I’m sure many of us have seen medical dramas. Because of that, we have preconceptions about EM. Whether these are true or false, I suggest entering this subject with your mind open because it’s nothing like what you see on TV.
If there were a show about what truly happens in the emergency room (ER), it would get horrible ratings because it mostly consists of paperwork.
So, forget all that stuff about patients leaving the ER minutes after they’re attached to an IV bag. Forget the parts where patients walk out of an ER following a severe accident. Most importantly, forget the scenes where they show characters doing CPR. Let’s remove these expectations and start with defining EM.
What is Emergency Medicine?
Emergency medicine focuses on the diagnosis and treatment of unforeseen illnesses or injuries.
Each medical specialty is a unique experience. In pediatrics, you deal with children. In surgery, you deal with operations. As such, your experience in EM will be different. In EM, you’re working with a whole triage of patients continuously.
If you’ve ever been to an ER, you’ll see a whole system there. Patients come in, are assessed, and then categorized depending on the severity of their symptoms. Patients are then seen by emergency care physicians and treated. Then, the doctors refer them to respective specialties for more advanced care. All this happens in (ideally) a short period. Patients flow in, and the process cycles while hospitals aim for the most efficient flow time. Some operational management concepts are also involved.
Take the Course: Emergency Medicine
Dr. Jung and Dr. Bord from Johns Hopkins University will walk you through all relevant Emergency Medicine topics with clinical example cases, in-depth explanations of emergencies, and clear guidance on stabilizing critical patients.
What Makes Emergency Medicine Hard to Study?
Studying in a classroom is hard because you don’t necessarily see the processes taught. How do you know a patient is an emergent case? What symptoms does a patient with an acute abdomen manifest? Where do all these machines and equipment come from, and how long does it take to procure them? How fast does a patient really get treated in the ER?
In the ER, a patient coming in could lose their life in a few minutes if you don’t act fast. That’s not something easy to learn in a classroom.
So, you must become more creative when you’re studying EM for class. Of course, once you get to your ER rotation, it’s a whole different thing, but that doesn’t mean you can’t prepare yourself for it. If you want help with it, take the emergency medicine online course to get guidance and check out the tips below.
Tips for Emergency Medicine
#1: Know your basics and know them well
Since this is a clinical subject, there are basic lessons and skills you must learn. Unlike more general subjects, EM doesn’t necessarily need you to review all your basics. Rather, it only requires some basics you must know by heart. Why? Because in the field, you don’t have the luxury of time to check your reference materials.
So which subjects should you review? Of course, they should be the most common cases you see in the ER. These cases include:
- Shock,
- Trauma
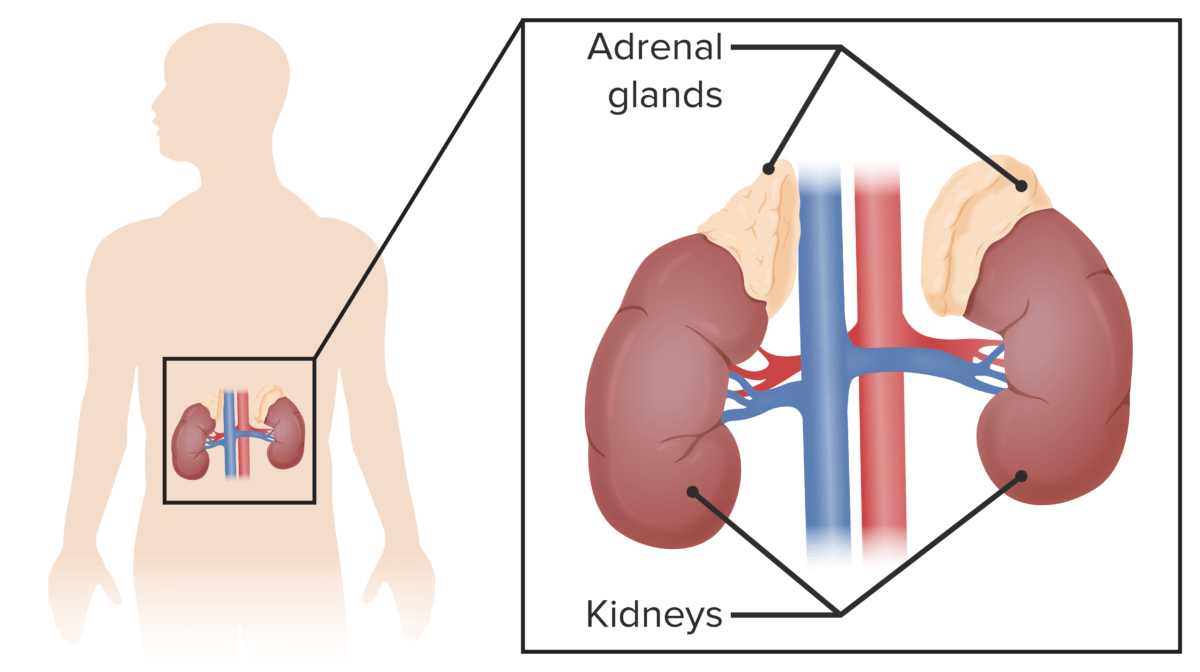
- Acute emergencies in each body system
- Electrolyte imbalances
