Acute otitis media is an infection in the middle ear characterized by mucosal inflammation and retention of fluid. The most common pathogens are Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. The condition can present with fever, otalgia, and diminished hearing. Diagnosis is made by history, clinical presentation, and otoscopic exam showing a bulging tympanic membrane with reduced mobility. Observation or antibiotics are the usual management approaches, but surgery for tympanostomy tubes may be required if there are recurrent infections. Potential complications include hearing loss, tympanic membrane perforation, and mastoiditis.
Last updated: Sep 12, 2025
Acute otitis media Acute Otitis Media Acute otitis media is an infection in the middle ear characterized by mucosal inflammation and retention of fluid. The most common pathogens are Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. The condition can present with fever, otalgia, and diminished hearing. Acute Otitis Media (AOM) is an infection characterized by the accumulation of fluid and inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation within the middle ear Middle ear The space and structures directly internal to the tympanic membrane and external to the inner ear (labyrinth). Its major components include the auditory ossicles and the eustachian tube that connects the cavity of middle ear (tympanic cavity) to the upper part of the throat. Acute Otitis Media.
Acute otitis media Acute Otitis Media Acute otitis media is an infection in the middle ear characterized by mucosal inflammation and retention of fluid. The most common pathogens are Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. The condition can present with fever, otalgia, and diminished hearing. Acute Otitis Media is an inflammatory condition of the middle ear Middle ear The space and structures directly internal to the tympanic membrane and external to the inner ear (labyrinth). Its major components include the auditory ossicles and the eustachian tube that connects the cavity of middle ear (tympanic cavity) to the upper part of the throat. Acute Otitis Media with an infectious etiology that may be bacterial (most common) or viral.
Bacterial:
Viral:
The middle ear Middle ear The space and structures directly internal to the tympanic membrane and external to the inner ear (labyrinth). Its major components include the auditory ossicles and the eustachian tube that connects the cavity of middle ear (tympanic cavity) to the upper part of the throat. Acute Otitis Media is lined with respiratory mucosa, and the cascade of events affecting adjacent areas is usually reflected in similar changes in the ear.
Endoscopic view of early otitis media of the left middle ear:
The typical aspect of beginning radial vascular drawing, injection of the vessels of the malleus handle, effusion with reddening and beginning protrusion of the tympanic membrane, as well as cloudiness of the surface of the eardrum are found.

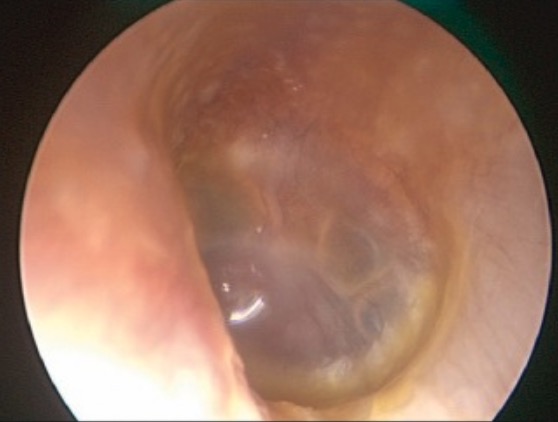
Endoscopic view of acute otitis media:
The middle ear is filled with a creamy-white mucopurulent exudate, which is causing the tympanic membrane to bulge laterally. Note the dilatation of the radial blood vessels of the tympanic membrane, which appear like the “spokes of a wheel.”

Endoscopic view of an advanced acute otitis media of the right middle ear:
Severe inflammatory reaction and protrusion of the eardrum are found.
The diagnosis of acute otitis media Acute Otitis Media Acute otitis media is an infection in the middle ear characterized by mucosal inflammation and retention of fluid. The most common pathogens are Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. The condition can present with fever, otalgia, and diminished hearing. Acute Otitis Media is primarily based on clinical presentation and otoscopic exam. No lab tests or imaging are needed unless there are special circumstances.
Management may vary based on practice location. The following information is based on U.S. recommendations from the American Academy of Pediatrics (AAP) and the American Academy of Family Physicians Physicians Individuals licensed to practice medicine. Clinician–Patient Relationship (AAFP) and from the UK’s National Institute for Health and Care Excellence (NICE) guidelines.
