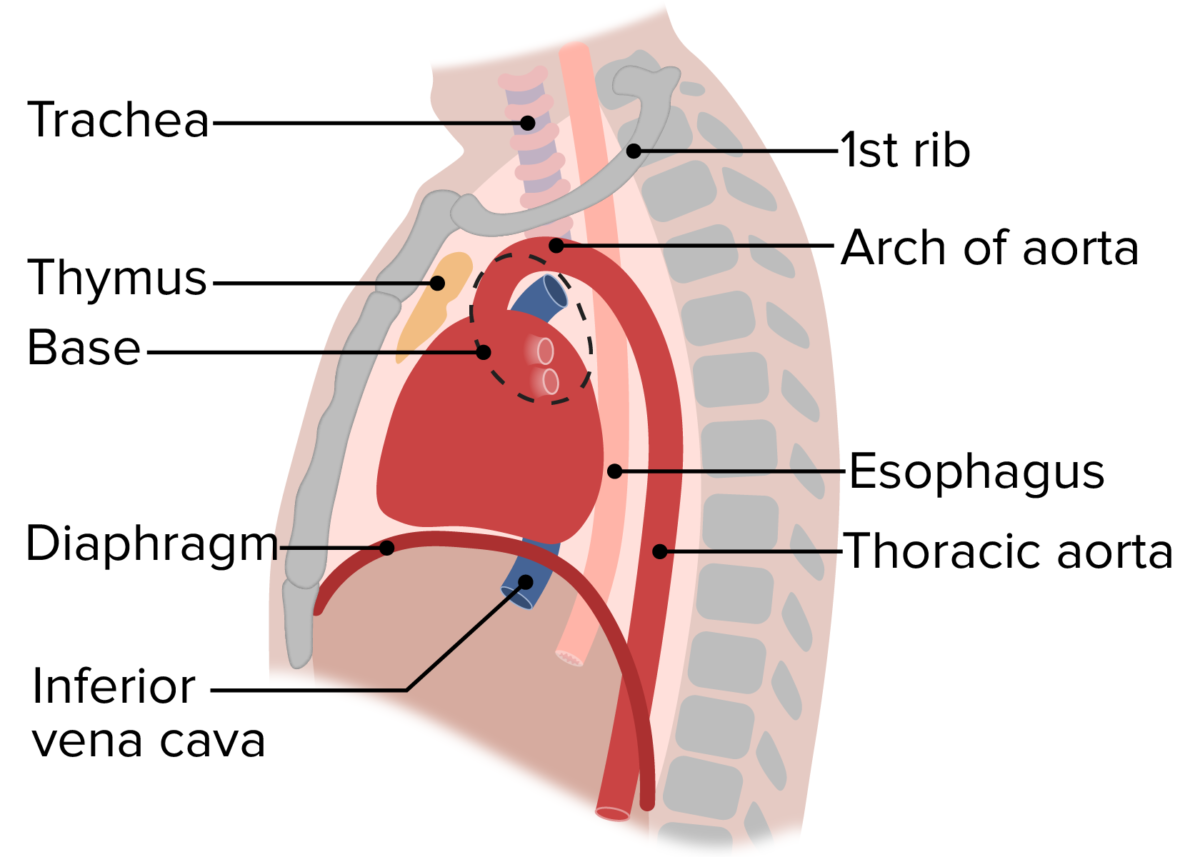
Position of the heart in the thoracic cavity, lateral view
Image by Lecturio.Like the pleural cavity Pleural cavity Paired but separate cavity within the thoracic cavity. It consists of the space between the parietal and visceral pleura and normally contains a capillary layer of serous fluid that lubricates the pleural surfaces. Pleura: Anatomy around the lungs Lungs Lungs are the main organs of the respiratory system. Lungs are paired viscera located in the thoracic cavity and are composed of spongy tissue. The primary function of the lungs is to oxygenate blood and eliminate CO2. Lungs: Anatomy and the peritoneal cavity Peritoneal Cavity The space enclosed by the peritoneum. It is divided into two portions, the greater sac and the lesser sac or omental bursa, which lies behind the stomach. The two sacs are connected by the foramen of winslow, or epiploic foramen. Peritoneum: Anatomy inside the abdomen, the pericardial cavity around the heart is enclosed