The subject that I find of particular importance is pharmacology. You often don’t have time to search for the proper medications and their doses (although if you’re ever unsure, please double check). Plus, you’ll need a lot of toxicology expertise.
#2: Watch videos
Since it’s hard to picture what happens in an ER, the next best thing is watching videos. You could probably get away with doing intubation based on written instructions. But that’s hard to do, and failure is not something you want to risk in an emergency. It’s also hard to understand the treatment protocols in the ER without actually seeing them. We have systems we activate for things like a heart attack, stroke, hypertensive crisis, etc.
There are many videos online that show you the steps the team performs to treat common emergencies. Although other countries may have different standards, it still helps to visualize the steps of managing any acute disease.
Related videos
#3: Master the flowcharts
What makes EM stand out is how often it uses algorithms. If you look at the walls of the ER or the crash carts, you might see these as flowcharts to avoid any unnecessary errors on the part of the medical team. As you study them, note how much time it should take to finish each step.
Algorithms are easy to understand because they’re visually stimulating, and websites make them accessible. So, if you’re having trouble visualizing the next steps in patient diagnosis and treatment, master these pathways. These algorithms helped me in this subject, and they’re so much easier to learn than simply reading them in a wordy paragraph.
#4: Mnemonics are your best friend
Mnemonics are usually hard to remember, but not in EM. That’s because you’ll use these mnemonics repeatedly until you remember them. You have ABCDE, which means Airway, Breathing, Circulation, Disability, and Exposure. You have AMPLE, the questions you ask in your Secondary Assessment. Apart from these, there are many other mnemonics. I’ve used these mnemonics so often that they’re second nature. Remember these because they often ask these mnemonics in exams.
Also, since you need to recall information quickly in the emergency room, mnemonics are the easiest way to do it. But be careful when using these! I’ve gotten mnemonics mixed up with the proper names all the time. For example, I would refer to the Alvarado Scoring as MANTRELS, which got a few laughs from my colleagues, but it will cost you a point in your exams.
Studying medicine has never been easier.
Set yourself up for success with Lecturio.
Surviving Emergency Medicine Rotations
Rotations are where you apply what you learn from the classroom. In the field, it’s a different ballgame. Lives will be on the line, and while you’re a student, you still play a role. Like any rotation, you have to move efficiently and carefully. Anything can go wrong in a few seconds for critical patients. In the ER, in particular, you can actually get yelled at for doing nothing.
#1: Come in well-rested
We have a firm rule in EM: Never have a tired doctor working.
Being tired can cause more negative outcomes. This is bad, especially when doctors are more prone to making mistakes in stressful and fast-paced environments. My consultant used to say that a critical patient’s condition can worsen because of a single deranged factor, no matter how small. In other words, any mistake could push the patient’s condition over the edge.