General approach:[8–11]
Observation:
| Pediatric age | Unilateral or bilateral AOM with severe symptoms or otorrhea Otorrhea Otitis Externa | Bilateral AOM without otorrhea Otorrhea Otitis Externa | Unilateral AOM without otorrhea Otorrhea Otitis Externa |
|---|---|---|---|
| < 6 months | Antibiotic therapy | Antibiotic therapy | Antibiotic therapy |
| 6–23 months | Antibiotic therapy | Antibiotic therapy | Antibiotic therapy or observation |
| ≥ 2 years (24 months) | Antibiotic therapy | Antibiotic therapy or observation | Antibiotic therapy or observation |
Pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways control:[7,9,10]
Antibiotics:
| Medication | Pediatric dosing | Adult dosing | Notes |
|---|---|---|---|
| Amoxicillin Amoxicillin A broad-spectrum semisynthetic antibiotic similar to ampicillin except that its resistance to gastric acid permits higher serum levels with oral administration. Penicillins | 80‒90 mg/kg/day by mouth in 2 divided doses | 500 mg by mouth every 8 hours OR 875 mg by mouth every 12 hours | 1st-line therapy for children who:
|
| Amoxicillin Amoxicillin A broad-spectrum semisynthetic antibiotic similar to ampicillin except that its resistance to gastric acid permits higher serum levels with oral administration. Penicillins/ clavulanate | 90 mg amoxicillin Amoxicillin A broad-spectrum semisynthetic antibiotic similar to ampicillin except that its resistance to gastric acid permits higher serum levels with oral administration. Penicillins per kg/day, 6.4 mg clavulanate per kg/day (14:1 ratio) by mouth in 2 divided doses | 875 mg/125 mg by mouth every 12 hours |
|
| Cefdinir | 14 mg/kg/day by mouth in 1 or 2 daily doses | 600 mg by mouth once daily OR 300 mg by mouth twice daily | |
| Cefuroxime | 30 mg/kg/day by mouth in 2 divided doses | 500 mg by mouth twice daily | |
| Cefpodoxime | 10 mg/kg/day by mouth in 2 divided doses | 200 mg by mouth twice daily | |
| Ceftriaxone Ceftriaxone A broad-spectrum cephalosporin antibiotic and cefotaxime derivative with a very long half-life and high penetrability to meninges, eyes and inner ears. Cephalosporins | 50 mg IM or IV per day | 1 g IM or 1‒2 g IV once daily for 3 days | |
| Azithromycin Azithromycin A semi-synthetic macrolide antibiotic structurally related to erythromycin. It has been used in the treatment of Mycobacterium avium intracellulare infections, toxoplasmosis, and cryptosporidiosis. Macrolides and Ketolides | 10 mg/kg by mouth once on day 1, then 5 mg/kg by mouth once daily on days 2‒5 | 500 mg by mouth once on day 1, then 250 mg once daily on days 2‒5 | 1st-line therapy for patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with penicillin Penicillin Rheumatic Fever and cephalosporin Cephalosporin Multidrug-resistant Organisms and Nosocomial Infections allergies Allergies A medical specialty concerned with the hypersensitivity of the individual to foreign substances and protection from the resultant infection or disorder. Selective IgA Deficiency |
| Clarithromycin Clarithromycin A semisynthetic macrolide antibiotic derived from erythromycin that is active against a variety of microorganisms. It can inhibit protein synthesis in bacteria by reversibly binding to the 50s ribosomal subunits. This inhibits the translocation of aminoacyl transfer-RNA and prevents peptide chain elongation. Macrolides and Ketolides | 15 mg/kg/day in 2 divided doses | 500 mg by mouth twice daily | Alternative agent for patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with penicillin Penicillin Rheumatic Fever and cephalosporin Cephalosporin Multidrug-resistant Organisms and Nosocomial Infections allergies Allergies A medical specialty concerned with the hypersensitivity of the individual to foreign substances and protection from the resultant infection or disorder. Selective IgA Deficiency |
| Clindamycin Clindamycin An antibacterial agent that is a semisynthetic analog of lincomycin. Lincosamides | 30‒40 mg/kg/day in 3 divided doses for 3 days | 300 mg every 6‒8 hours |
Other instructions:
Indications for referral to otorhinolaryngology:
Two types of complications can occur.
Intratemporal complications:
Intracranial complications:
Diagnosis Codes:
These codes are used to diagnose
Acute Otitis Media
Acute Otitis Media
Acute otitis media is an infection in the middle ear characterized by mucosal inflammation and retention of fluid. The most common pathogens are Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. The condition can present with fever, otalgia, and diminished hearing.
Acute Otitis Media (AOM), an infection of the
middle ear
Middle ear
The space and structures directly internal to the tympanic membrane and external to the inner ear (labyrinth). Its major components include the auditory ossicles and the eustachian tube that connects the cavity of middle ear (tympanic cavity) to the upper part of the throat.
Acute Otitis Media. The codes are specific to the ear (left, right, bilateral) and can specify the type of infection.
| Coding System | Code | Description |
|---|---|---|
| ICD-10-CM | H66.90 | Otitis media, unspecified, unspecified ear |
| ICD-10-CM | H66.001 | Acute suppurative otitis media without spontaneous rupture of eardrum, right ear |
Procedures/Interventions:
This code is for a tympanostomy, a procedure to insert ear tubes (pressure equalization tubes), which is performed for recurrent
acute otitis media
Acute Otitis Media
Acute otitis media is an infection in the middle ear characterized by mucosal inflammation and retention of fluid. The most common pathogens are Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. The condition can present with fever, otalgia, and diminished hearing.
Acute Otitis Media or chronic otitis media with effusion.
| Coding System | Code | Description |
|---|---|---|
| CPT | 69436 | Tympanostomy (requiring insertion of ventilating tube), general anesthesia General anesthesia Procedure in which patients are induced into an unconscious state through use of various medications so that they do not feel pain during surgery. Anesthesiology: History and Basic Concepts |
Medications:
This code is for
amoxicillin
Amoxicillin
A broad-spectrum semisynthetic antibiotic similar to ampicillin except that its resistance to gastric acid permits higher serum levels with oral administration.
Penicillins, the first-line oral antibiotic recommended for the treatment of uncomplicated
acute otitis media
Acute Otitis Media
Acute otitis media is an infection in the middle ear characterized by mucosal inflammation and retention of fluid. The most common pathogens are Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. The condition can present with fever, otalgia, and diminished hearing.
Acute Otitis Media in children.
| Coding System | Code | Description |
|---|---|---|
| RxNorm | 834 | Amoxicillin Amoxicillin A broad-spectrum semisynthetic antibiotic similar to ampicillin except that its resistance to gastric acid permits higher serum levels with oral administration. Penicillins (ingredient) |