in a double layer of fibroelastic connective tissue Connective tissue Connective tissues originate from embryonic mesenchyme and are present throughout the body except inside the brain and spinal cord. The main function of connective tissues is to provide structural support to organs. Connective tissues consist of cells and an extracellular matrix. Connective Tissue: Histology known as pericardium.
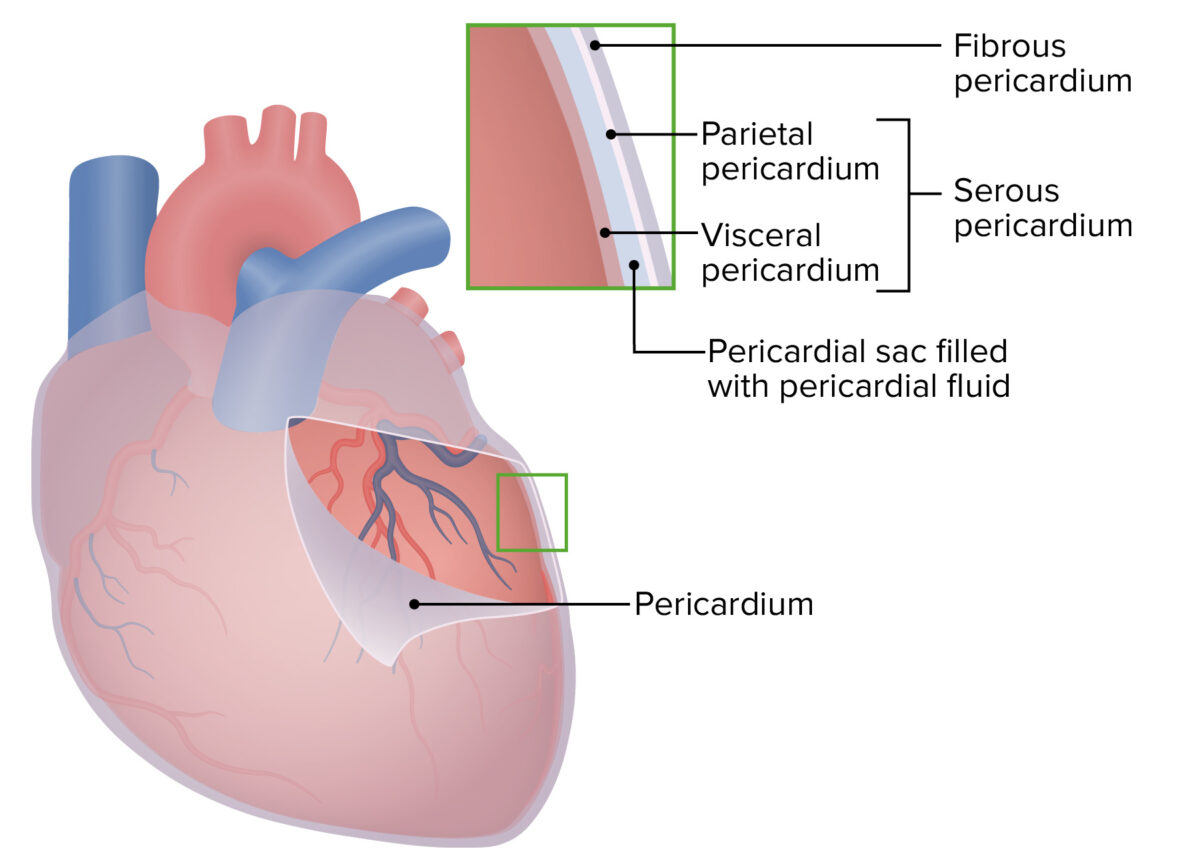
Pericardial cavity of the heart
Image by Lecturio.There are 2 important sinuses, or spaces, within the pericardial cavity:
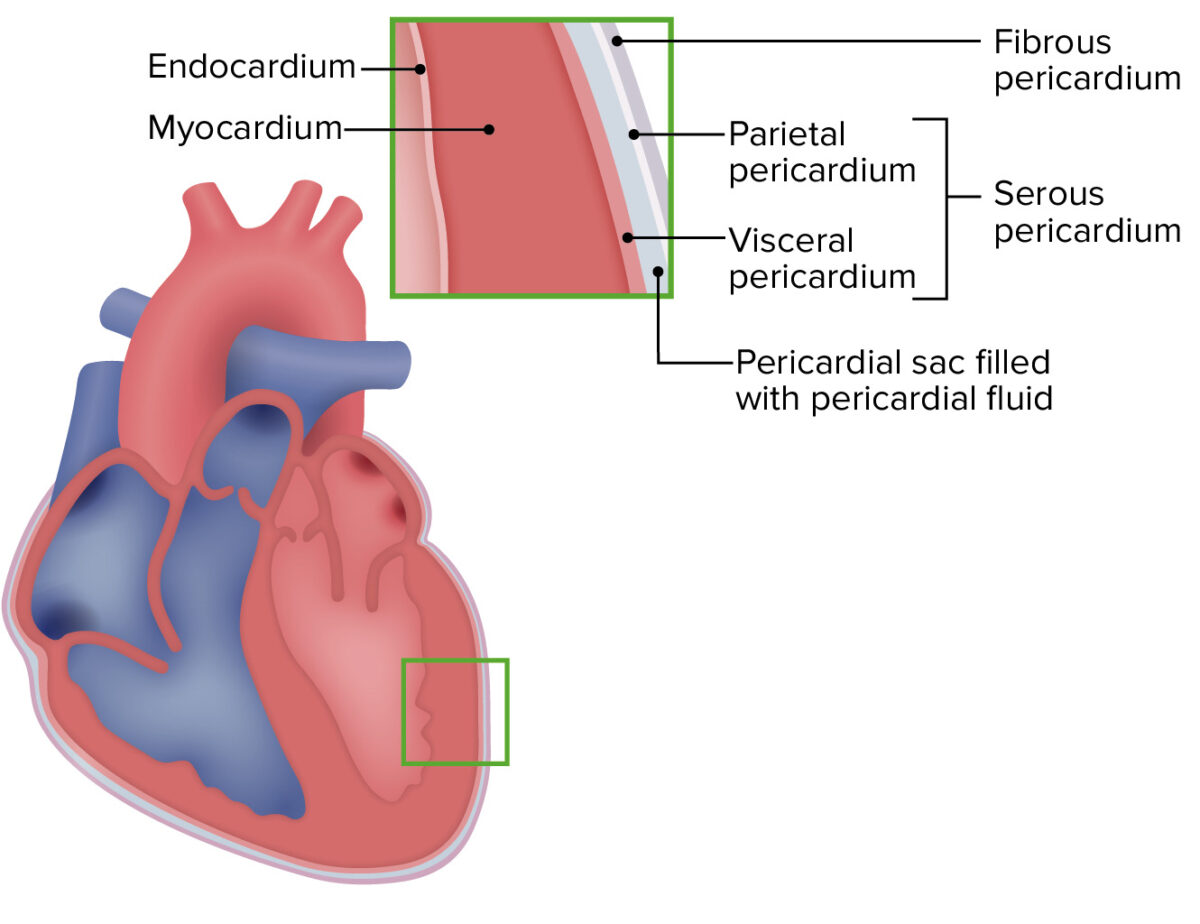
The layers of the heart wall
Image by Lecturio.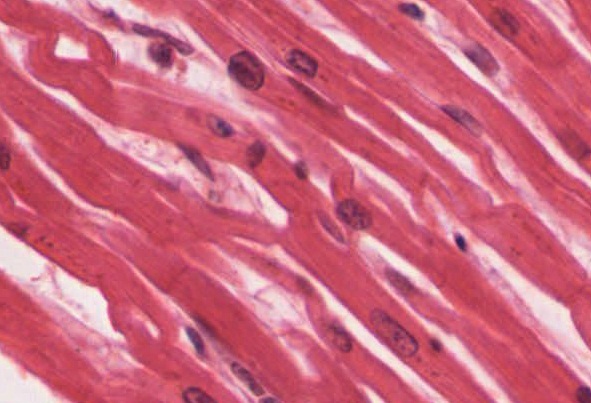
Histologic section of cardiac muscle:
Cardiac muscle tissue is found only in the heart.
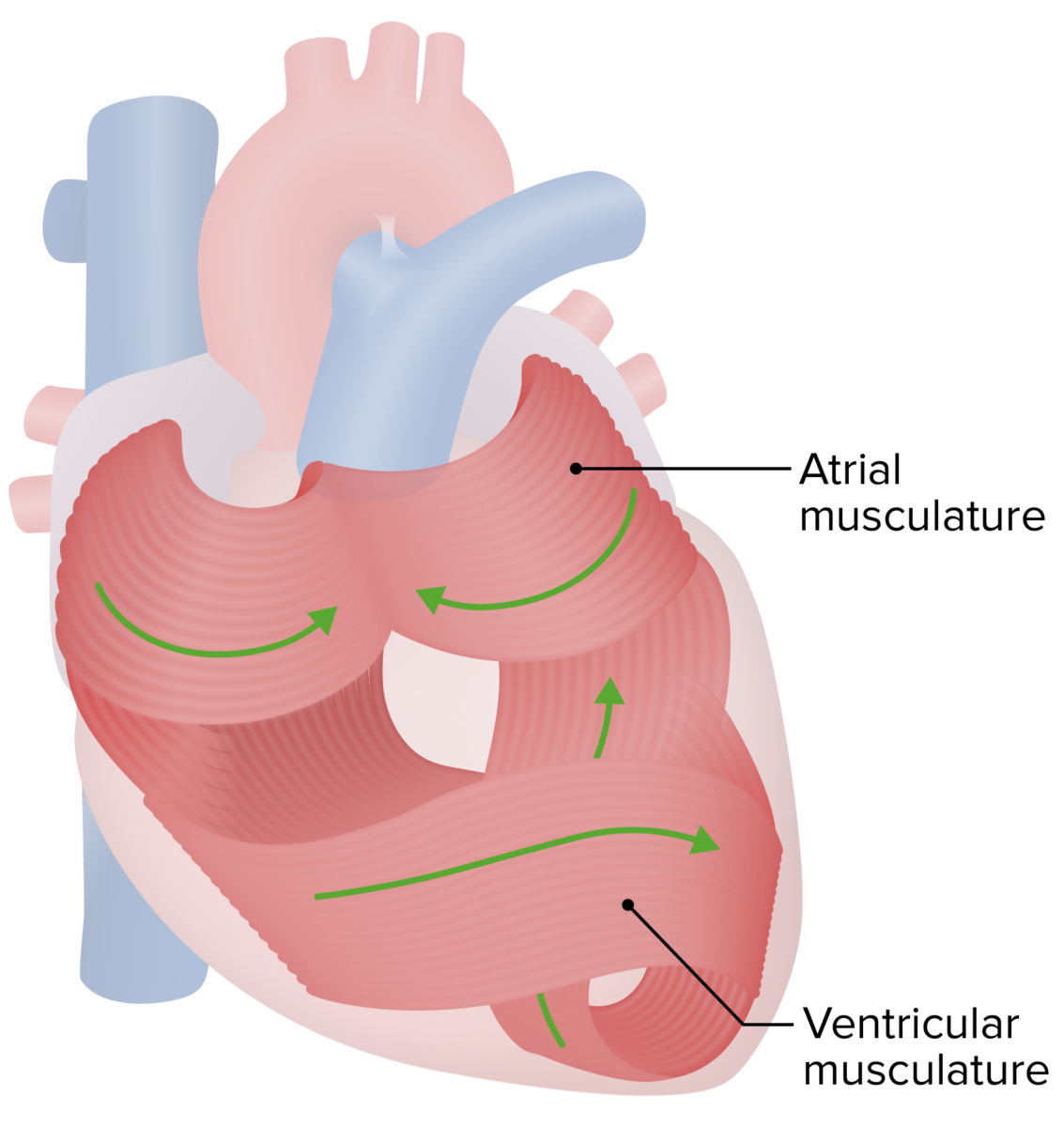
Orientation of the myocardium, allowing the heart to pump blood effectively
Image by Lecturio.The heart has 4 chambers: 2 atria (receiving chambers) and 2 ventricles (pumping chambers).
