Playlist
Show Playlist
Hide Playlist
Pancreatic Cancer
-
Slides Pancreas and Biliary Tract.pdf
-
Download Lecture Overview
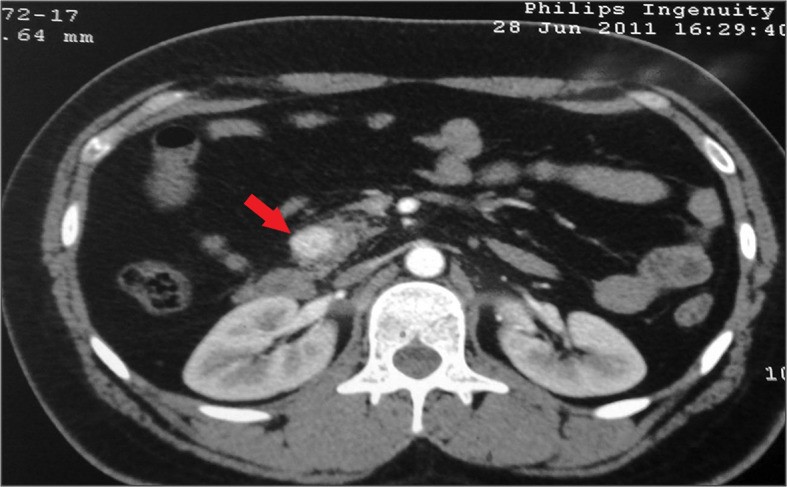
00:01 Pancreatic cancer. 00:02 Second most common GI cancer. 00:05 We have cancers such as primary gastric adenocarcinoma. 00:09 We have colorectal cancer, all being part of GI, and pancreatic cancer, second most common GI cancer. 00:16 When you say pancreatic cancer, here, we’re referring to adenocarcinoma of the pancreas. 00:21 Adenocarcinoma. 00:23 Remember when it comes to the pancreas, you’ll be dividing it into an adenocarcinoma, and your Islet cell tumor cancers. 00:30 For example, most common, Islet cell tumor, a beta islet cell tumor, a benign cancer called insulinoma. 00:39 This is adenocarcinoma. 00:43 Risk factors. 00:45 Family history plays a big role. 00:46 Smoking plays a big role. 00:48 Molecularly, what kind of RAS is associated with pancreatic cancer? Good. 00:55 K-ras. 00:57 It is an adenocarcinoma. 01:00 Endocrine tumor. 01:02 A cystic tumor. 01:03 Or a lymphoma. All different types of pancreatic cancers. 01:08 Our focus in this section will be adenocarcinoma. 01:11 Remember the endocrine tumors; a beta Islet cell tumor, an alpha Islet cell tumor, a delta Islet cell tumor referring to insulinoma, glucagonoma, somatostatinoma that we’ve discussed all prior. 01:23 You could have cystic tumors, and perhaps even, lymphomas. 01:28 Clinical presentation of pancreatic cancer is what you would expect with pancreatitis. 01:34 Abdominal pain with the radiation to the back. 01:37 There is going to be weight loss, but you will also find this with chronic pancreatitis. 01:43 If it’s adenocarcinoma, which actually for you, would be more found or located in the head of the pancreas. 01:51 Please put the head of the pancreas and jaundice manifestation together. 01:56 The head of the pancreas is nestled within the second part of the duodenum. 02:02 If you go on to develop an adenocarcinoma of the head, as it enlarges, it is then going to cause obstruction in the area of the intestine. 02:12 What happens now? Obstruction. 02:14 You cannot properly dump out your bile into the second part of the duodenum. 02:19 This is an obstructive type of jaundice. 02:25 Courvoisier's sign is the name, but what it means is the fact that the gallbladder may be palpable, which is rather interesting, isn’t it? The gallbladder which is behind the liver ends up -- You find a description where upon physical examination, it’s palpable, high on the differential at that point should be some kind of GI cancer. 02:45 Clinical presentation continues and now we have something called Trousseau Syndrome. 02:50 And those of you that have memorized Trousseau sign, meaning to say your Chvostek sign or something like your carpopedal spasms after placing a blood pressure cuff This is not that. 03:05 This is a Trousseau syndrome, and what this means is you’re a migratory type of thrombosis. 03:11 A venous thrombosis that you would find. 03:13 This is called Trousseau’s syndrome. 03:16 Also, there might be variceal hemorrhage from portal hypertension. 03:20 Remember, with pancreatic cancer, there’s every possibility that you might have portal hypertension. 03:26 And with all of this, sequelae of portal hypertension, it’s the variceal hemorrhage that you’re worried about the most. 03:33 And with enough damage that’s taken place to pancreas at some point in time, you’re expect there to be glucose intolerance due to decreased insulin release. 03:43 Important. Important clinical presentations for pancreatic cancer. 03:48 And why? Specifically is because you cannot afford to get this confused with chronic pancreatitis in which weight loss could also be found, also with hypoglycemia. 03:59 But these others things such as your Trousseau syndrome and such, mm-mm. 04:06 Pancreatic cancer and our evaluation of it. 04:09 How do we diagnose it? You’re going to be looking for CA 19-9. 04:14 Serum levels of a CA 19-9 have a high sensitivity and specificity for patients presenting with classic symptoms of a GI malignancy. 04:22 But there are poor screening test, when used in the general population. 04:25 For example you can see non-specific elevations in patients that present with obstructive jaundice for elated the gallstones. 04:32 Remember, they are going to give you a number of signs and symptoms so that it points you towards pancreatic cancer. 04:39 They will give you CA 19-9. 04:41 And at that point, you should be thinking about pancreatic cancer. 04:44 No doubt. 