Acute cholangitis refers to acute inflammation in the bile duct system; it is a life-threatening condition characterized by fever, jaundice, and abdominal pain. This condition develops as a result of stasis and infection of the biliary tract. Septic shock, liver abscess, and multi-organ dysfunction are potential serious complications. The diagnosis is confirmed with ultrasound (or other hepatobiliary imaging studies) showing dilation of the common bile duct (CBD) or gallstones, elevated liver function tests, and leukocytosis. Treatment includes hemodynamic stabilization, broad-spectrum antibiotics, urgent biliary drainage, and addressing the underlying etiology (e.g., cholecystectomy for gallstones).
Last updated: Dec 15, 2025
Mnemonic: Bacteria Bacteria Bacteria are prokaryotic single-celled microorganisms that are metabolically active and divide by binary fission. Some of these organisms play a significant role in the pathogenesis of diseases. Bacteriology responsible for cholangitis—KEEPS:
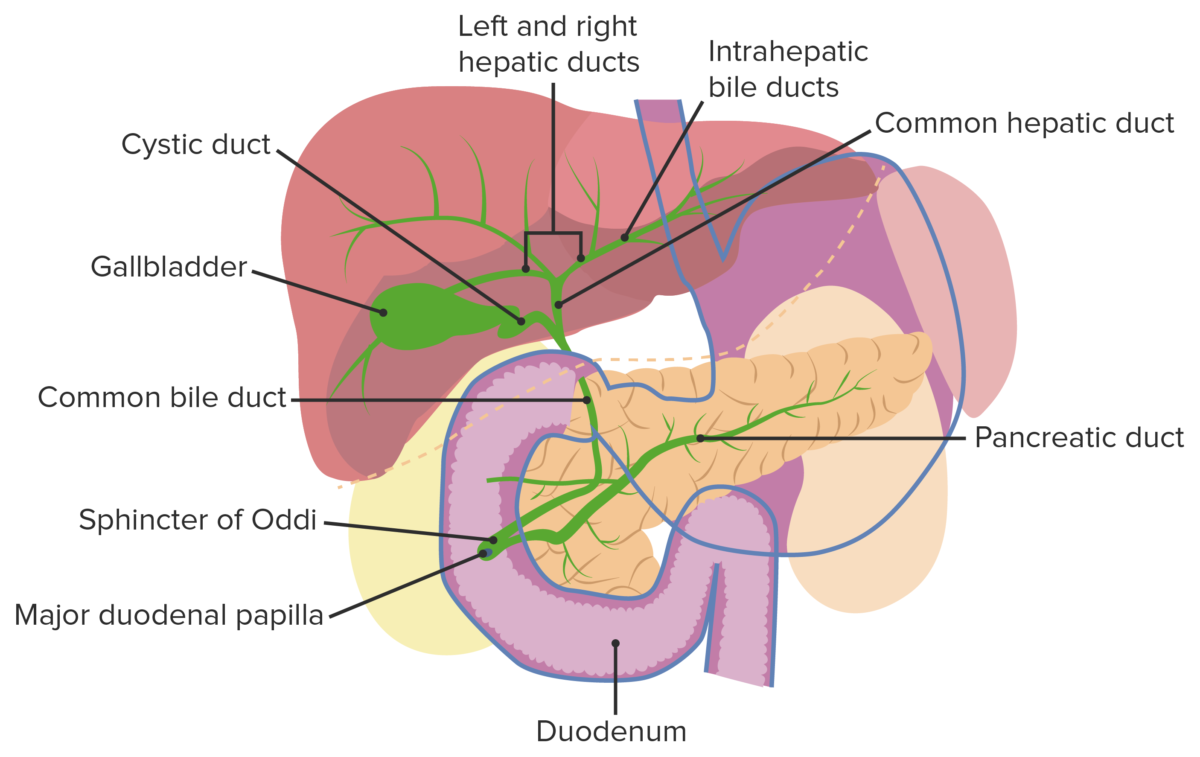
Gallbladder and biliary tract: Bacteria from the duodenum can ascend into the bile duct due to an obstruction or a disruption in the sphincter of Oddi.