RA:
LA:
RV:
LV:

Anterior view of the internal cardiac structures
Image by Lecturio.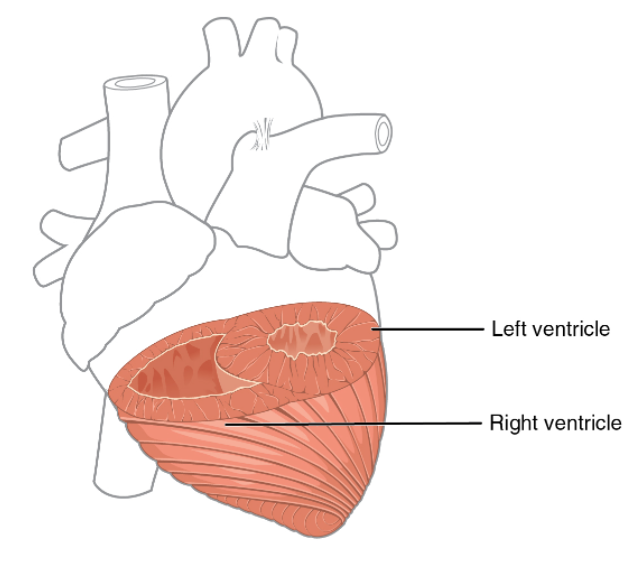
Differences in ventricular thickness
Image: “Heart Musculature” by Philschatz. License: Public Domain, cropped by Lecturio.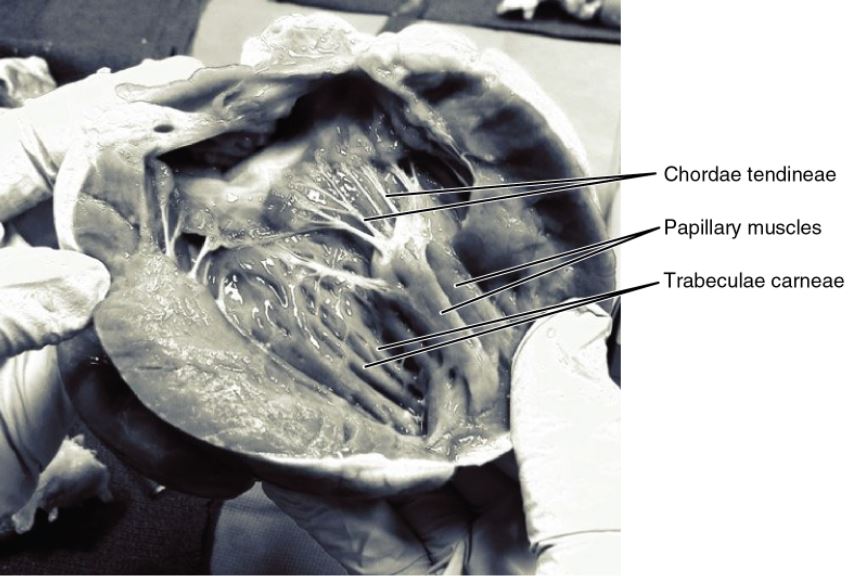
A frontal section of the heart showing part of the mitral valve on the left and the tricuspid valve on the right:
Note how the valves are attached to papillary muscles via the chordae tendineae.
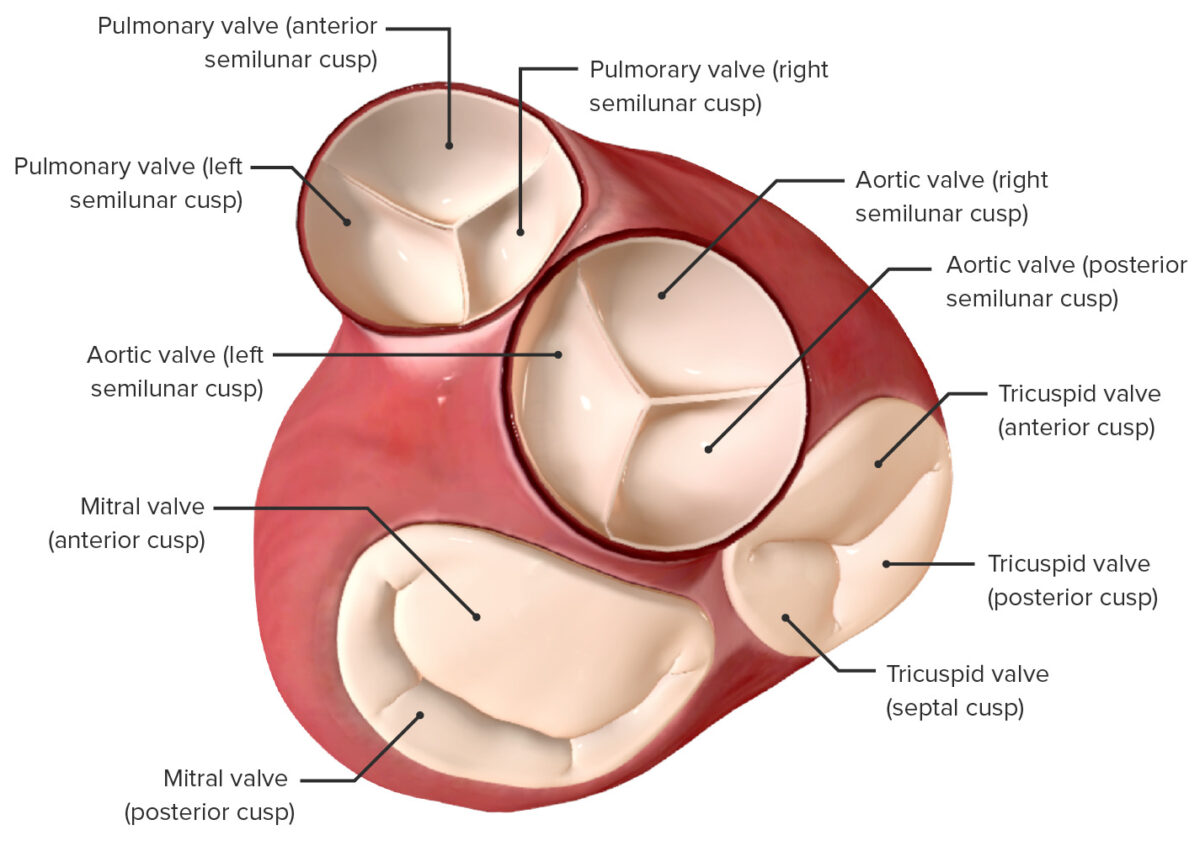
View of the valves of the heart from an atrial perspective:
Atria removed
Blood flows into, through, and out of the heart by sequentially passing through the following structures (in order):
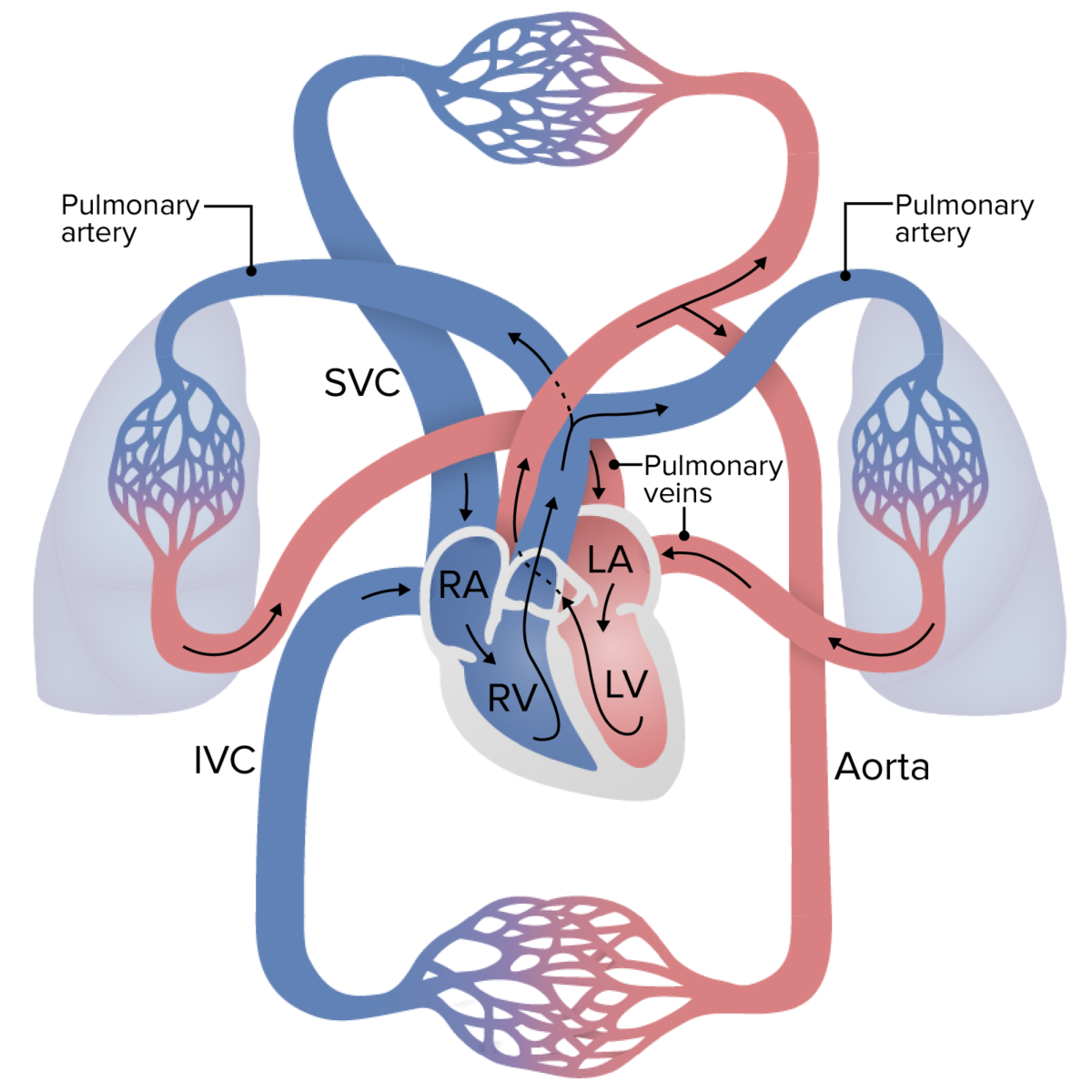
Circulation of blood through the body:
Deoxygenated blood enters the right side of the heart and passes through the pulmonary trunk to the lungs, where it is oxygenated. The blood then returns to the left side of the heart via the pulmonary veins, where it is pumped into the aorta and distributed throughout the body. The blood travels through systemic capillaries, where it is deoxygenated again, and travels back to the heart via the superior and inferior vena cava.
LA: left atrium
LV: left ventricle
RA: right atrium
RV: right ventricle
Coronary circulation Circulation The movement of the blood as it is pumped through the cardiovascular system. ABCDE Assessment describes the flow Flow Blood flows through the heart, arteries, capillaries, and veins in a closed, continuous circuit. Flow is the movement of volume per unit of time. Flow is affected by the pressure gradient and the resistance fluid encounters between 2 points. Vascular resistance is the opposition to flow, which is caused primarily by blood friction against vessel walls. Vascular Resistance, Flow, and Mean Arterial Pressure of blood through the vessels supplying the heart muscle itself. There are 2 primary coronary arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology: the left and the right, and both originate from the aorta Aorta The main trunk of the systemic arteries. Mediastinum and Great Vessels: Anatomy, just above the aortic valve.
