Playlist
Show Playlist
Hide Playlist
Genital Herpes: Signs, Symptoms & Diagnosis
-
Slides GenitalHerpes InfectiousDiseases.pdf
-
Reference List Infectious Diseases.pdf
-
Download Lecture Overview
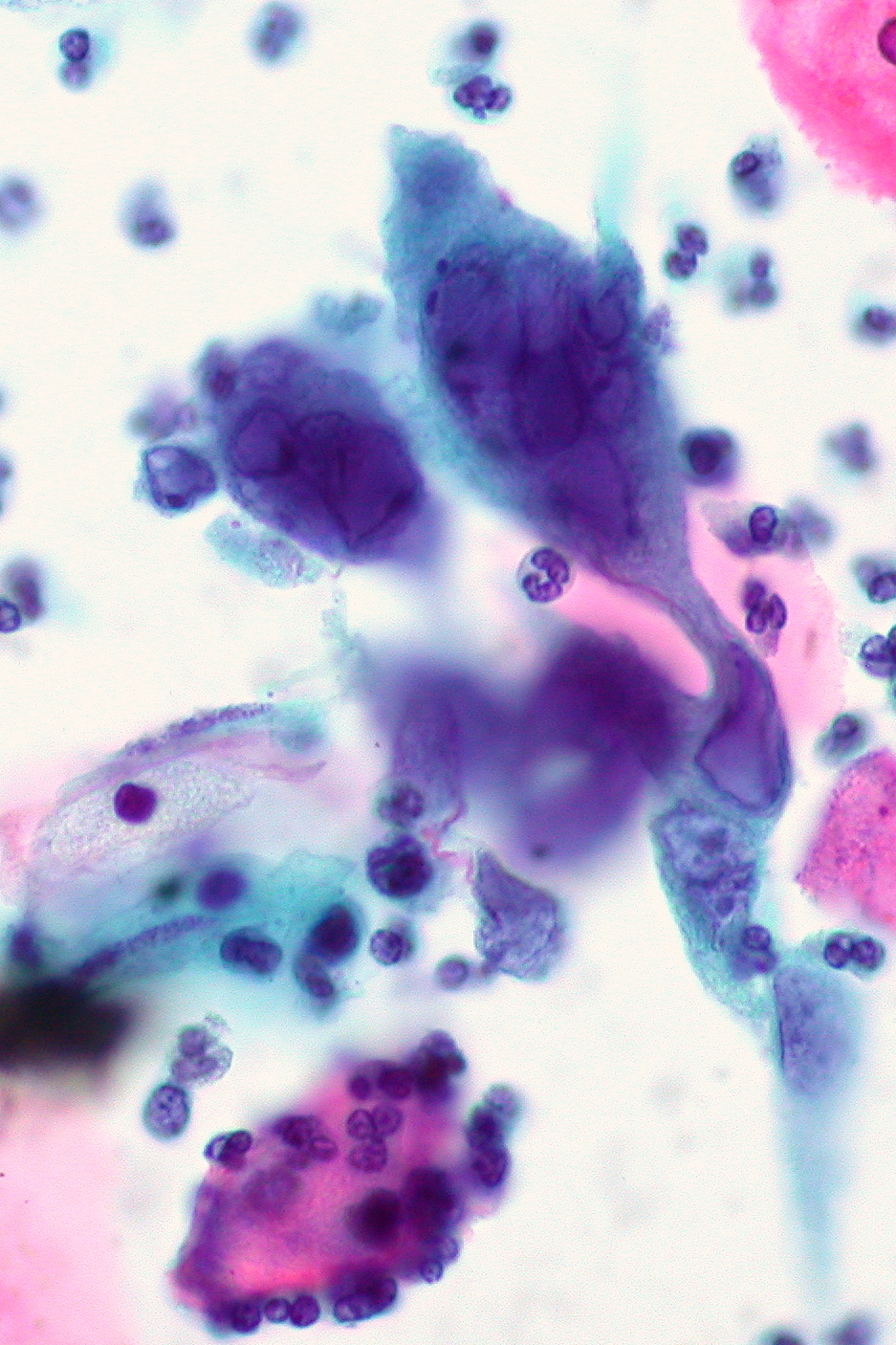
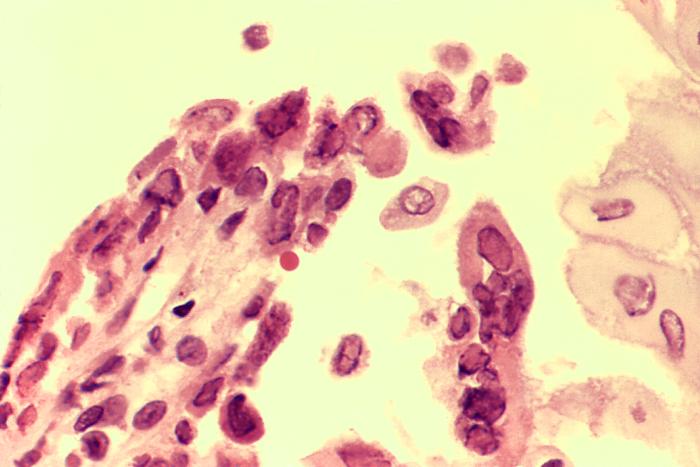
00:01 So the clinical features are pretty well known. 00:05 And most physicians and medical students have seen this infection. 00:11 It usually starts out with systemic symptoms like fever, headache, malaise, and myalgias, and then widely spaced bilateral lesions in the external genitalia in the form of vesicles, which then become pustules, and then painful – and I mean painful – erythematous ulcers which eventually crust over pretty much like a fever blister on the upper lip. 00:42 Recurrent infection, however, the duration of the recurrences is shorter. 00:50 In other words, its symptoms don’t last as long, there are not as many vesicles, and initially, a person might have 4 to 5 episodes per year. 01:01 But over several years, there is a decrease in the number of episodes. 01:08 Before each of these episodes, there may be some mild tingling 1 to 5 days before the eruption of new vesicles. 01:19 There maybe shooting pains in the buttocks, legs, and hips, which reflect the nerve root involvement. 01:28 And then 20 percent of patients, that’s all you get. 01:31 You don’t get any lesions – maybe just localized pain and itching. 01:37 And the duration of the viral shedding is about 4 days. 01:43 This is a problem because there is asymptomatic viral shedding, especially in women from the cervix, vulva, anus, and urethra. 01:53 And in men, from the skin of the penis, the urethra, the anus, and the virus has even been found in semen. 02:03 Persons with a history of receptive anal intercourse may present with proctitis. 02:08 We certainly worry about infants who are born to infected mothers. 02:13 But actually, thankfully, relatively few infants are at risk. 02:20 And so, we only have to consider a C-section in women who are actively shedding virus at the time of delivery. 02:29 So if a woman who is about to deliver has visible lesions of herpes simplex, obviously, we would want to do a C-section. 02:42 But otherwise, only if we know that she is shedding virus. 02:50 So how do you make the diagnosis? Well, the clinical picture is so characteristic, it’s rarely mistaken for any other thing. 03:00 So they're characteristic multiple vesicles on an erythematous base and they’re tender. 03:07 We can isolate the virus in culture, but actually doing PCR in identifying herpes simplex virus DNA and scrapings of the lesions is 3 to 4 times more sensitive than doing a viral culture. 03:28 So you can culture it, but finding viral DNA is much more sensitive. 03:37 Now, not every situation has the ability to do PCR. 03:43 So for the physician that’s practicing and has the ability to use the microscope, staining of scrapings from the lesions, called a Tzanck preparation, is at least 70 percent sensitive in making the diagnosis of a herpes virus infection. 