Image by Lecturio.
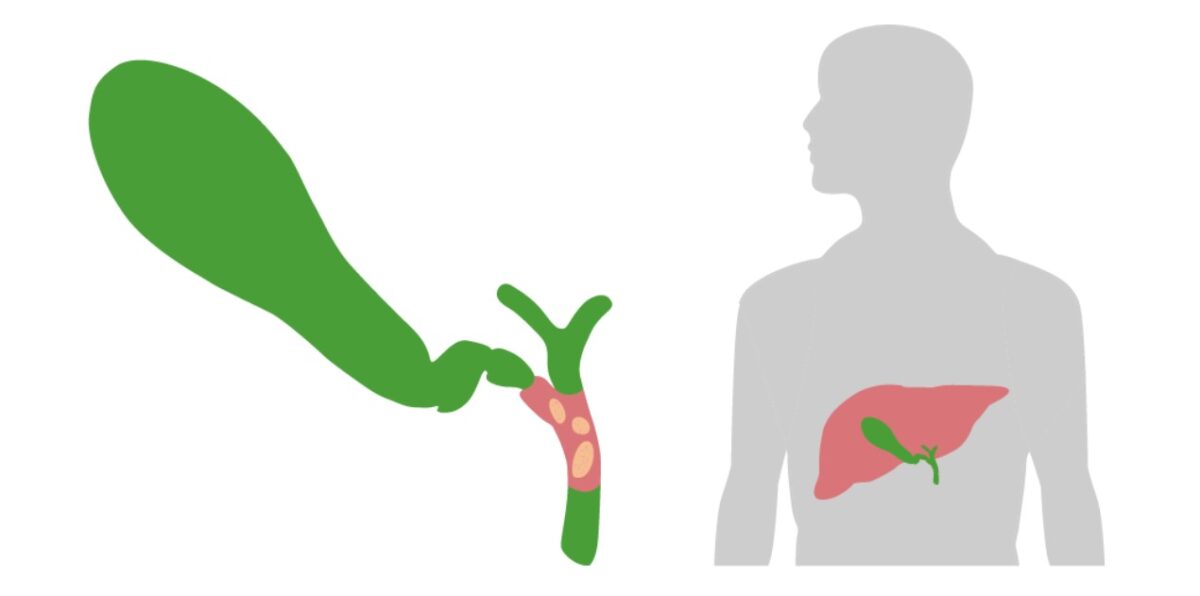
Obstruction (usually due to a stone) of the CBD is a crucial step in the development of acute cholangitis.
Image by Lecturio.The next step in evaluation is determining presence of inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation and biliary obstruction/stasis.[5,6,13]
Imaging is necessary to confirm the diagnosis and to exclude other conditions. Generally, on initial presentation, ultrasonography and CT are performed 1st in evaluating cholestasis.
Diagnostic criteria (Tokyo guidelines 2018)
| Suspected diagnosis:1 item from A + 1 item from either B or C Definite diagnosis:1 item from A + 1 item from B + 1 item from C |
|
| A. Systemic inflammation Systemic Inflammation Surgical Site Infections | Fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever (temperature > 38 °C) and/or shaking chills Chills The sudden sensation of being cold. It may be accompanied by shivering. Fever |
|---|---|
| Laboratory evidence of inflammatory response:
|
|
| B. Cholestasis | Jaundice Jaundice Jaundice is the abnormal yellowing of the skin and/or sclera caused by the accumulation of bilirubin. Hyperbilirubinemia is caused by either an increase in bilirubin production or a decrease in the hepatic uptake, conjugation, or excretion of bilirubin. Jaundice (total bilirubin Bilirubin A bile pigment that is a degradation product of heme. Heme Metabolism ≥ 2 mg/dL) |
| Abnormal
liver
Liver
The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood.