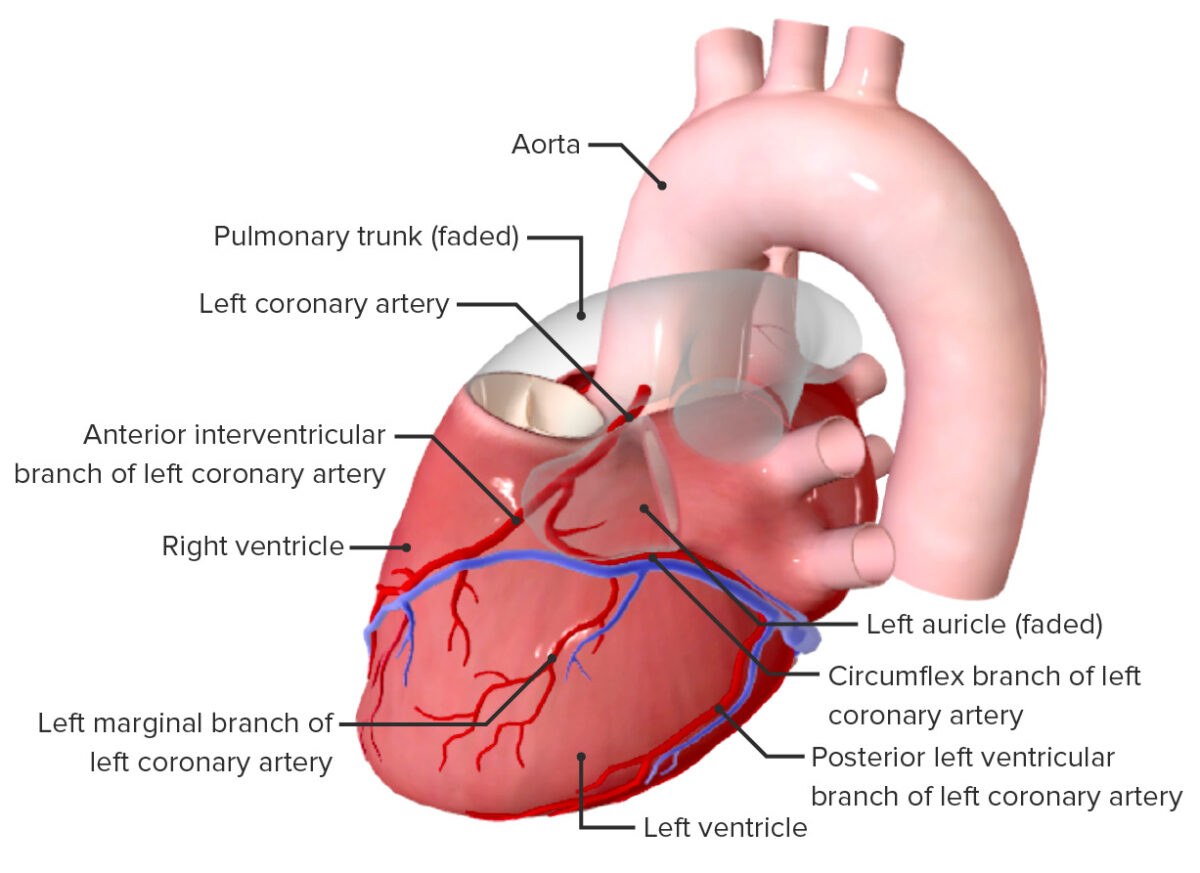
Left coronary artery and its branches
Image by BioDigital, edited by Lecturio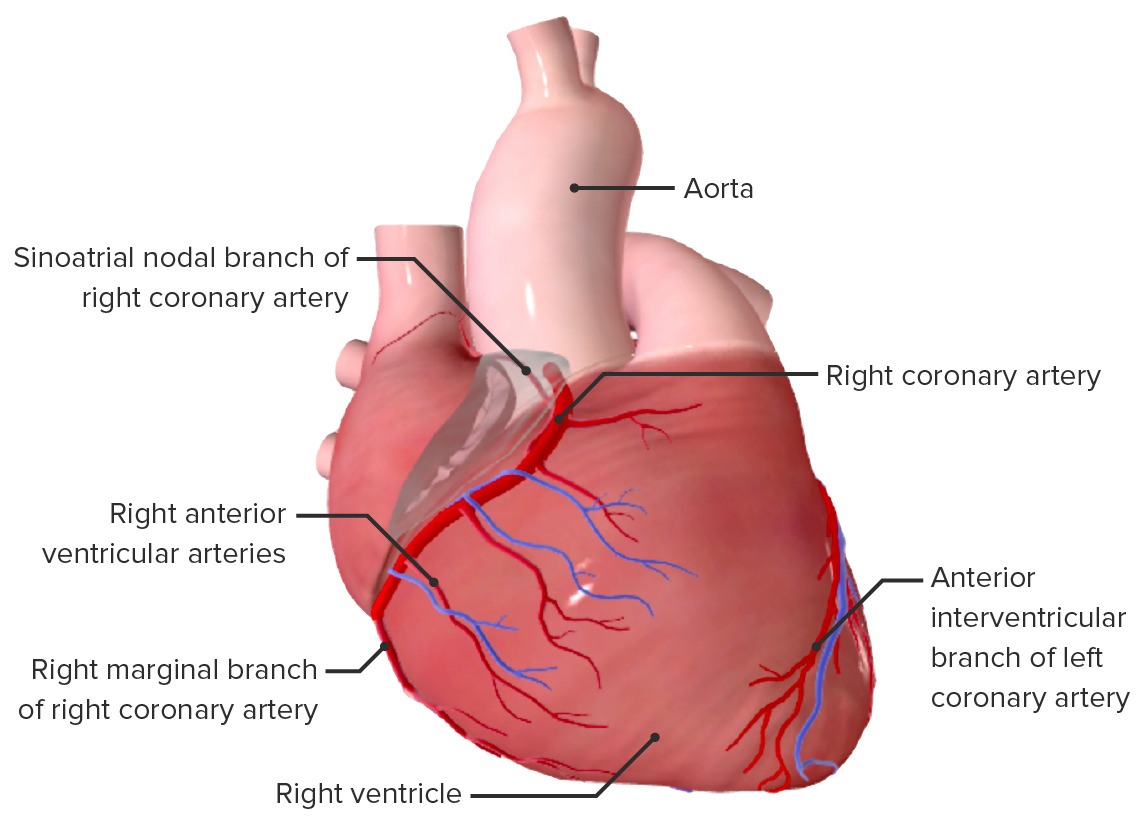
Right coronary artery
Image by BioDigital, edited by Lecturio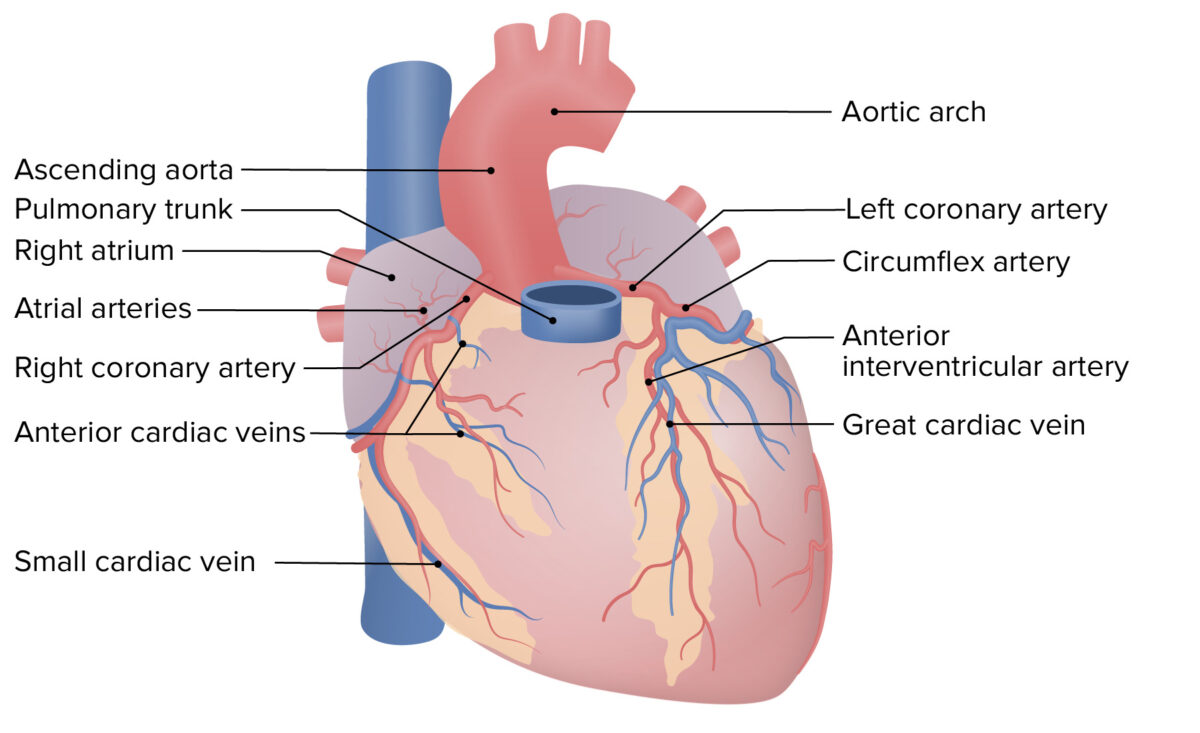
Coronary circulation, anterior view
Image by Lecturio.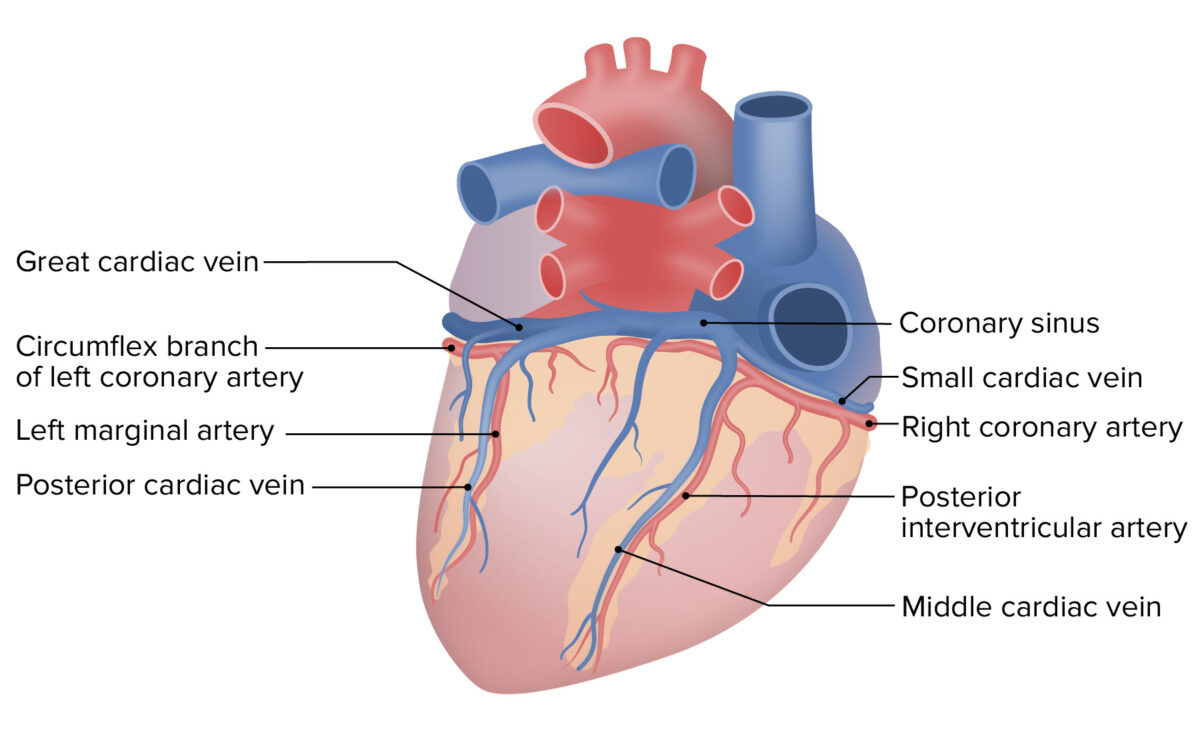
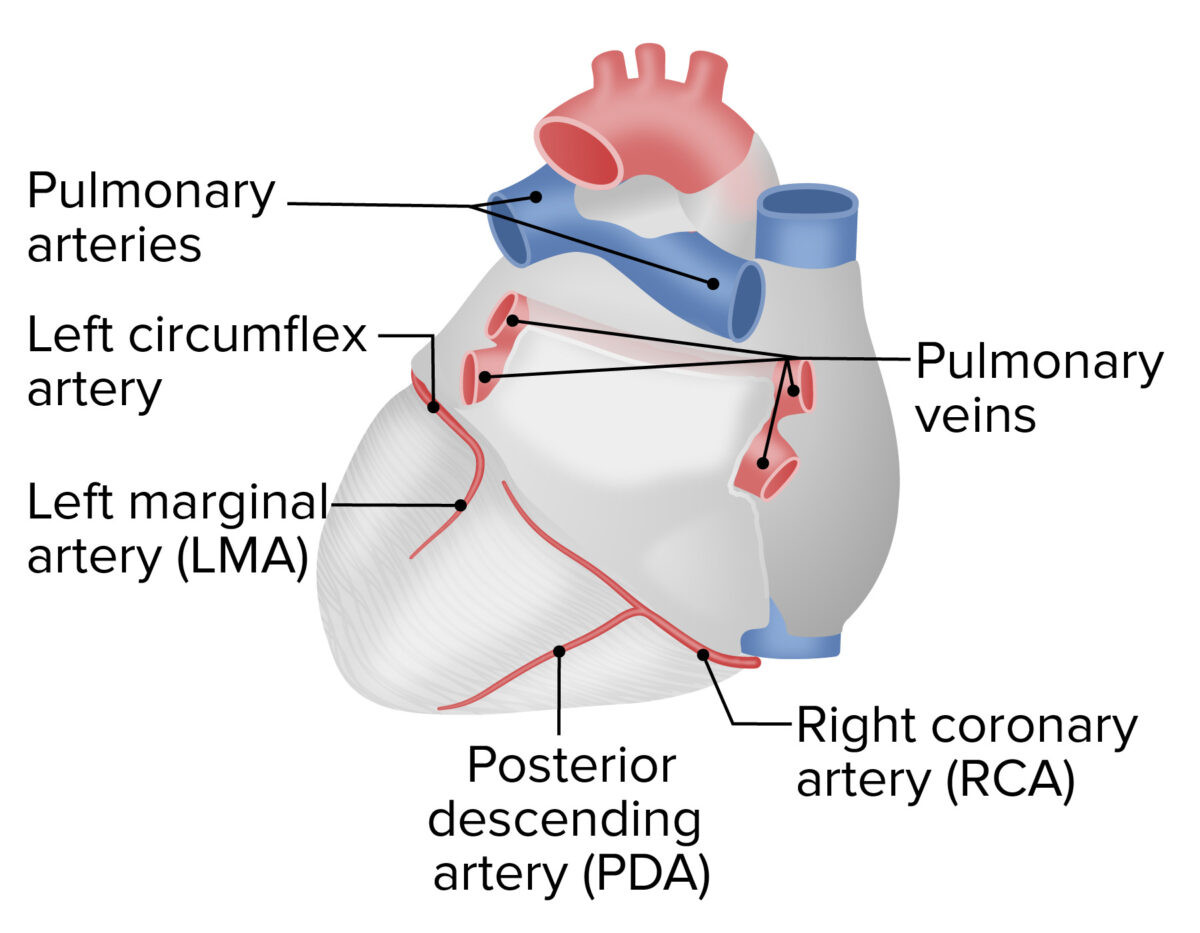
Coronary circulation, posterior view
Image by Lecturio.A person’s coronary dominance pattern is determined by the artery that gives off the PDA PDA The ductus arteriosus (DA) allows blood to bypass pulmonary circulation. After birth, the DA remains open for up to 72 hours and then constricts and involutes, becoming the ligamentum arteriosum. Failure of this process to occur results in patent ductus arteriosus (PDA), a condition that causes up to 10% of congenital heart defects. Patent Ductus Arteriosus (PDA).