Not just that, like any service job, you have to be efficient. My hospital used to notify us when a patient stayed in the ER past the expected time, meaning we weren’t working fast enough. More patients will be coming in, and they will need the beds of those who could have long been discharged or admitted to other services. So, believe me—you’ll need the energy. It’s important to note that despite knowing the necessity of self-care and the stressors of the job, ER doctors are still the most burnt-out specialists in medicine. So remember to take it easy and rest before your rotation!
#2: Always be moving
As I said, it’s one of the most fast-paced specialties out there. You must keep moving. My first ER patient had an ongoing seizure. Instead of helping, I froze. I didn’t know what to do. I didn’t know that one of the first things you do is ensure the patient has a patent airway. My lack of preparation left me feeling inadequate, and I got a good scolding from my superior.
Don’t be afraid to ask what you can do to help. All the doctors I’ve worked for in the ER appreciate people with initiative. You’re part of the team now, and everyone needs to work together. It doesn’t make sense for anyone to leave you in the dark about your role in the ER. Also, be prepared. Read up on the most common cases and their management so that when they do come up, you can help.
#3: If you don’t know what to do, get out of the way
Of course, there will be times when you don’t know what to do. That’s perfectly normal. For those cases, it’s enough to step back and watch—just don’t get in the way. Blocking the way of the healthcare team will delay life-saving treatment for emergency patients. Sometimes students unintentionally block the crash cart and get yelled at for it. So find a comfy spot in the corner and let the team do their thing.
You can also handle other tasks while the team works on cases in which you won’t participate. While the doctors are busy with a critical patient, if you’re not doing anything there, you can help manage other patients in the ER so that the workflow doesn’t stagnate.
#4: Master taking a patient history and doing a physical exam
Your main job, and the biggest expectation of you in the ER, is your history taking and physical exam skills –— and how fast you can do it. In the ER, you need to be efficient. You need to get as much information as possible from the patient without taking too much time.
In other words, you need to master it. Sure, by the end of your rotation, you’ll probably master these skills. But don’t wait for the end of the rotation to do a good job. Search how to perform secondary surveys and what questions to ask for common chief complaints. Once you hear their chief complaint, you should already have a list of differentials on your mind, then use the interview and PE to rule them in or out.
#5: Prioritize the deadliest diagnoses
Usually, once you have your list of differentials, you want to rule out the least likely ones first. In the ER, however, you want to rule out the most deadly ones. Why? People show up to the ER when their symptoms are at their worst. Even worse, those symptoms can point to many things. Chest pain can mean a heart attack. Abdominal pain can point to a ruptured appendix. A headache can be a sign of a stroke.
Many patients believe the diagnostics that doctors run in the ER seem excessive. Well, that’s because they are excessive, but with good reason! I once had a patient who thought he came in for gastroesophageal reflux disease (GERD), but when we ran him through the electrocardiogram, it turns out he had an ST elevation myocardial infarction. In other words, if we had overlooked his chest pain as GERD and then sent him home, he’d be back in cardiogenic shock, or worse — he’d die at home from fatal arrhythmia. So, always be on your toes and suspect everything.
In the ER, it’s better safe than sorry.
#6: Enjoy it and be kind
The ER can be stressful and tiring. But of all my rotations, there hasn’t been anything like the ER.
I’m not telling you to have fun while doing CPR on a patient. Instead, prepare yourself for the worst, and take everything in stride.
Whatever mistakes you make, learn from them. Whatever things you do right, keep doing them. Take comfort in the idea that you’re growing from the experience.
Be enthusiastic about helping patients. I know it’s tiring when you’re seeing patients left and right. Because of that, it’s easy to see patients in the ER as something similar to items on a checklist. So, look at it this way: for you, it’s Tuesday; for them, it’s the worst day of their lives. You’re in a position to make this process as smooth and painless as possible. In the hectic environment of the ER, kindness can make a huge difference.