Liver: Anatomy tests > 1.5 the standard upper
limit
Limit
A value (e.g., pressure or time) that should not be exceeded and which is specified by the operator to protect the lung
Invasive Mechanical Ventilation of normal:
|
C.Imaging findings | Biliary dilatation |
| Evidence of the etiology (e.g., common bile Bile An emulsifying agent produced in the liver and secreted into the duodenum. Its composition includes bile acids and salts; cholesterol; and electrolytes. It aids digestion of fats in the duodenum. Gallbladder and Biliary Tract: Anatomy duct stone(s), stricture Stricture Primary Sclerosing Cholangitis) | |
Assessing severity of illness
| Category | Description | Findings |
|---|---|---|
| Grade I | Mild |
|
| Grade II | Moderate | Any 2 of the following:
|
| Grade III | Severe | Associated with organ dysfunction (any 1 of the following):
|
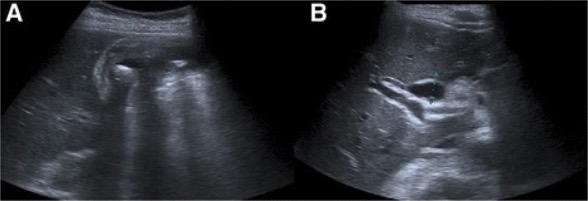
Acute cholangitis: Abdominal ultrasound showing gallbladder wall thickening, pericholecystic fluid and cholelithiasis (a). The common bile duct is dilated (b).
Image: “Abdominal ultrasound” by Serviço de Gastrenterologia e Hepatologia, Hospital de Santa Maria, Centro Hospitalar Lisboa Norte, Avenida Professor Egas Moniz, Lisboa, 1649-035, Portugal. License: CC BY 4.0Management guidelines may vary depending on practice location, and should be guided by specialist consultation (e.g., gastroenterology). The following information is based on the current literature and guidelines.
Overview of the management approach[9,11,13]
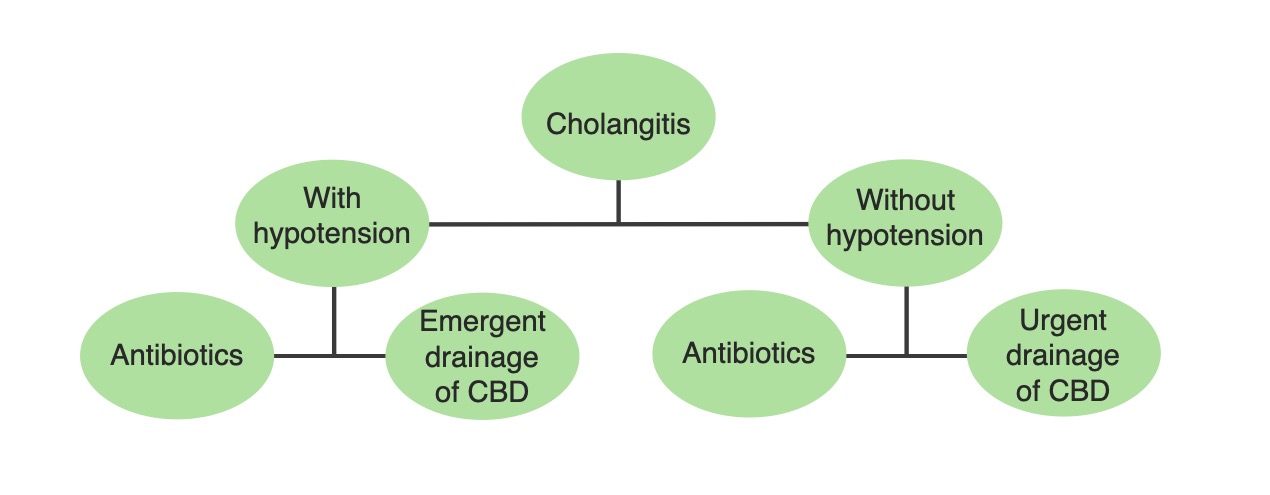
A simplified management algorithm for acute cholangitis based on the hemodynamic stability of the patient: Definitive treatment requires source control with biliary drainage. Therefore, this treatment is performed emergently in patients who are hemodynamically unstable.