04:06 It doesn’t tell you whether it’s herpes simplex 1 or 2, or even varicella zoster, but this is what the Tzanck prep looks like. 04:18 And what you do is you some kind of cell stain on scrapings from the base of one of these vesicles or ulcers. 04:28 And the cell stain would be a Wright stain, which is, as a matter of fact, you can actually take a slide down to the hematology lab and run it through their automated Wright stainer, or you can do a rapid Giemsa stain, or as they do in PAP smears – you can use that form of stain to identify the evidence of a herpes infection. 04:56 What you’re looking for are these large cells that have many nuclei. 05:03 They’re called multi-nuclei giant cells, but they’re really not giant cells. 05:08 What’s happened is that several infected cells have lost their cell membrane and you’ve essentially got a bunch of nuclei that have sort of flowed into this bag that looks like a giant cell. 05:24 But it’s just a bunch of nuclei in what we call a syncytium.
About the Lecture
The lecture Genital Herpes: Signs, Symptoms & Diagnosis by John Fisher, MD is from the course Genital and Sexually Transmitted Infections. It contains the following chapters:
- Genital Herpes – Signs/Symptoms
- Genital Herpes – Diagnosis
Included Quiz Questions
Which of the following is NOT a typical clinical manifestation of primary herpes simplex virus infection?
- Blurred vision
- Tender lymphadenopathy
- Fever
- Headache
- Local pruritus
Which of the following is the classical lesion of herpes simplex virus?
- Painful vesicles on an erythematous base
- Beefy red friable ulcers with rolled up edges
- Non-tender well demarcated "cut-out" lesions
- Minute asymptomatic papules on the mucosal surfaces
- White pearly papules with central umbilication
Which of the following statements regarding clinical recurrences of herpes simplex virus (HSV) infection is MOST ACCURATE?
- Recurrence rates usually decrease over time.
- Recurrence rates usually increase over time.
- The likelihood of recurrence is much higher with HSV-1 infection.
- Recurrences are always notable as vesicular lesions at the site of primary infection.
- Clinical recurrences of genital HSV are rare.
Which of the following is the most sensitive diagnostic testing for herpes simplex virus infection?
- Real-time HSV polymerase chain reaction
- Viral culture
- Tzank smear
- Clinical signs and symptoms
- Serology
Which of the following is the most appropriate management of a pregnant woman who has presented in active labor and has active genital herpes simplex infection?
- Cesarean section
- Intravenous antiviral therapy
- A bolus dose of acyclovir and vaginal delivery
- Normal vaginal delivery
- Assisted vaginal delivery
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |