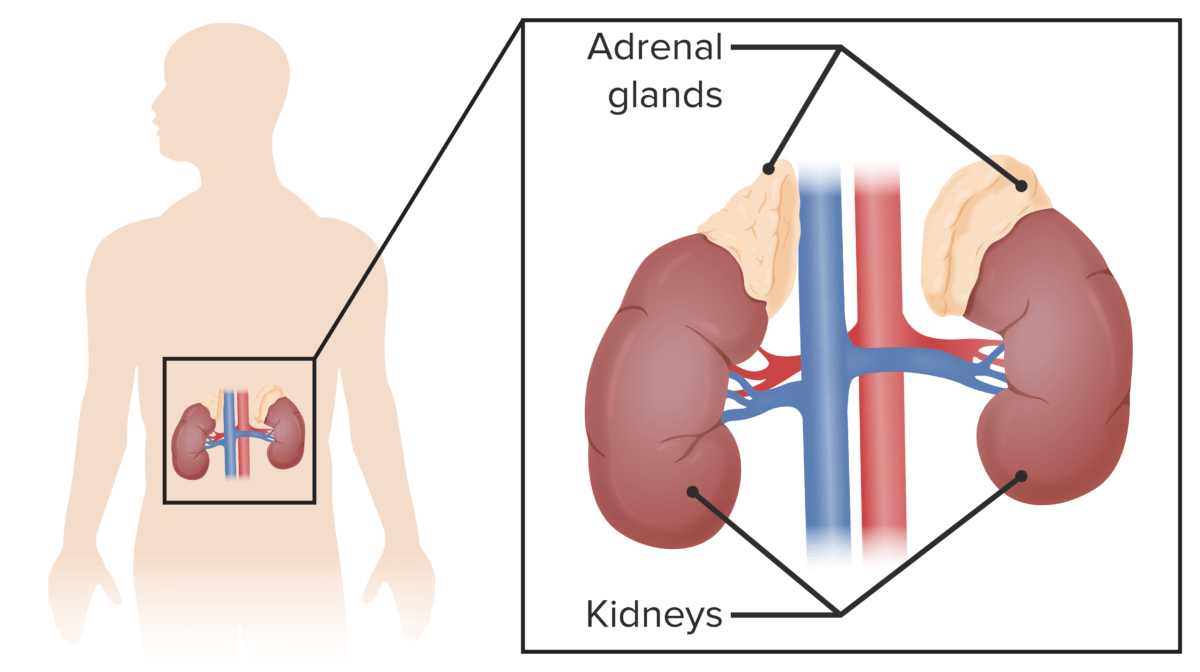
LFS is known as the sarcoma, breast, leukemia, and adrenal gland (SBLA) cancer syndrome due to its propensity for these cancer types. Those affected are also at increased risk of melanomas, Wilms’ tumors, and other gastrointestinal and reproductive cancers.
For USMLE Step 1, it is essential to understand the genetic basis of LFS, its inheritance pattern, the typical clinical presentation and diagnosis, and cancer risks and patient surveillance. Reviewing these topics will prepare you for any test question about LFS thrown your way on test day!
Genetic Basis
LFS is caused by mutations in a gene called TP53, which encodes the p53 tumor suppressor protein. This protein regulates the cell cycle and prevents mutations that may lead to cancer.
There are three genes identified with LFS: TP53, 17p13, 1q23, and checkpoint kinase two genes (CHEK2). CHEK2 is also a tumor suppressor gene. Mutations in the TP53 gene are the most common, with about 70% of affected families having a mutation of this gene.
The TP53 gene follows the two-hit hypothesis, which states that mutations in both gene copies are required to develop the disease. Individuals with LFS are born with one abnormal copy of the TP53 gene. The disease then develops when a spontaneous mutation occurs in the other copy of the gene, leading to the loss of function of the P53 protein. This mutation is most likely to occur in breast, bone, or muscle tissue cells.
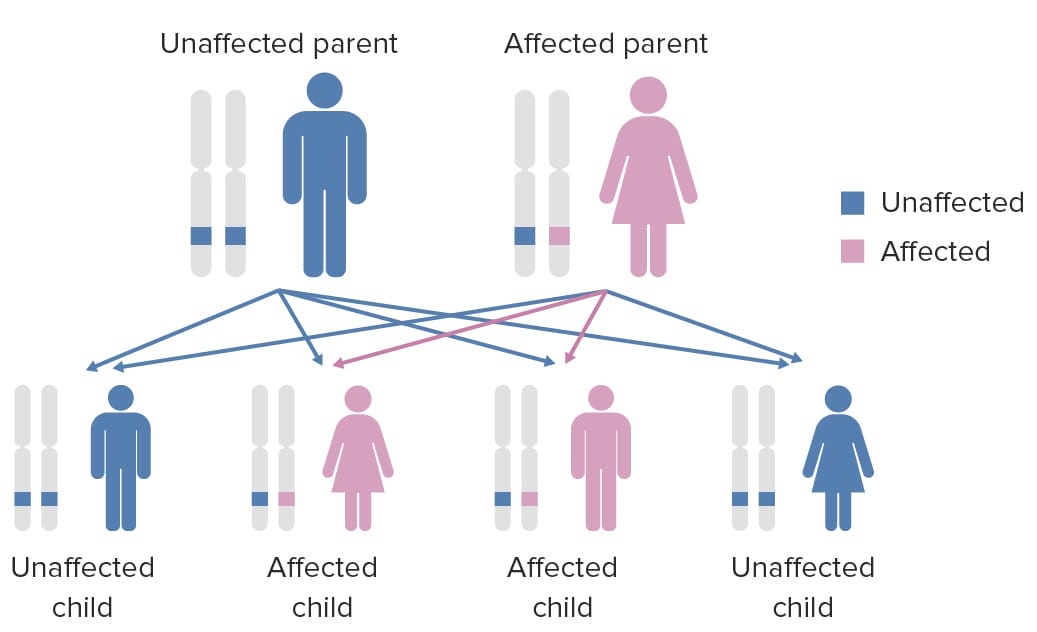
Inheritance Pattern
LFS is an autosomal dominant inherited disorder. Most individuals will inherit a mutated copy of the TP53 gene on the 17p3.1 chromosome from a parent affected by the syndrome. Most commonly, this is a missense mutation in exons 5 and 8.
In 7–20% of LFS cases, the mutated gene results from a de novo mutation in the gene that occurred during oogenesis, spermatogenesis, or early in development. Regardless of whether the mutation is inherited or de novo, there is a 50% chance of passing the disease to children.
Clinical Presentation
Initially, the diagnosis of LFS was done using clinical criteria based on signs and symptoms, but with the development of advanced genetic testing, patients can now know if they carry a copy of the TP53 mutation before signs or symptoms become apparent. Genetic testing is crucial for early detection and cancer prevention. If a patient tests positive, the patient must be counseled about surveillance and continuously screened for LFS-related types of cancer.
Common signs and symptoms of the most prevalent cancers include:
- Sarcomas: painless mass, enlarging and potentially compressing surrounding structures
- Leukemia: pancytopenia, fatigue, fever, weight loss, loss of appetite, swollen lymph nodes, bleeding gums, and increased rate of infections
- Osteosarcomas: localized pain, soft tissue mass tender to palpation, common in long bones
- Breast cancer: breast mass or lump
- Brain tumors: neurological features such as seizures, vomiting, headaches, and gait changes
- Adrenocortical carcinomas: mass in the abdomen or virilization, including prepubertal genital hair, increased penile size, clitoromegaly, or deep voice
Diagnostic Criteria
LFS is diagnosed based on genetic conformational testing. Additionally, LFS may be suspected when lab results reveal increased hormonal levels. This includes increased levels of adrenocortical carcinoma and increased alkaline phosphatase in osteosarcoma.
There are two sets of diagnostic criteria to be aware of.
#1 Classic Li-Fraumeni syndrome
Classic Li-Fraumeni syndrome is diagnosed when individuals meet all of the following criteria:
- Sarcoma is diagnosed before 45 years old.
- First-degree-relative, parent, sibling, or child with any cancer before 45 years old
- Any cancer before 45 years old or a sarcoma at any age in a first-degree or second-degree relative (grandparent, aunt/uncle, niece/nephew, or grandchild)
#2 Chompret criteria
Consider LFS diagnosis in anyone with a personal and family history that meets one of the following criteria. This is less likely to be tested on USMLE examinations, but it is crucial to understand to identify potential LFS impacted individuals on test day and clinically in practice.
- Tumor in the LFS variance before 46 years old. This includes premenopausal breast cancer, soft tissue sarcoma, osteosarcoma, adrenal cortical tumor, brain tumor, leukemia, lung cancer, AND at least one first or second-degree relative who has an LFS tumor before 56 years old or numerous tumors, except for breast cancer.
- An individual has multiple tumors, except when two belong to the LFS tumor spectrum before 46 years old.
- An individual who is diagnosed with adrenocortical carcinoma or choroid plexus tumor, regardless of family history.
Li-Fraumeni-like syndrome
Li-Fraumeni-like syndrome (LFL) is another set of criteria used to diagnose families who do not meet the classic LFS criteria but still have an increased risk of developing cancer. This includes:
- An individual diagnosed with any brain tumor, adrenocortical tumor, or breast cancer before 45 years old AND
- A typical LFS cancer in a first or second-degree relative at any age AND
- A first-degree or second-degree relative with any cancer before 60 years old.
Cancer Risk
Individuals with LFS have a significantly higher risk of developing multiple primary cancers throughout their lifetime. Specific cancer risks vary depending on the individual and their family history, but early detection and surveillance are crucial for optimal management.
Surveillance is an integral part of care for individuals who are at risk based on the history of LFS.
Surveillance includes:
- Annual physical examination and medical evaluation should be performed for unexplained symptoms
- Whole body MRI
- Abdominal and pelvic ultrasound
- Biochemical markers for adrenocortical function
- Blood tests (CBC, lactate dehydrogenase, and erythrocyte sedimentation rate) every four months
- Breast cancer monitoring via breast self-examination, clinical breast evaluation, and annual breast imaging
- Colonoscopy
Main Takeaways
LFS is a rare hereditary cancer syndrome with an autosomal dominant inheritance pattern. It is also known as the sarcoma, breast, leukemia, and adrenal gland (SBLA) cancer syndrome. It is most commonly caused by mutations in the TP53 gene, affecting the functioning of the p53 tumor suppressor protein. This disease is characterized by an increased risk of developing a wide range of cancers from a young age. Individuals with a family history of LFS should undergo genetic testing to allow for appropriate surveillance and monitoring throughout their lifetime.
By understanding the main takeaways from this review, you should be prepared for any questions about LPS on test day and easily tackle them!