Image by Lecturio.Supportive therapy[9–11]
Antibiotic coverage for gram negatives and anaerobes Anaerobes Lincosamides:[10–12]
| Medication | Typical dosing (adult; IV) | |
|---|---|---|
| Fluoroquinolones Fluoroquinolones Fluoroquinolones are a group of broad-spectrum, bactericidal antibiotics inhibiting bacterial DNA replication. Fluoroquinolones cover gram-negative, anaerobic, and atypical organisms, as well as some gram-positive and multidrug-resistant (MDR) organisms. Fluoroquinolones | Ciprofloxacin Ciprofloxacin A broad-spectrum antimicrobial carboxyfluoroquinoline. Fluoroquinolones | 400 mg every 12 hours |
| Levofloxacin Levofloxacin The l-isomer of ofloxacin. Fluoroquinolones | 750 mg daily | |
| Moxifloxacin Moxifloxacin A fluoroquinolone that acts as an inhibitor of DNA topoisomerase II and is used as a broad-spectrum antibacterial agent. Fluoroquinolones | 400 mg daily | |
| Metronidazole Metronidazole A nitroimidazole used to treat amebiasis; vaginitis; trichomonas infections; giardiasis; anaerobic bacteria; and treponemal infections. Pyogenic Liver Abscess | 500 mg every 8 hours | |
| Cephalosporins Cephalosporins Cephalosporins are a group of bactericidal beta-lactam antibiotics (similar to penicillins) that exert their effects by preventing bacteria from producing their cell walls, ultimately leading to cell death. Cephalosporins are categorized by generation and all drug names begin with “cef-” or “ceph-.” Cephalosporins | Cefazolin Cefazolin A semisynthetic cephalosporin analog with broad-spectrum antibiotic action due to inhibition of bacterial cell wall synthesis. It attains high serum levels and is excreted quickly via the urine. Cephalosporins | 1–2 g every 8 hours |
| Cefuroxime | 1.5 g every 8 hours | |
| Ceftriaxone Ceftriaxone A broad-spectrum cephalosporin antibiotic and cefotaxime derivative with a very long half-life and high penetrability to meninges, eyes and inner ears. Cephalosporins | 1–2 g daily | |
| Cefotaxime Cefotaxime Semisynthetic broad-spectrum cephalosporin. Cephalosporins | 2 g every 8 hours | |
| Piperacillin Piperacillin Semisynthetic, broad-spectrum, ampicillin derived ureidopenicillin antibiotic proposed for pseudomonas infections. It is also used in combination with other antibiotics. Penicillins– tazobactam Tazobactam A penicillanic acid and sulfone derivative and potent beta-lactamase inhibitor that enhances the activity of other anti-bacterial agents against beta-lactamase producing bacteria. Cephalosporins | ||
| Carbapenems Carbapenems A group of beta-lactam antibiotics in which the sulfur atom in the thiazolidine ring of the penicillin molecule is replaced by a carbon atom. Thienamycins are a subgroup of carbapenems which have a sulfur atom as the first constituent of the side chain. Carbapenems and Aztreonam | Ertapenem Ertapenem A carbapenem derivative antibacterial agent that is more stable to renal dehydropeptidase I than imipenem, but does not need to be given with an enzyme inhibitor such as cilastatin. It is used in the treatment of gram-positive and gram-negative bacterial infections including intra-abdominal infections, acute gynecological infections, complicated urinary tract infections, skin infections, and respiratory tract infections. It is also used to prevent infection in colorectal surgery. Carbapenems and Aztreonam | 1 g daily |
| Imipenem Imipenem Semisynthetic thienamycin that has a wide spectrum of antibacterial activity against gram-negative and gram-positive aerobic and anaerobic bacteria, including many multiresistant strains. It is stable to beta-lactamases. Clinical studies have demonstrated high efficacy in the treatment of infections of various body systems. Its effectiveness is enhanced when it is administered in combination with cilastatin, a renal dipeptidase inhibitor. Carbapenems and Aztreonam–cilastin | 500 mg every 6 hours OR 1 g every 8 hours | |