04:46 Radiologically, what are you going to find? Well, you do a high resolution CT with pancreatic protocol used for staging, staging, staging when it comes to pancreatic cancer. 04:57 You wouldn’t find such a thing as your pseudocyst and such. 05:00 A pseudocyst is something that you would find with pancreatitis more notably with chronic pancreatitis. 05:09 Your endoscopic ultrasound. 05:11 What are you going to find? What are you looking for? So at this point, you are suspecting pancreatic cancer. 05:16 Why? Well, because there is glucose intolerance, there is jaundice in your patient, and you end up finding a marker for CA19-9. 05:24 Exploration. 05:25 Ultrasound. 05:26 Localization of the tumor and staging, endoscopic ultrasound. 05:31 The ERCP becomes important for therapeutic stenting for obstructive jaundice. 05:36 Okay? So even to this day, as far as you’re concerned, you’re going to use ERCP at certain times, especially because if you want to open up things, to explore for certain pathologies and understand that this might actually cause damage as well, referring to the fact that earlier, a cause of pancreatitis was in fact ERCP. 05:57 Management. 05:58 Surgery, only curative option. 06:01 Steve Jobs from Apple died of pancreatic cancer. 06:05 It is extremely aggressive. 06:07 And even with surgery, there is no guarantee that the patient is going to live. 06:13 A five-year survival rate remains very poor even after surgery. 06:18 And, let me bring up a basic concept that we talked about in our discussion of neoplasia. 06:24 And at the time, I told you that adenocarcinoma is involved with a particular type of change around the cancer that gives it a fibrous type of consistency. 06:38 What’s that called? Desmoplasia. 06:41 Interesting phenomenon, isn’t it? You could find that with pancreatic cancer big time. 06:47 Palliation: Endoscopic or percutaneous stent. 06:51 What are you trying to do? You’re trying to open up perhaps a blocked duct, chemotherapy with a drug called gemcitabine, and pain control with the celiac nerve block, if at all, effective.
About the Lecture
The lecture Pancreatic Cancer by Carlo Raj, MD is from the course Pancreatic and Biliary Tract Diseases: Basic Principles with Carlo Raj.
Included Quiz Questions
Which of the following is NOT a risk factor for pancreatic adenocarcinoma?
- Acute pancreatitis
- Family history
- Smoking
- Hereditary genetic mutations
- Older age
Which oncogene is primarily associated with pancreatic adenocarcinoma?
- K-ras
- p53
- PTEN
- C-kit
- Raf kinase
Which of the following is NOT classified as an exocrine tumor of the pancreas?
- Islet cell tumor
- Pancreatic adenocarcinoma
- Cystic tumors of the pancreas
- Lymphoma
- Papillary neoplasms
Which of the following is NOT a sign or symptom of pancreatic adenocarcinoma?
- Asterixis
- Jaundice
- Weight loss
- Pain radiating to the back
- A palpable gallbladder
Which of the following signs is associated with pancreatic adenocarcinoma?
- Courvoisier sign
- Cullen's sign
- Murphy's sign
- Trousseau sign
- Chvostek's sign
Which paraneoplastic syndrome is associated with pancreatic adenocarcinoma?
- Migratory thrombophlebitis
- Hypercalcemia
- Cortisol increase
- Polycythemia
- Acanthosis nigricans
Which tumor marker is associated with pancreatic adenocarcinoma?
- CA 19-9
- CA 125
- CEA
- CA 15-3
- CD 117
Which of the following is used for staging of pancreatic cancers?
- High-resolution CT scan with pancreatic protocol
- MRI scan with pancreatic protocol
- MRCP with pancreatic protocol
- Abdominal ultrasound scan with pancreatic protocol
- ERCP with pancreatic protocol
Which of the following is NOT considered palliative therapy for pancreatic cancer?
- Therapeutic embolization
- Pain control with celiac block
- Chemotherapy with gemcitabine
- Endoscopic or percutaneous stent
Which of the following statements is NOT true about pancreatic adenocarcinoma?
- ERCP is a curative option for pancreatic adenocarcinoma.
- Pancreatic adenocarcinoma is known to show a desmoplastic reaction around the tumor.
- The 5-year survival rate is poor for pancreatic adenocarcinoma.
- Endoscopic ultrasound is used for localizing the tumor and staging.
- Therapeutic stenting relieves the obstructive jaundice in cases of pancreatic adenocarcinoma.
Which of the following is a common site for endocrine pancreatic tumors?
- Tail of the pancreas
- Head of the pancreas
- Body of the pancreas
- Ductal system of the pancreas
- Ampulla of Vater
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Excellently explained everything. I was looking for alternative to Kaplan and I think this is it.