Right-dominant pattern of coronary circulation
Image by Lecturio.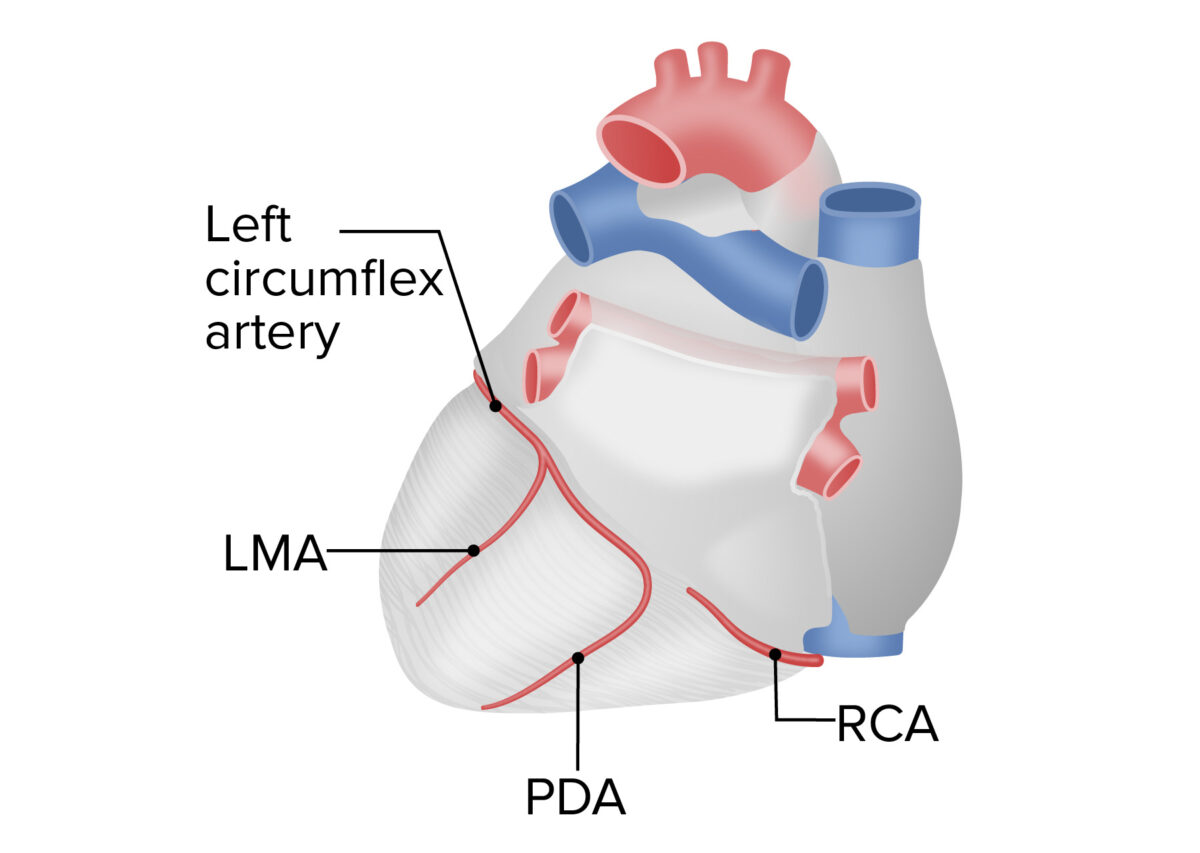
Left-dominant pattern of coronary circulation
Image by Lecturio.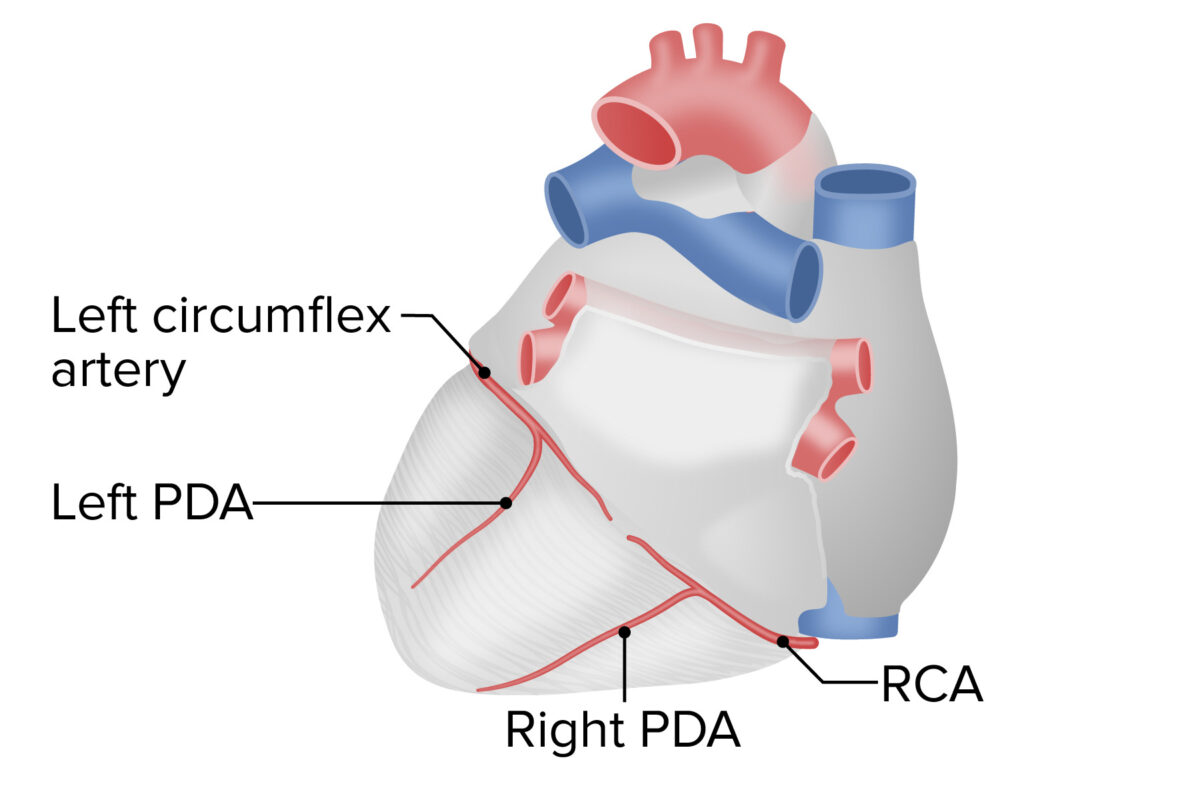
Codominant pattern of coronary circulation
Image by Lecturio.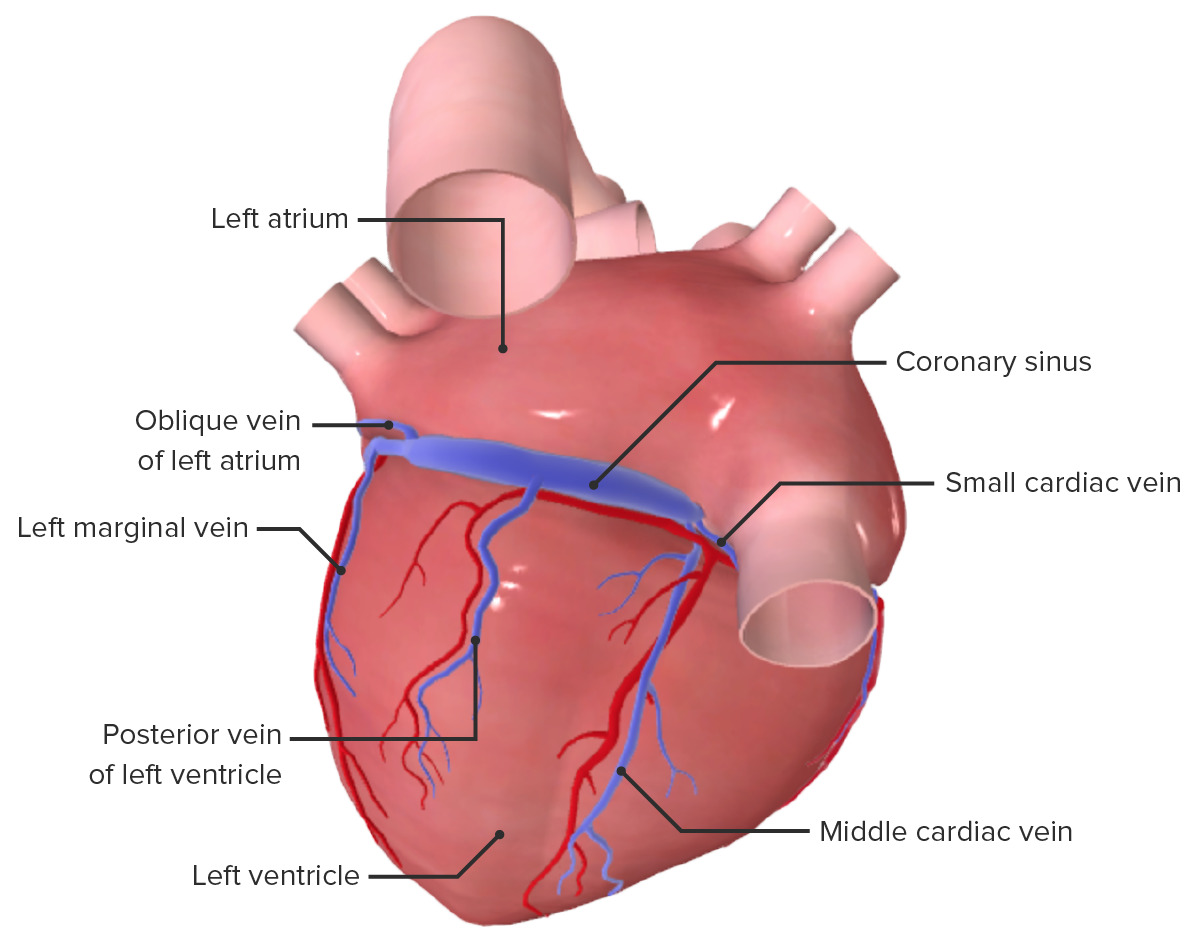
Posterior view of the heart showing the coronary sinus and middle cardiac vein
Image by BioDigital, edited by Lecturio| Vessel | Trajectory | Area of supply/drainage | |
|---|---|---|---|
| Left coronary artery Coronary Artery Truncus Arteriosus | LAD artery | Runs in the anterior IV sulcus toward the apex |
|
| Left circumflex artery | Wraps around toward the posterior aspect of the heart in the coronary (AV) sulcus | Posterior aspect of LA and LV | |
| Right coronary artery Coronary Artery Truncus Arteriosus | PDA PDA The ductus arteriosus (DA) allows blood to bypass pulmonary circulation. After birth, the DA remains open for up to 72 hours and then constricts and involutes, becoming the ligamentum arteriosum. Failure of this process to occur