| Meropenem Meropenem A thienamycin derivative antibacterial agent that is more stable to renal dehydropeptidase I than imipenem, but does not need to be given with an enzyme inhibitor such as cilastatin. It is used in the treatment of bacterial infections, including infections in immunocompromised patients. Carbapenems and Aztreonam | 1 g every 8 hours | |
| Doripenem Doripenem A carbapenem derivative antibacterial agent that is more stable to renal dehydropeptidase I than imipenem, but does not need to be given with an enzyme inhibitor such as cilastatin. It is used in the treatment of infections such as hospital-acquired pneumonia, and complicated intra-abdominal or urinary-tract infections, including pyelonephritis. Carbapenems and Aztreonam | 500 mg every 8 hours | |
Duration of antibiotics:[10]
Factors considered in choosing antibiotic regimens (see table):[10–12]
| Grade | Grade I | Grade II | Grade III or health care–associated infection |
|---|---|---|---|
| Single agents |
|
||
| Agents that may be used alone OR in combination with metronidazole Metronidazole A nitroimidazole used to treat amebiasis; vaginitis; trichomonas infections; giardiasis; anaerobic bacteria; and treponemal infections. Pyogenic Liver Abscess** |
Biliary decompression procedures[9,15]

A patient presented to the emergency department with Charcot triad and was diagnosed with acute cholangitis. Percutaneous transhepatic cholangiography shows a dilated common bile duct containing multiple calcified stones affected above the papilla of Vater. Stone extraction and biliary drainage would be performed during this procedure.
Image: “Percutaneous cholangiography” by Service of Gastroenterology and Hepatology, Geneva University Hospitals, Rue Gabrielle Perret Gentil 24, 1211 Geneva, Switzerland. License: CC BY 2.0The following table outlines common biliary diagnoses and how they may be differentiated from acute cholangitis Acute Cholangitis Acute cholangitis is a life-threatening condition characterized by fever, jaundice, and abdominal pain which develops as a result of stasis and infection of the biliary tract. Septic shock, liver abscess, and multi-organ dysfunction are potential serious complications. Acute Cholangitis:
| Condition | Pathology | Clinical presentation | Diagnosis | Management |
|---|---|---|---|---|
| Cholelithiasis Cholelithiasis Cholelithiasis (gallstones) is the presence of stones in the gallbladder. Most gallstones are cholesterol stones, while the rest are composed of bilirubin (pigment stones) and other mixed components. Patients are commonly asymptomatic but may present with biliary colic (intermittent pain in the right upper quadrant). Cholelithiasis | Presence of gallstones Gallstones Cholelithiasis (gallstones) is the presence of stones in the gallbladder. Most gallstones are cholesterol stones, while the rest are composed of bilirubin (pigment stones) and other mixed components. Patients are commonly asymptomatic but may present with biliary colic (intermittent pain in the right upper quadrant). Cholelithiasis in the gallbladder Gallbladder The gallbladder is a pear-shaped sac, located directly beneath the liver, that sits on top of the superior part of the duodenum. The primary functions of the gallbladder include concentrating and storing up to 50 mL of bile. Gallbladder and Biliary Tract: Anatomy | Asymptomatic or biliary colic (constant, dull RUQ pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways lasting < 6 hours) |
|
|
| Cholecystitis Cholecystitis Cholecystitis is the inflammation of the gallbladder (GB) usually caused by the obstruction of the cystic duct (acute cholecystitis). Mechanical irritation by gallstones can also produce chronic GB inflammation. Cholecystitis is one of the most common complications of cholelithiasis but inflammation without gallstones can occur in a minority of patients. Cholecystitis | Cystic Cystic Fibrocystic Change duct obstruction with inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation of the gallbladder Gallbladder The gallbladder is a pear-shaped sac, located directly beneath the liver, that sits on top of the superior part of the duodenum. The primary functions of the gallbladder include concentrating and storing up to 50 mL of bile. Gallbladder and Biliary Tract: Anatomy | Constant RUQ pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways (> 6 hours), fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever, nausea Nausea An unpleasant sensation in the stomach usually accompanied by the urge to vomit. Common causes are early pregnancy, sea and motion sickness, emotional stress, intense pain, food poisoning, and various enteroviruses. Antiemetics and vomiting Vomiting The forcible expulsion of the contents of the stomach through the mouth. Hypokalemia, Murphy’s sign |
|
|
| Choledocholithiasis Choledocholithiasis Presence or formation of gallstones in the common bile duct. Cholelithiasis | CBD CBD Atypical Parkinsonian Syndromes obstruction due to a stone | Postprandial colicky RUQ pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways > 6 h, jaundice Jaundice Jaundice is the abnormal yellowing of the skin and/or sclera caused by the accumulation of bilirubin. Hyperbilirubinemia is caused by either an increase in bilirubin production or a decrease in the hepatic uptake, conjugation, or excretion of bilirubin. Jaundice |
|
ERCP ERCP Fiberoptic endoscopy designed for duodenal observation and cannulation of vater’s ampulla, in order to visualize the pancreatic and biliary duct system by retrograde injection of contrast media. Endoscopic (vater) papillotomy may be performed during this procedure. Primary Sclerosing Cholangitis and cholecystectomy Cholecystectomy Cholecystectomy is a surgical procedure performed with the goal of resecting and extracting the gallbladder. It is one of the most common abdominal surgeries performed in the Western world. Cholecystectomy is performed for symptomatic cholelithiasis, cholecystitis, gallbladder polyps > 0.5 cm, porcelain gallbladder, choledocholithiasis and gallstone pancreatitis, and rarely, for gallbladder cancer. Cholecystectomy |
| Acute cholangitis Acute Cholangitis Acute cholangitis is a life-threatening condition characterized by fever, jaundice, and abdominal pain which develops as a result of stasis and infection of the biliary tract. Septic shock, liver abscess, and multi-organ dysfunction are potential serious complications. Acute Cholangitis | Bile Bile An emulsifying agent produced in the liver and secreted into the duodenum. Its composition includes bile acids and salts; cholesterol; and electrolytes. It aids digestion of fats in the duodenum. Gallbladder and Biliary Tract: Anatomy duct infection | RUQ pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways, fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever, jaundice Jaundice Jaundice is the abnormal yellowing of the skin and/or sclera caused by the accumulation of bilirubin. Hyperbilirubinemia is caused by either an increase in bilirubin production or a decrease in the hepatic uptake, conjugation, or excretion of bilirubin. Jaundice, hypotension Hypotension Hypotension is defined as low blood pressure, specifically < 90/60 mm Hg, and is most commonly a physiologic response. Hypotension may be mild, serious, or life threatening, depending on the cause. Hypotension, tachycardia Tachycardia Abnormally rapid heartbeat, usually with a heart rate above 100 beats per minute for adults. Tachycardia accompanied by disturbance in the cardiac depolarization (cardiac arrhythmia) is called tachyarrhythmia. Sepsis in Children |
|
|
Other potential diagnoses to consider:
Diagnosis Codes:
This code is used to diagnose
acute cholangitis
Acute Cholangitis
Acute cholangitis is a life-threatening condition characterized by fever, jaundice, and abdominal pain which develops as a result of stasis and infection of the biliary tract. Septic shock, liver abscess, and multi-organ dysfunction are potential serious complications.