results in patent ductus arteriosus (PDA), a condition that causes up to 10% of congenital heart defects. Patent Ductus Arteriosus (PDA) | Runs in the posterior interventricular sulcus toward the apex | RV and LV and posterior ⅓ of IVS |
| Right marginal artery | Runs over the RV toward the apex | RV and apex of the heart | |
| Great cardiac vein | With the LAD within the anterior IV sulcus | Areas of the heart supplied by the LCA | |
| Middle cardiac vein | With the PDA PDA The ductus arteriosus (DA) allows blood to bypass pulmonary circulation. After birth, the DA remains open for up to 72 hours and then constricts and involutes, becoming the ligamentum arteriosum. Failure of this process to occur results in patent ductus arteriosus (PDA), a condition that causes up to 10% of congenital heart defects. Patent Ductus Arteriosus (PDA) within the posterior IV sulcus | Posterior wall of LV and RV | |
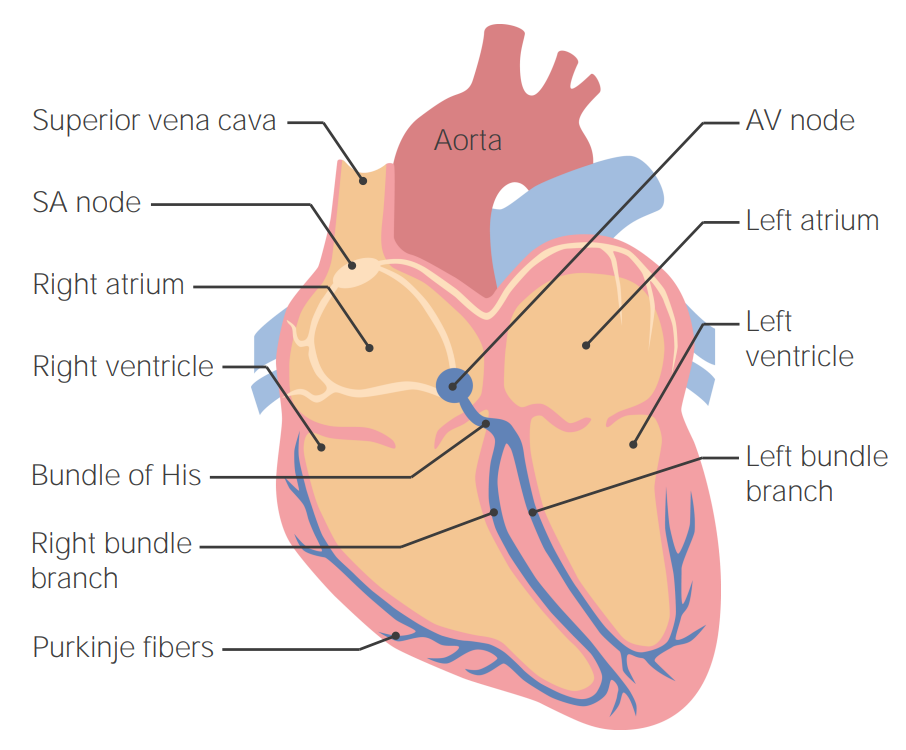
Cardiac conduction system:
Starting with the sinoatrial (SA) node and ending in the Purkinje fibers
AV: atrioventricular