Acute Cholangitis, a life-threatening bacterial infection of the
bile
Bile
An emulsifying agent produced in the liver and secreted into the duodenum. Its composition includes bile acids and salts; cholesterol; and electrolytes. It aids digestion of fats in the duodenum.
Gallbladder and Biliary Tract: Anatomy ducts, which is typically caused by a blockage from a gallstone.
| Coding System | Code | Description |
|---|---|---|
| ICD-10-CM | K83.09 | Other cholangitis |
| SNOMED CT | 87789006 | Cholangitis (disorder) |
Procedures/Interventions:
This code is for an
Endoscopic Retrograde Cholangiopancreatography
Endoscopic Retrograde Cholangiopancreatography
Fiberoptic endoscopy designed for duodenal observation and cannulation of Vater’s ampulla, in order to visualize the pancreatic and biliary duct system by retrograde injection of contrast media. Endoscopic (Vater) papillotomy may be performed during this procedure.
Primary Sclerosing Cholangitis (
ERCP
ERCP
Fiberoptic endoscopy designed for duodenal observation and cannulation of vater’s ampulla, in order to visualize the pancreatic and biliary duct system by retrograde injection of contrast media. Endoscopic (vater) papillotomy may be performed during this procedure.
Primary Sclerosing Cholangitis), which is both the diagnostic and therapeutic procedure of choice. It is used to decompress the
biliary tree
Biliary tree
The bile ducts and the gallbladder.
Gallbladder and Biliary Tract: Anatomy by removing the obstructing stone or placing a stent.
| Coding System | Code | Description |
|---|---|---|
| CPT | 43264 | Endoscopic retrograde cholangiopancreatography Endoscopic Retrograde Cholangiopancreatography Fiberoptic endoscopy designed for duodenal observation and cannulation of Vater’s ampulla, in order to visualize the pancreatic and biliary duct system by retrograde injection of contrast media. Endoscopic (Vater) papillotomy may be performed during this procedure. Primary Sclerosing Cholangitis ( ERCP ERCP Fiberoptic endoscopy designed for duodenal observation and cannulation of vater’s ampulla, in order to visualize the pancreatic and biliary duct system by retrograde injection of contrast media. Endoscopic (vater) papillotomy may be performed during this procedure. Primary Sclerosing Cholangitis); with endoscopic retrograde removal of calculus/calculi from biliary and/or pancreatic duct(s) |
Complications:
This code is for
sepsis
Sepsis
Systemic inflammatory response syndrome with a proven or suspected infectious etiology. When sepsis is associated with organ dysfunction distant from the site of infection, it is called severe sepsis. When sepsis is accompanied by hypotension despite adequate fluid infusion, it is called septic shock.
Sepsis and Septic Shock, a common and life-threatening complication of
acute cholangitis
Acute Cholangitis
Acute cholangitis is a life-threatening condition characterized by fever, jaundice, and abdominal pain which develops as a result of stasis and infection of the biliary tract. Septic shock, liver abscess, and multi-organ dysfunction are potential serious complications.
Acute Cholangitis, resulting from the biliary infection spreading into the bloodstream.
| Coding System | Code | Description |
|---|---|---|
| ICD-10-CM | A41.9 | Sepsis Sepsis Systemic inflammatory response syndrome with a proven or suspected infectious etiology. When sepsis is associated with organ dysfunction distant from the site of infection, it is called severe sepsis. When sepsis is accompanied by hypotension despite adequate fluid infusion, it is called septic shock. Sepsis and Septic Shock, unspecified organism |